Mental Health
Category: Abstract Submission
Mental Health I
522 - Increased Rates of Positive Routine Suicide Screens Among Youth in the ED During COVID-19
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 522
Publication Number: 522.422
Publication Number: 522.422
Rachel Cafferty, Children's Hospital Colorado, Denver, CO, United States; Maya Haasz, Children's Hospital Colorado, Aurora, CO, United States; Jan Leonard, University of Colorado Anschutz Medical Campus, Aurora, CO, United States; Lilliam Ambroggio, Children's Hospital Colorado, Aurora, CO, United States
.jpg)
Rachel Cafferty, MD (she/her/hers)
Assistant Professor
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Suicide is the second leading cause of death for adolescents. The pediatric emergency department (PED) is uniquely positioned to provide screening for suicide risk. At the onset of the COVID-19 pandemic, routine screening in the PED identified an increase in suicidal ideation (SI) among patients. SI trends and patient outcomes (i.e. crisis evaluation or psychiatric hospitalization rates) resulting from routine screening with prolonged time in the pandemic are unknown.
Objective: The objectives of this study were to 1) compare rates of positive suicide screens and SI, crisis evaluations, and psychiatric admission among PED or urgent care (UC) patients during the COVID-19 pandemic compared to pre-pandemic, and 2) demonstrate trends over time for positive suicide screens and SI with prolonged time in a pandemic.
Design/Methods: This retrospective cohort study included children aged 10 to 18 years presenting to the PED/UC who completed routine screening for suicide using the validated Ask Suicide Screening Questions (ASQ) between March 1, 2020 and February 28, 2021 of the COVID-19 pandemic and the preceding year. A positive suicide screen was defined as a 'yes' response to any of the ASQ questions. SI was