Global Neonatal & Children's Health
Category: Abstract Submission
Global Child and Adolescent Health I
146 - Should Mothers be Taught about Jaundice in Antenatal Clinics?
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 146
Publication Number: 146.111
Publication Number: 146.111
Richard P. Wennberg, University of Calfornia, Davis, Bothell, WA, United States; Stephen Oguche, University of Jos, Jos, Plateau, Nigeria; Zubaida L. Farouk, Bayero University Kano, Kano, Kano, Nigeria; Imam Zainab, Lagos State University Teaching Hospital, Ikeja, Lagos, Nigeria; Isa Abdulkadir, Ahmadu Bello University Teaching Hospital, Zaria Kaduna, Nigeria, Zaria, Kaduna, Nigeria
.jpg)
Richard P. Wennberg, MD
Owner, Research Director
Bilimetrix USA, LLC
Bothell, Washington, United States
Presenting Author(s)
Background: The World Health Organization provides a list of subjects to teach expectant mothers in antenatal clinics. Neonatal jaundice is not one of them. Verbal and/or printed instruction about jaundice is usually presented postpartum when mothers are faced with an overload of information along with emotional and physical adjustments. Retention is variable, and many mothers are unaware that jaundice may cause brain damage.
We recently provided evidence that instructing mothers about jaundice and its risks** increases early care seeking and decreases the incidence of kernicterus in Nigeria. This study reexamines these data focusing on when we should teach mothers about jaundice.
Objective: To compare the effectiveness of instructing mothers about jaundice following delivery (current standard) with instruction during antenatal clinic visits (with postpartum reinforcement) in reducing the incidence of acute bilirubin encephalopathy (ABE).
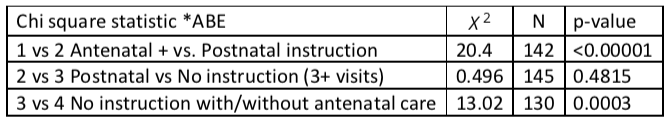
Design/Methods: We documented evidence of ABE among 272 newborns admitted to four tertiary care medical centers in Nigeria with serum bilirubin levels greater than 15 mg/dL, the accepted indication for phototherapy. Subjects were then assigned to four groups where 1) mothers had participated in an antenatal instruction session + post-delivery reinforcement, 2) mothers received instruction about jaundice but only following birth, 3) mothers had 3 or more antenatal visits but did not receive antenatal or postnatal instruction (not all clinics offered the program), 4) mothers had 0-2 clinic antenatal visits and did not receive jaundice instruction.
Results: The occurrence of ABE was lowest when mothers had received antenatal instruction and highest when mothers had no or minimal antenatal care. When mothers attended antenatal clinic regularly but did not receive antenatal jaundice instruction, adding postnatal training did not significantly reduce the incidence of ABE. The majority of antenatally trained mothers sought care because of jaundice while untrained mothers more often sought care because their babies were sick.Conclusion(s): Antenatal instruction coupled with postpartum reinforcement is more effective than postnatal education alone in promoting early care seeking and preventing ABE. WHO should consider adding jaundice instruction to prescribed antenatal maternal education, especially in countries such as Nigeria where kernicterus is a major preventable disease.
** Upgraded teaching materials used in this project can be found on the Stop Kernicterus International (SKI) website. https://skibilimetrixusa.azurewebsites.net
Instruction versus ABE.png)
Statistic
We recently provided evidence that instructing mothers about jaundice and its risks** increases early care seeking and decreases the incidence of kernicterus in Nigeria. This study reexamines these data focusing on when we should teach mothers about jaundice.
Objective: To compare the effectiveness of instructing mothers about jaundice following delivery (current standard) with instruction during antenatal clinic visits (with postpartum reinforcement) in reducing the incidence of acute bilirubin encephalopathy (ABE).
Design/Methods: We documented evidence of ABE among 272 newborns admitted to four tertiary care medical centers in Nigeria with serum bilirubin levels greater than 15 mg/dL, the accepted indication for phototherapy. Subjects were then assigned to four groups where 1) mothers had participated in an antenatal instruction session + post-delivery reinforcement, 2) mothers received instruction about jaundice but only following birth, 3) mothers had 3 or more antenatal visits but did not receive antenatal or postnatal instruction (not all clinics offered the program), 4) mothers had 0-2 clinic antenatal visits and did not receive jaundice instruction.
Results: The occurrence of ABE was lowest when mothers had received antenatal instruction and highest when mothers had no or minimal antenatal care. When mothers attended antenatal clinic regularly but did not receive antenatal jaundice instruction, adding postnatal training did not significantly reduce the incidence of ABE. The majority of antenatally trained mothers sought care because of jaundice while untrained mothers more often sought care because their babies were sick.Conclusion(s): Antenatal instruction coupled with postpartum reinforcement is more effective than postnatal education alone in promoting early care seeking and preventing ABE. WHO should consider adding jaundice instruction to prescribed antenatal maternal education, especially in countries such as Nigeria where kernicterus is a major preventable disease.
** Upgraded teaching materials used in this project can be found on the Stop Kernicterus International (SKI) website. https://skibilimetrixusa.azurewebsites.net
Instruction versus ABE
.png)
Statistic