Emergency Medicine: Quality Improvement
Category: Abstract Submission
Emergency Medicine XIII
39 - Increasing Waveform Capnography Use During Intubations and Cardiac Arrests in a Pediatric Emergency Department
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 39
Publication Number: 39.406
Publication Number: 39.406
Chisom Agbim, Children's Hospital Colorado, Aurora, CO, United States; Kristina Brumme, University of Colorado School of Medicine, Lincoln, MA, United States; Stacey Coss, Childrens Hospital Colorado, Denver, CO, United States; Korey L. Preston, Childrens Hospital of Colorado, Thornton, CO, United States; Tara Neubrand, Children's Hospital Colorado/University of Colorado, Denver, CO, United States

Chisom Agbim, MD, MSHS
Attending Physician, Pediatric Emergency Medicine
Children's Hospital Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background: Waveform capnography is the continuous, noninvasive measurement and graphical display of exhaled end-tidal carbon dioxide (ETCO2). National guidelines recommend the use of ETCO2 detection via capnography to confirm endotracheal tube placement, monitor cardiopulmonary resuscitation (CPR) quality, and detect the return of spontaneous circulation in intubated patients.
Our hospital is a freestanding tertiary care children’s hospital and level one trauma center with a dedicated pediatric emergency department (PED) that has 90,000 patient visits per year. Between 2018 and 2020, there was an annual average of 32 cardiac arrests and 105 intubations in the PED. Prior to this study, there was inconsistent use of waveform capnography in the PED.
Objective: Our goal was to improve outcomes for patients during PED intubations and CPR events. Our SMART aim was to increase waveform capnography use from 20% to 85% in PED intubations and increase from 33% to 70% in PED cardiac arrests within 6 months beginning in January 2021 and to maintain these targets for at least 3 months.
