Emergency Medicine: Quality Improvement
Category: Abstract Submission
Emergency Medicine XIV
53 - Increasing Pediatric Anxiolysis & Analgesia Use in a Community Emergency Department Network: A Quality Improvement Initiative
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 53
Publication Number: 53.407
Publication Number: 53.407
Mariann Kelley, Connecticut Children's Medical Center, Hartford, CT, United States; William Lynders, Middlesex Health, Guilford, CT, United States; Emily Pelletier, Middlesex Health, Old Saybrook, CT, United States; Megan L. Petrucelli, Yale-New Haven Children's Hospital, Cromwell, CT, United States; Beth Emerson, Yale School of Medicine, New Haven, CT, United States; Gunjan Tiyyagura, yale university, New Haven, CT, United States; Michael P. Goldman, Yale School of Medicine, New Haven, CT, United States
- MK
Mariann Kelley, MD (she/her/hers)
Assistant Professor of Pediatrics
Connecticut Children's Medical Center
West Hartford, Connecticut, United States
Presenting Author(s)
Background: Prior reports describe the care children receive in community emergency departments (CEDs) and pediatric emergency departments (PEDs) as uneven. In our state, Emergency Medical Services for Children (EMSC) works to close these gaps using QI methodology. We identified the use of safe and effective pharmacologic and non-pharmacologic anxiolysis and analgesia (A&A) strategies, a routine PED practice, as one such gap.
Objective: This abstract describes initial process analysis to understand pediatric procedural A&A practice in a CED network, increase A&A use and generate a QI toolkit for easy widespread implementation in CEDs.
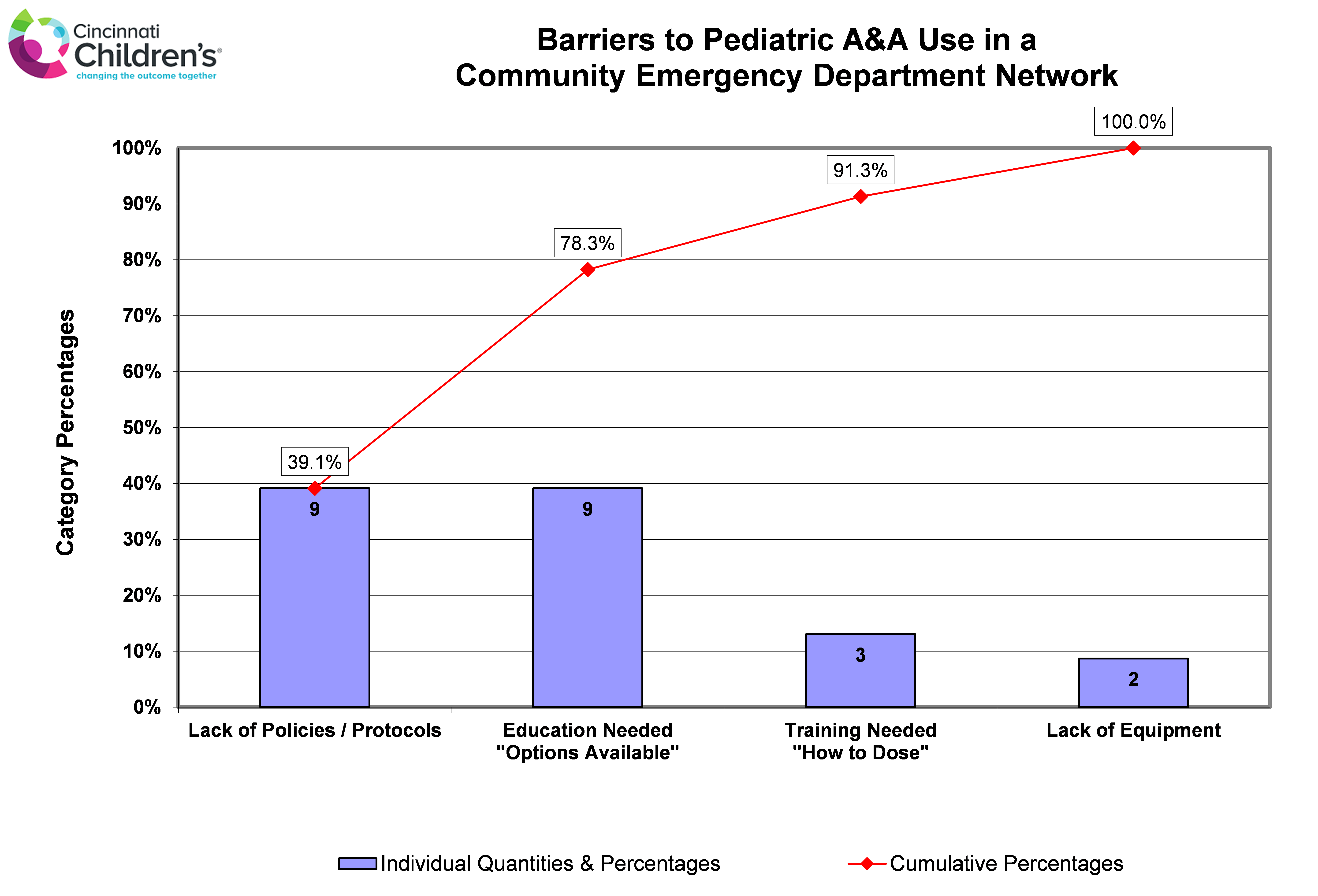