defined by a ‘yes’ response to question(s) one through three on the ASQ. We compared patient demographics and visit characteristics using chi-square, fisher exact, and Wilcoxon Mann Whitney tests. The difference in positive suicide screens and SI was evaluated using interrupted time series with segmented regression analysis.
Results: Of the 28,563 patients who completed routine screening for suicide, 2,231 had a positive screen. During COVID-19 there was an increase in positive suicide screening rates (0.9% (p=0.01)). Among patients with a positive screen, there was an increase in SI rates (4.0% (p=0.05)), ED crisis evaluation rates (1.5% (p=0.03)) and number of patients requiring psychiatric hospitalization (n=4 vs n=7) during COVID-19. During the pandemic, SI and crisis evaluations were more common among younger patients and male patients were more likely to require psychiatric hospitalization. Rates of positive suicide screens and SI were not directly correlated to local or national COVID-19 case rates. Cumulative time in the pandemic resulted in an overall rise in positive suicide screens and SI above predicted rates from pre-pandemic trends.Conclusion(s): This study suggests that youth suicidality may further worsen as the pandemic continues. Younger patients and male patients may represent unique groups requiring targeted resources and intervention for suicide.
Table 1. Characteristics of Patients with a Positive Suicide Screen.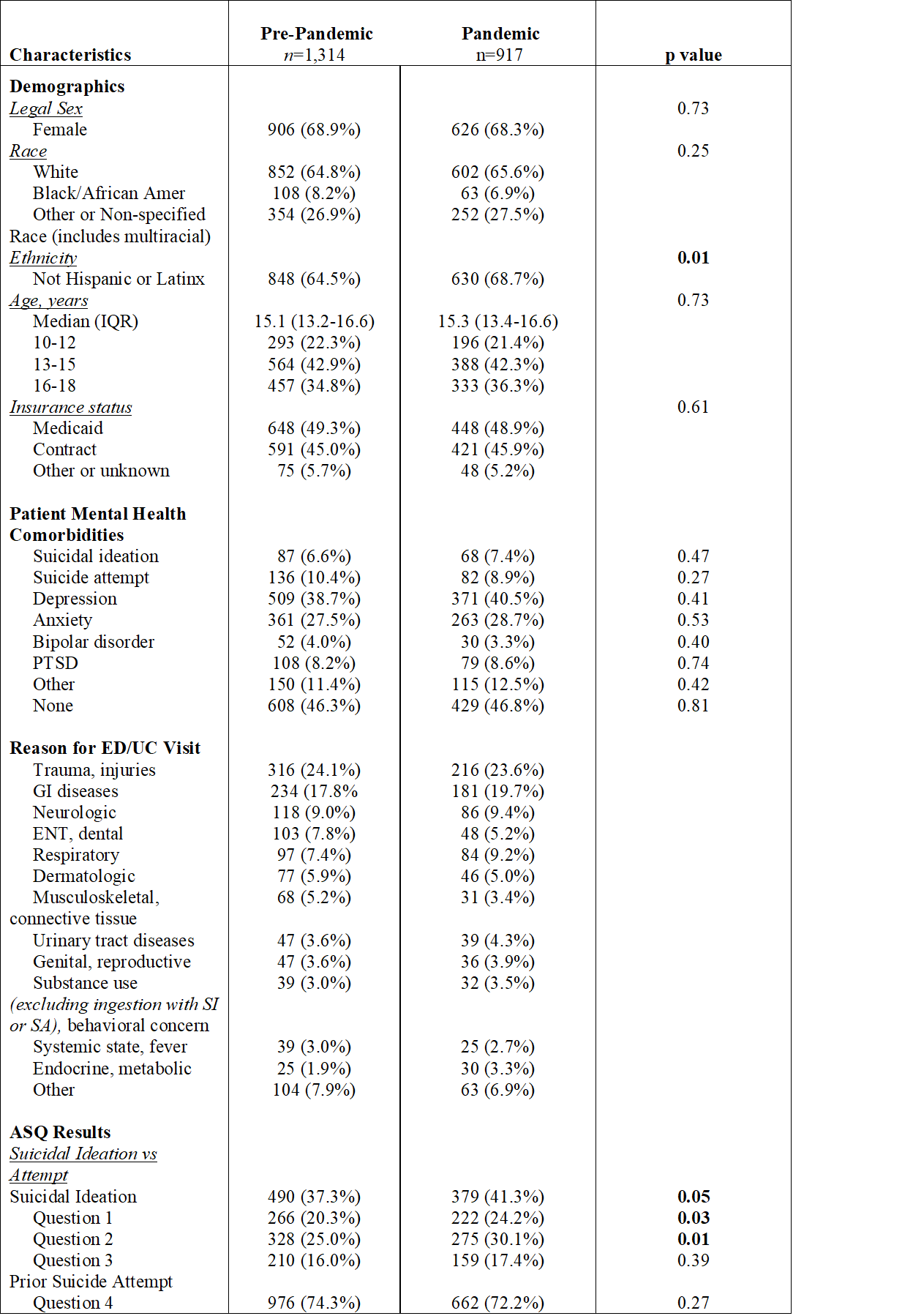
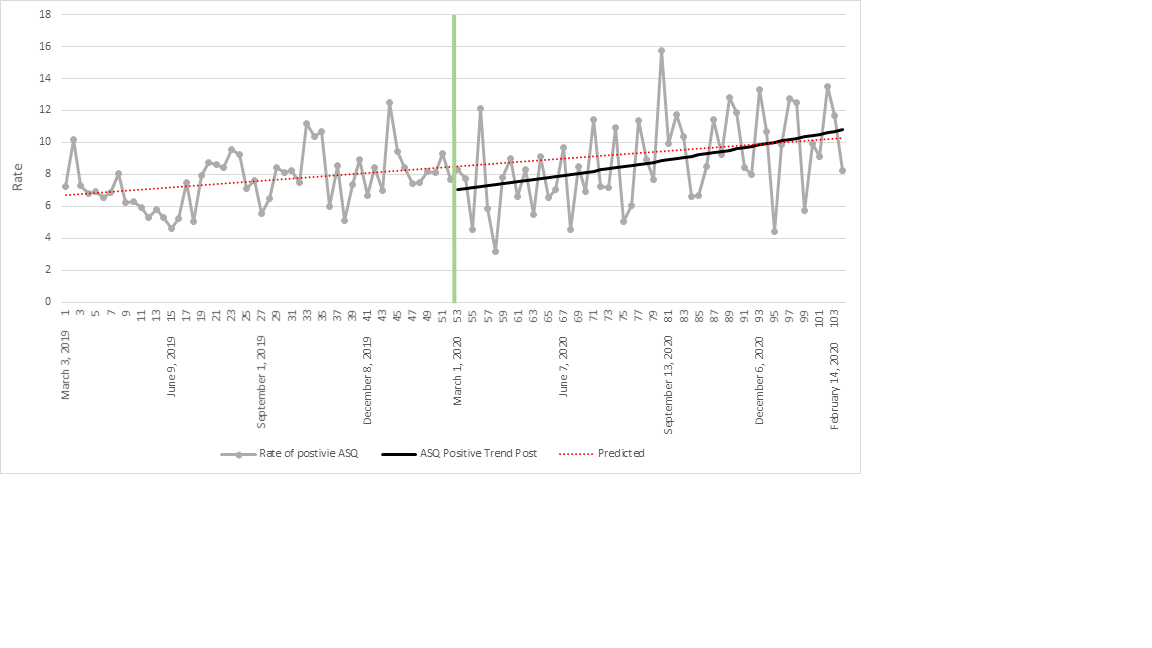
Figure 1. Rate of Positive ASQ Suicide Screens Before and After the Start of the COVID-19 Pandemic, by week.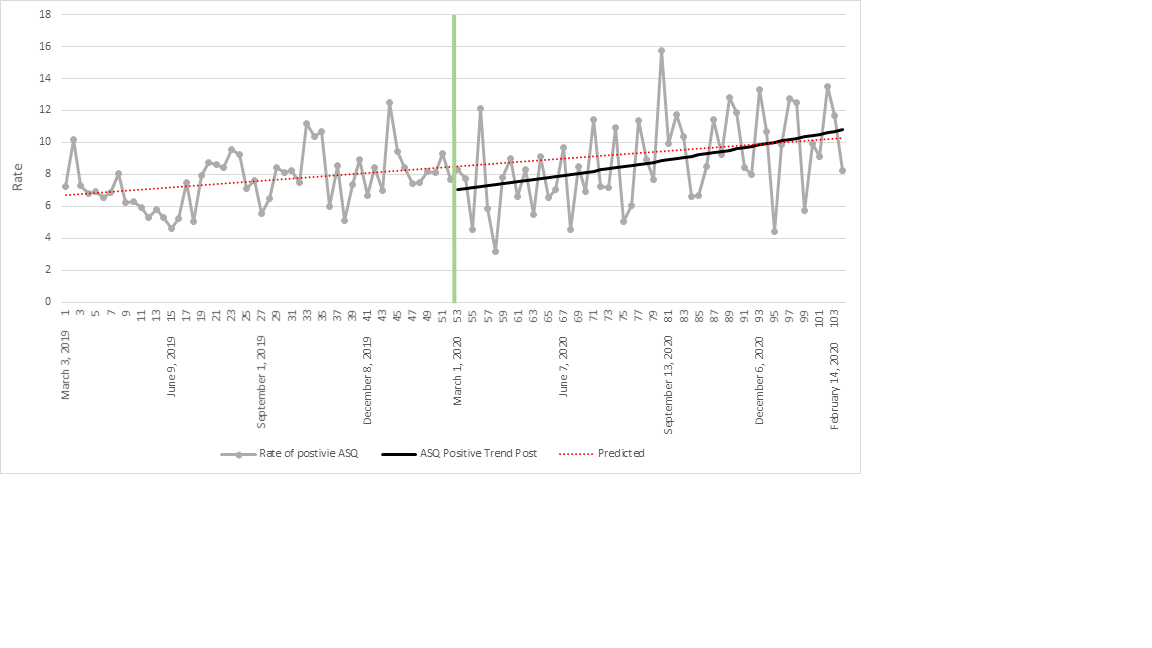
Objective: The objectives of this study were to 1) compare rates of positive suicide screens and SI, crisis evaluations, and psychiatric admission among PED or urgent care (UC) patients during the COVID-19 pandemic compared to pre-pandemic, and 2) demonstrate trends over time for positive suicide screens and SI with prolonged time in a pandemic.
