Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine XIV
50 - Implementing Suicide Risk Factor Screening in a Pediatric Emergency Department
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 50
Publication Number: 50.407
Publication Number: 50.407
Rachel Cafferty, Children's Hospital Colorado, Denver, CO, United States; Irina Topoz, Children's Hospital Colorado, Denver, CO, United States; Maya Haasz, Children's Hospital Colorado, Aurora, CO, United States; Jan Leonard, University of Colorado Anschutz Medical Campus, Aurora, CO, United States; Lilliam Ambroggio, Children's Hospital Colorado, Aurora, CO, United States
.jpg)
Rachel Cafferty, MD (she/her/hers)
Assistant Professor
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Suicide is the second leading cause of death for adolescents. Identification of suicidal ideation and risk factors associated with a suicide attempt is an important first step in suicide prevention. The pediatric Emergency Department (ED) serves as a point of access for many adolescents without a primary care physician and is uniquely positioned to provide screening for suicide. However, documentation of suicide risk factors in the pediatric ED is poor.
Objective: To increase completion of a suicide risk factor survey for children screening at-risk on the Ask Suicide Screening Questions (ASQ) from 0% to 60% by August 31, 2021.
Design/Methods: Our institution routinely screens for suicide with the ASQ for all youth aged 10 years and older presenting to the ED. Providers secondarily perform a non-standardized risk assessment on patients with a positive ASQ. A multi-disciplinary team, including nurses and providers, participated in a Kaizen event. We created a process map of the current workflow and developed a survey of suicide risk factors unique to adolescents which underwent cognitive interviews with our institution’s youth advisory board prior to implementation. The primary outcome was percent of patient encounters in which a risk factor survey was completed. Rate of ED crisis evaluation was used as a process measure. ED length of stay (LOS) was the balancing measure. DMAIC methodology was used.
Results: Data from 1,711 patients are included. Prior to the study period, zero patients were screened using a standardized suicide risk assessment tool. During the study period, the percent of eligible patients who completed a comprehensive suicide risk survey went from 24.6% to 37.4%, with special cause variation detected (Figure 1). Rate of ED crisis evaluation decreased, with detection of special cause variation, from 11.4% baseline to 5.2% during the QI intervention period. Median LOS did not change over time (200.5 minutes (121.5-294.5 IQR) baseline, 213 minutes (135-324 IQR) during the QI intervention). Conclusion(s): Using QI methodology, we improved identification of suicide risk factors among youth in the ED and decreased ED crisis evaluation rates without impacting LOS. We were not able to meet the project aim of 60% survey completion. However, future improvement efforts will include utilization of technology to improve screening practices in our high-acuity and busy ED environment.
Proportion of Patients Screened for Suicide Risk Factors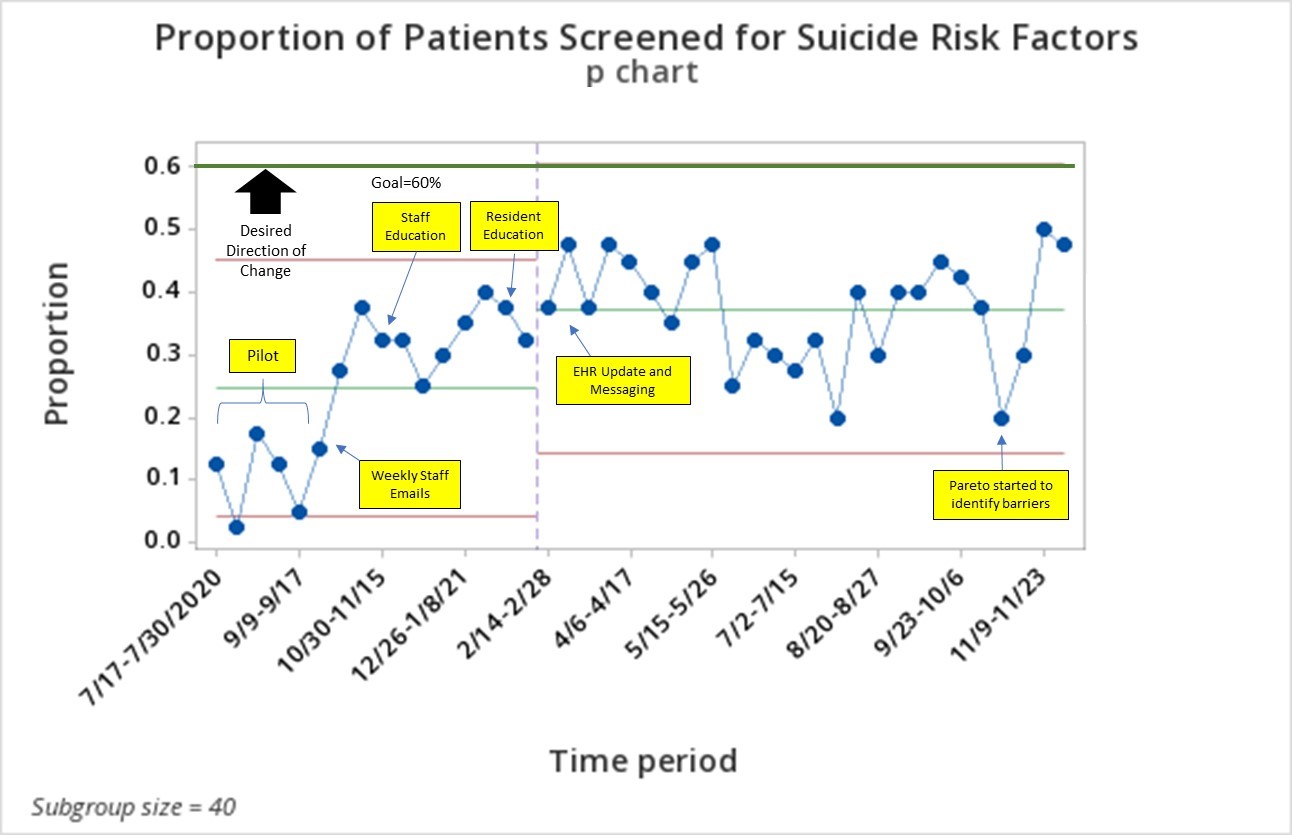 P Chart
P Chart
Objective: To increase completion of a suicide risk factor survey for children screening at-risk on the Ask Suicide Screening Questions (ASQ) from 0% to 60% by August 31, 2021.