Design/Methods: A team of EMSC stakeholders from 3 hospital networks collaborated. Following the Model for Improvement, we initiated process analysis by reviewing CED A&A practice patterns and compared them to 2 regional PEDs. We also surveyed CED providers about pediatric procedural A&A practice. These data guided our aim statements, identified barriers to A&A use (Pareto chart - fig 1) and informed our key driver diagram (fig 2).
Results: Query of all pediatric procedural data from this CED network identified 2 groups of commonly performed procedures: 1) anxiety-provoking simple procedures such as laceration repairs, abscess drainage and foreign body removal in children less than 8 years old and 2) Intravenous (IV) access in children less than 13 years old. Group one occurred on average 8 times per month and group 2, 16 times per month. Intranasal (IN) versed was used 3% of the time for group 1 and any A&A was documented 11% of the time for group 2. Regional PED practice showed 43% of simple procedures used IN versed and 61% of IVs documented any form of A&A. Twenty-two providers and 20 CED RNs responded to the survey. Fifty-two percent of respondents perceived inconsistent pediatric A&A practice and 69% reported comfort in the rationale for A&A use. From this process analysis, the QI project’s primary aim statements are: In this CED network, in a year’s time, we aim to 1) increase the use of IN versed for anxiety-provoking simple procedures in children less than 8 years old from 3% to 25% and, 2) increase A&A documentation for IV access from 11% to 40%.Conclusion(s): Through process analysis, we characterized a modifiable difference between practice in a PED and a representative CED network. This has informed our measurement strategy, generated the primary aim statements, and guided the prioritization of a series of planned PDSA cycles as noted in the key driver diagram. If successful, we will disseminate a CED A&A QI toolkit throughout our state and beyond through EMSC networks.