Design/Methods: This retrospective cohort study included children aged 10 to 18 years presenting to the PED/UC who completed routine screening for suicide using the validated Ask Suicide Screening Questions (ASQ) between March 1, 2020 and February 28, 2021 of the COVID-19 pandemic and the preceding year. A positive suicide screen was defined as a 'yes' response to any of the ASQ questions. SI was defined by a ‘yes’ response to question(s) one through three on the ASQ. We compared patient demographics and visit characteristics using chi-square, fisher exact, and Wilcoxon Mann Whitney tests. The difference in positive suicide screens and SI was evaluated using interrupted time series with segmented regression analysis.
Results: Of the 28,563 patients who completed routine screening for suicide, 2,231 had a positive screen. During COVID-19 there was an increase in positive suicide screening rates (0.9% (p=0.01)). Among patients with a positive screen, there was an increase in SI rates (4.0% (p=0.05)), ED crisis evaluation rates (1.5% (p=0.03)) and number of patients requiring psychiatric hospitalization (n=4 vs n=7) during COVID-19. During the pandemic, SI and crisis evaluations were more common among younger patients and male patients were more likely to require psychiatric hospitalization. Rates of positive suicide screens and SI were not directly correlated to local or national COVID-19 case rates. Cumulative time in the pandemic resulted in an overall rise in positive suicide screens and SI above predicted rates from pre-pandemic trends.Conclusion(s): This study suggests that youth suicidality may further worsen as the pandemic continues. Younger patients and male patients may represent unique groups requiring targeted resources and intervention for suicide.