Design/Methods: Our institution routinely screens for suicide with the ASQ for all youth aged 10 years and older presenting to the ED. Providers secondarily perform a non-standardized risk assessment on patients with a positive ASQ. A multi-disciplinary team, including nurses and providers, participated in a Kaizen event. We created a process map of the current workflow and developed a survey of suicide risk factors unique to adolescents which underwent cognitive interviews with our institution’s youth advisory board prior to implementation. The primary outcome was percent of patient encounters in which a risk factor survey was completed. Rate of ED crisis evaluation was used as a process measure. ED length of stay (LOS) was the balancing measure. DMAIC methodology was used.
Results: Data from 1,711 patients are included. Prior to the study period, zero patients were screened using a standardized suicide risk assessment tool. During the study period, the percent of eligible patients who completed a comprehensive suicide risk survey went from 24.6% to 37.4%, with special cause variation detected (Figure 1). Rate of ED crisis evaluation decreased, with detection of special cause variation, from 11.4% baseline to 5.2% during the QI intervention period. Median LOS did not change over time (200.5 minutes (121.5-294.5 IQR) baseline, 213 minutes (135-324 IQR) during the QI intervention). Conclusion(s): Using QI methodology, we improved identification of suicide risk factors among youth in the ED and decreased ED crisis evaluation rates without impacting LOS. We were not able to meet the project aim of 60% survey completion. However, future improvement efforts will include utilization of technology to improve screening practices in our high-acuity and busy ED environment.
Proportion of Patients Screened for Suicide Risk Factors
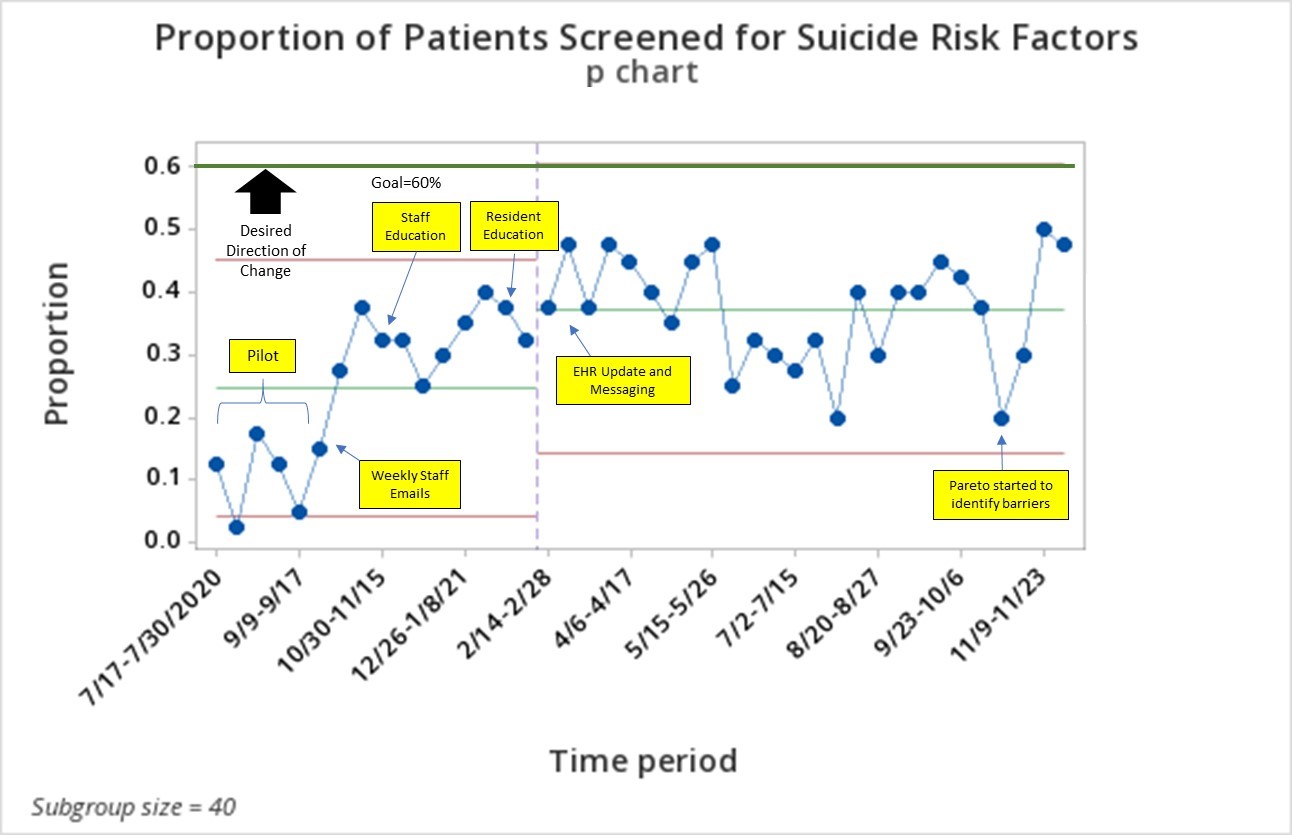 P Chart
P Chart