Key Driver Diagram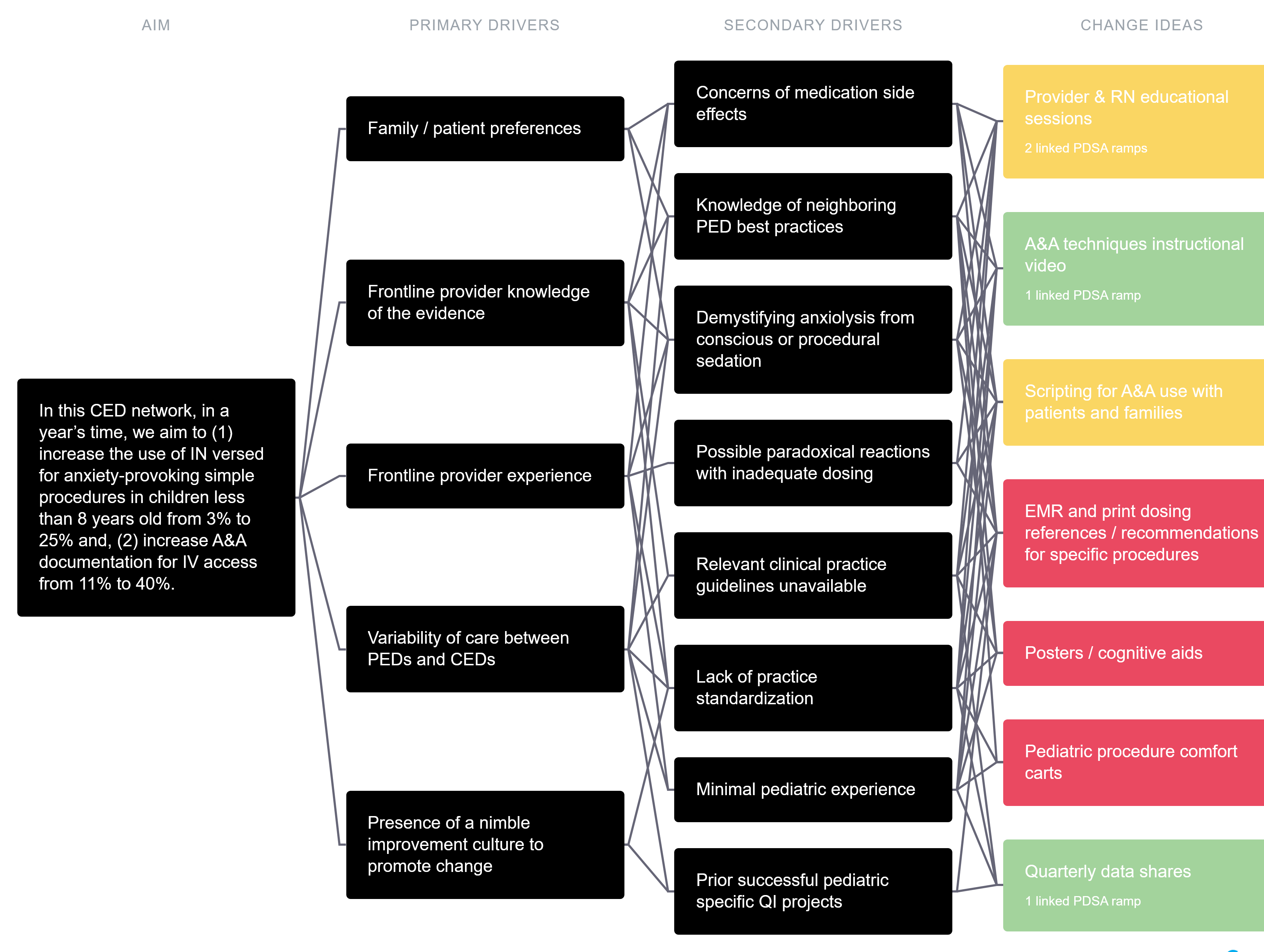 Green = Completed / Ongoing
Green = Completed / Ongoing
Yellow = In process
Red = Planned
Pareto Chart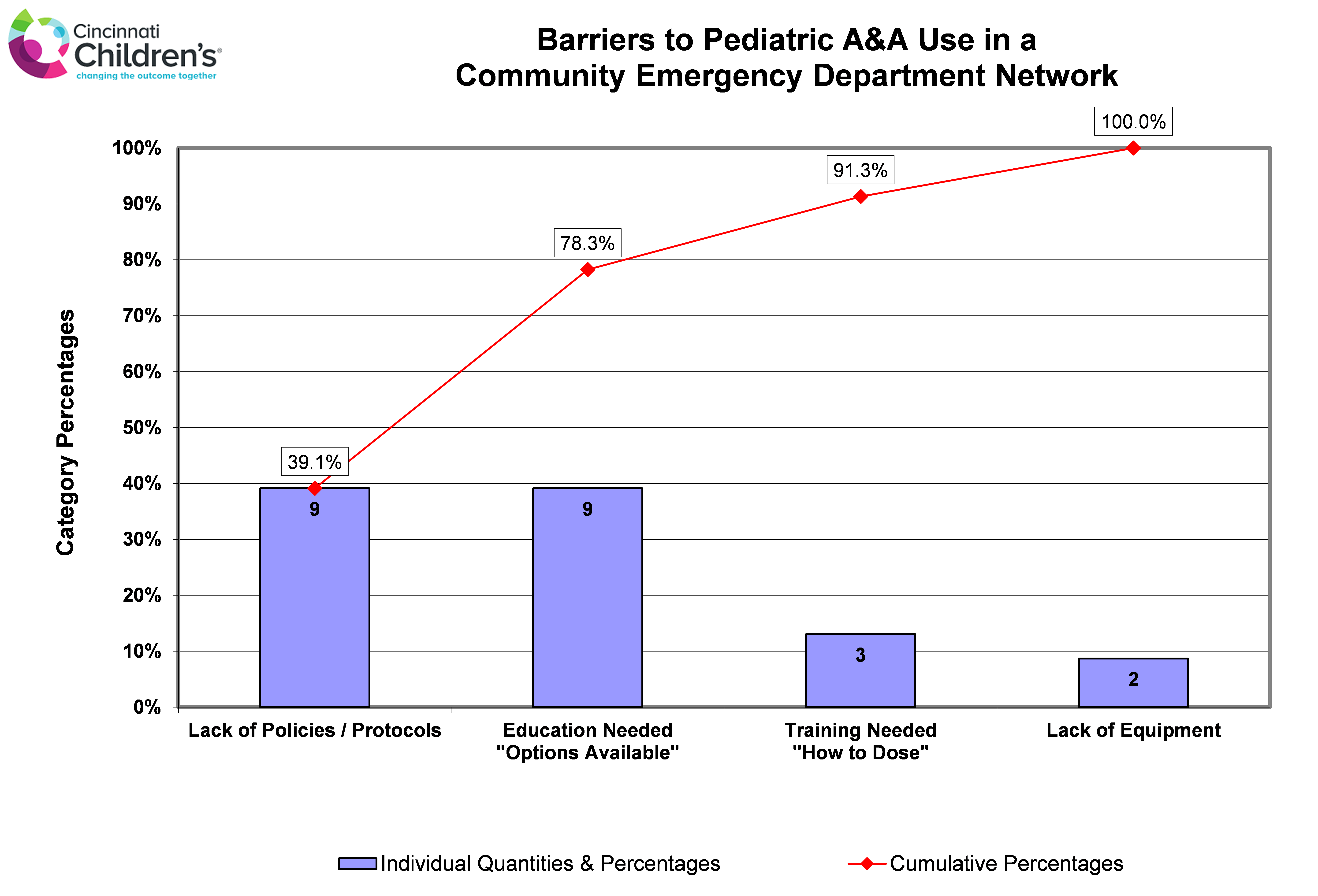
Objective: This abstract describes initial process analysis to understand pediatric procedural A&A practice in a CED network, increase A&A use and generate a QI toolkit for easy widespread implementation in CEDs.
Design/Methods: A team of EMSC stakeholders from 3 hospital networks collaborated. Following the Model for Improvement, we initiated process analysis by reviewing CED A&A practice patterns and compared them to 2 regional PEDs. We also surveyed CED providers about pediatric procedural A&A practice. These data guided our aim statements, identified barriers to A&A use (Pareto chart - fig 1) and informed our key driver diagram (fig 2).
Results: Query of all pediatric procedural data from this CED network identified 2 groups of commonly performed procedures: 1) anxiety-provoking simple procedures such as laceration repairs, abscess drainage and foreign body removal in children less than 8 years old and 2) Intravenous (IV) access in children less than 13 years old. Group one occurred on average 8 times per month and group 2, 16 times per month. Intranasal (IN) versed was used 3% of the time for group 1 and any A&A was documented 11% of the time for group 2. Regional PED practice showed 43% of simple procedures used IN versed and 61% of IVs documented any form of A&A. Twenty-two providers and 20 CED RNs responded to the survey. Fifty-two percent of respondents perceived inconsistent pediatric A&A practice and 69% reported comfort in the rationale for A&A use. From this process analysis, the QI project’s primary aim statements are: In this CED network, in a year’s time, we aim to 1) increase the use of IN versed for anxiety-provoking simple procedures in children less than 8 years old from 3% to 25% and, 2) increase A&A documentation for IV access from 11% to 40%.Conclusion(s): Through process analysis, we characterized a modifiable difference between practice in a PED and a representative CED network. This has informed our measurement strategy, generated the primary aim statements, and guided the prioritization of a series of planned PDSA cycles as noted in the key driver diagram. If successful, we will disseminate a CED A&A QI toolkit throughout our state and beyond through EMSC networks.