Table 1. Characteristics of Patients with a Positive Suicide Screen.
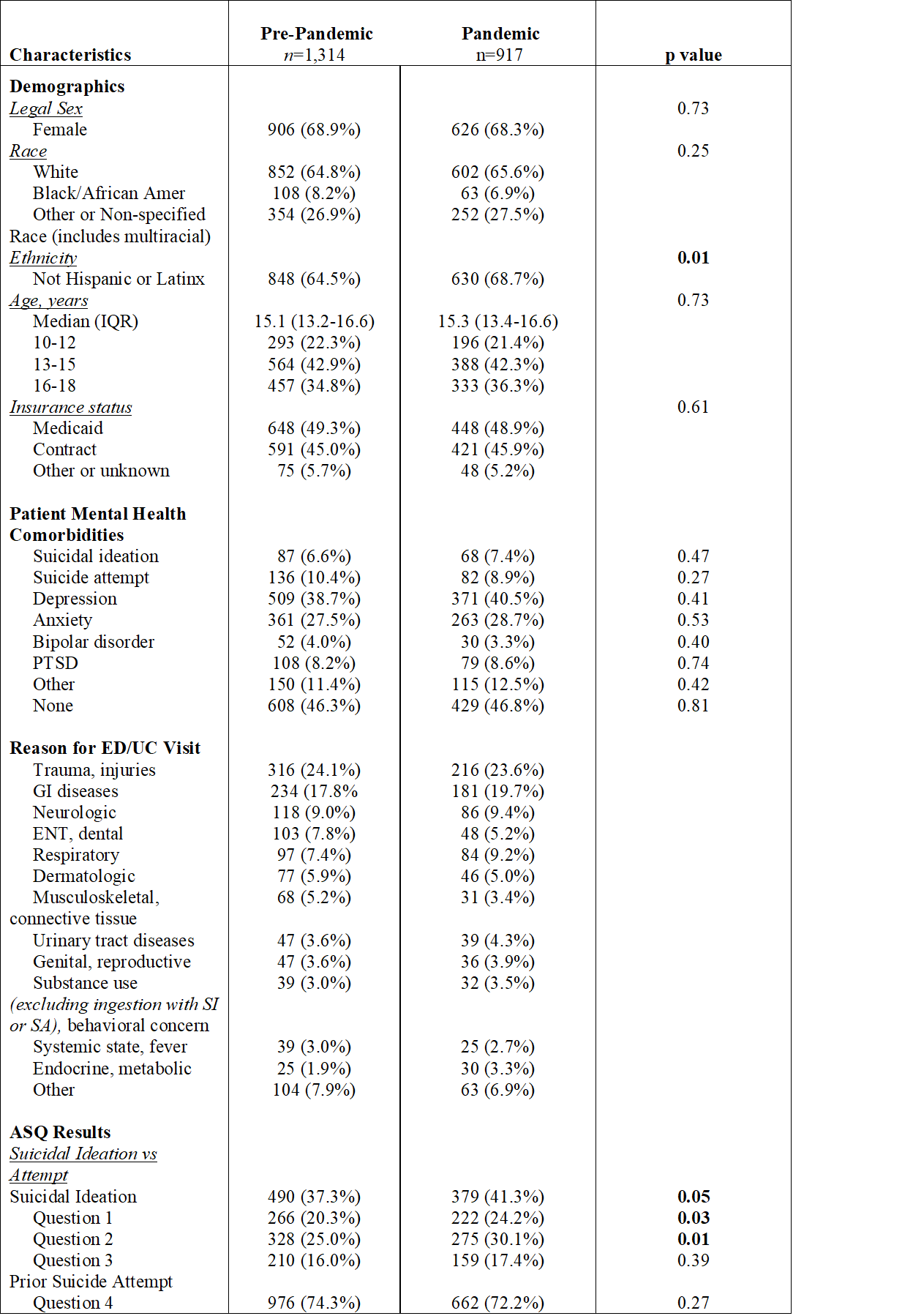
Figure 1. Rate of Positive ASQ Suicide Screens Before and After the Start of the COVID-19 Pandemic, by week.