Design/Methods: This quality improvement (QI) study was led by two PED physicians (MDs), an ED nurse (RN) and a respiratory therapist (RT). The primary and outcome measures were the proportion of resuscitations with documented waveform capnography use. The balancing measure was the percentage of patients requiring >1 reintubation attempt. Interventions included educational initiatives for all ED provider groups regarding the importance and benefits of waveform capnography, replacing colorimetry with waveform capnography as the standard of care for all intubations in the PED, integrating waveform capnography training into the RT orientation and competencies, and working with the RTs and RNs to improve documentation of waveform capnography use in resuscitations.
Results: We collected data from January 2020 to November 2021. Our data for waveform capnography use in PED intubations showed special cause variation with a center line shift from 29% to 81% and sustained change for 10 months. Waveform capnography use in PED cardiac arrests also increased, trending toward special cause variation. Our balancing measures remained unchanged.Conclusion(s): Using QI methodology, we increased the use of waveform capnography during intubations and cardiac arrest in a freestanding PED. Future work will focus on achieving 100% compliance with PED waveform capnography use, expanding our efforts to additional PED sites within our hospital network, using waveform capnography to assess CPR quality, and targeting specific ETCO2 goals to improve post-resuscitation care.
Figure 1. Proportion of PED Intubations with Waveform Capnography Use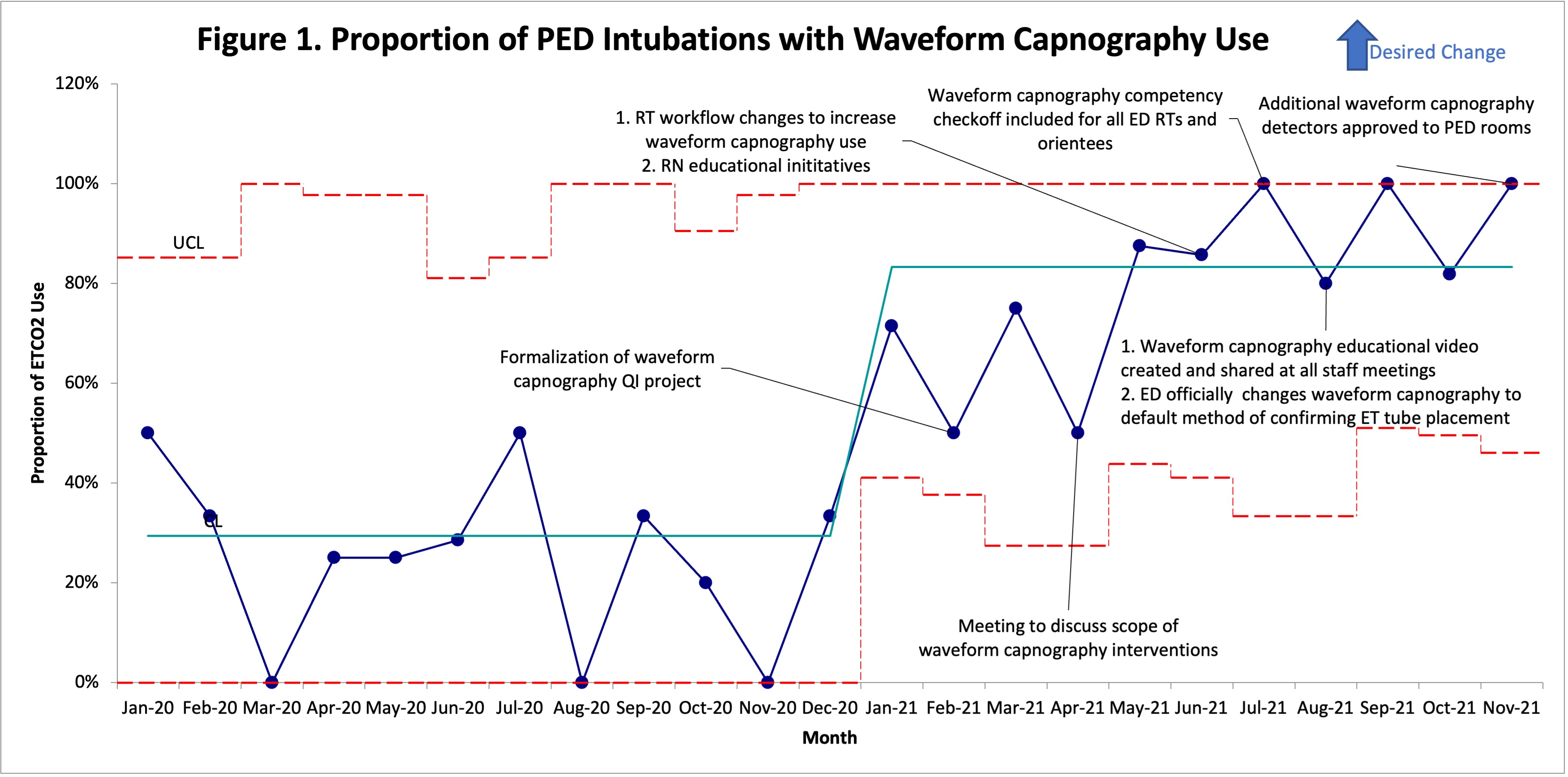 The proportion of waveform capnography use in PED intubations per month from January 2020 to November 2021
The proportion of waveform capnography use in PED intubations per month from January 2020 to November 2021
Figure 2. Proportion of PED Cardiac Arrests with Waveform Capnography Use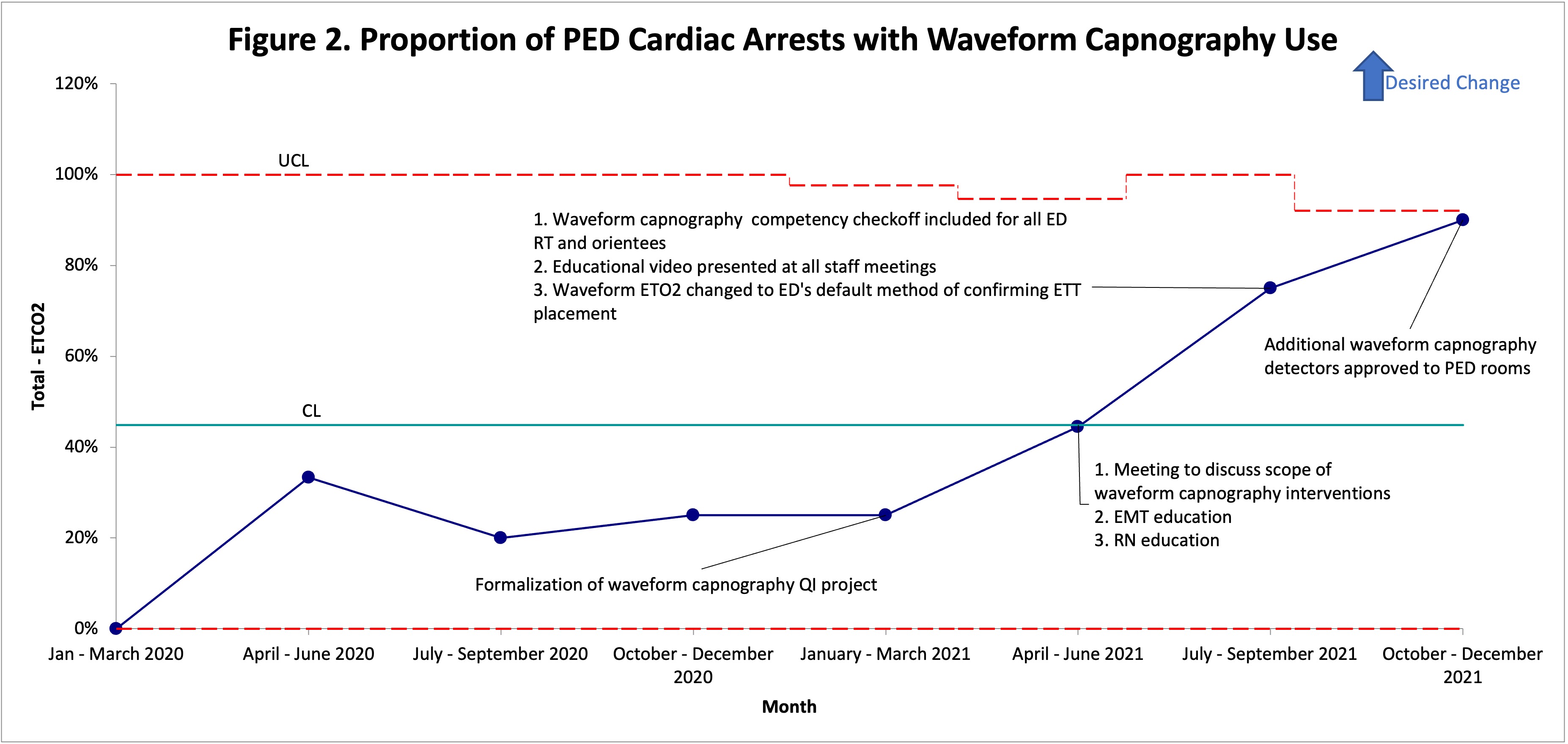 The proportion of waveform capnography use in PED cardiac arrests per quarter from January 2020 to November 2021
The proportion of waveform capnography use in PED cardiac arrests per quarter from January 2020 to November 2021