Key Driver Diagram
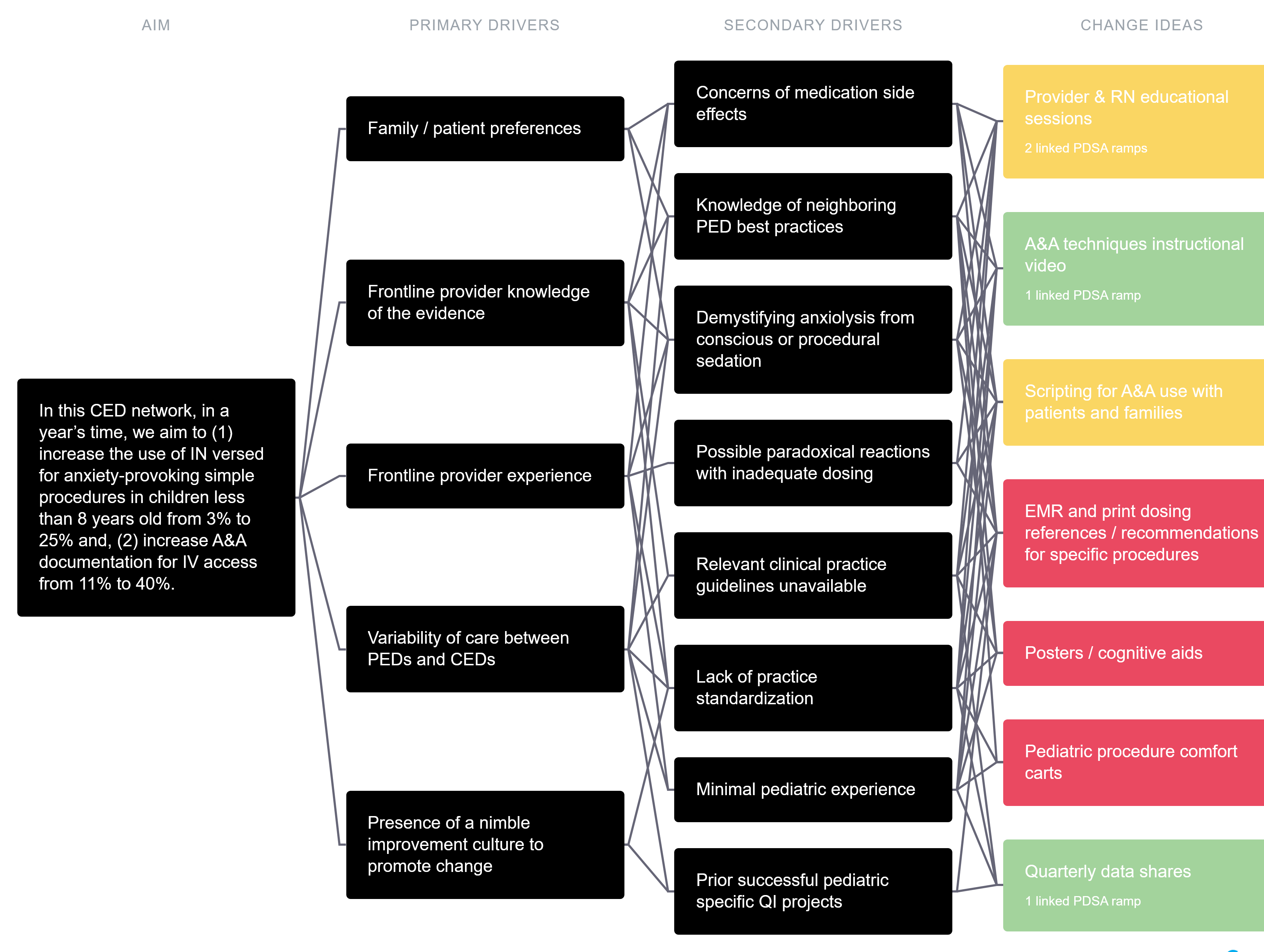 Green = Completed / Ongoing
Green = Completed / OngoingYellow = In process
Red = Planned
Pareto Chart