Our hospital is a freestanding tertiary care children’s hospital and level one trauma center with a dedicated pediatric emergency department (PED) that has 90,000 patient visits per year. Between 2018 and 2020, there was an annual average of 32 cardiac arrests and 105 intubations in the PED. Prior to this study, there was inconsistent use of waveform capnography in the PED.
Objective: Our goal was to improve outcomes for patients during PED intubations and CPR events. Our SMART aim was to increase waveform capnography use from 20% to 85% in PED intubations and increase from 33% to 70% in PED cardiac arrests within 6 months beginning in January 2021 and to maintain these targets for at least 3 months.
Design/Methods: This quality improvement (QI) study was led by two PED physicians (MDs), an ED nurse (RN) and a respiratory therapist (RT). The primary and outcome measures were the proportion of resuscitations with documented waveform capnography use. The balancing measure was the percentage of patients requiring >1 reintubation attempt. Interventions included educational initiatives for all ED provider groups regarding the importance and benefits of waveform capnography, replacing colorimetry with waveform capnography as the standard of care for all intubations in the PED, integrating waveform capnography training into the RT orientation and competencies, and working with the RTs and RNs to improve documentation of waveform capnography use in resuscitations.
Results: We collected data from January 2020 to November 2021. Our data for waveform capnography use in PED intubations showed special cause variation with a center line shift from 29% to 81% and sustained change for 10 months. Waveform capnography use in PED cardiac arrests also increased, trending toward special cause variation. Our balancing measures remained unchanged.Conclusion(s): Using QI methodology, we increased the use of waveform capnography during intubations and cardiac arrest in a freestanding PED. Future work will focus on achieving 100% compliance with PED waveform capnography use, expanding our efforts to additional PED sites within our hospital network, using waveform capnography to assess CPR quality, and targeting specific ETCO2 goals to improve post-resuscitation care.
Figure 1. Proportion of PED Intubations with Waveform Capnography Use
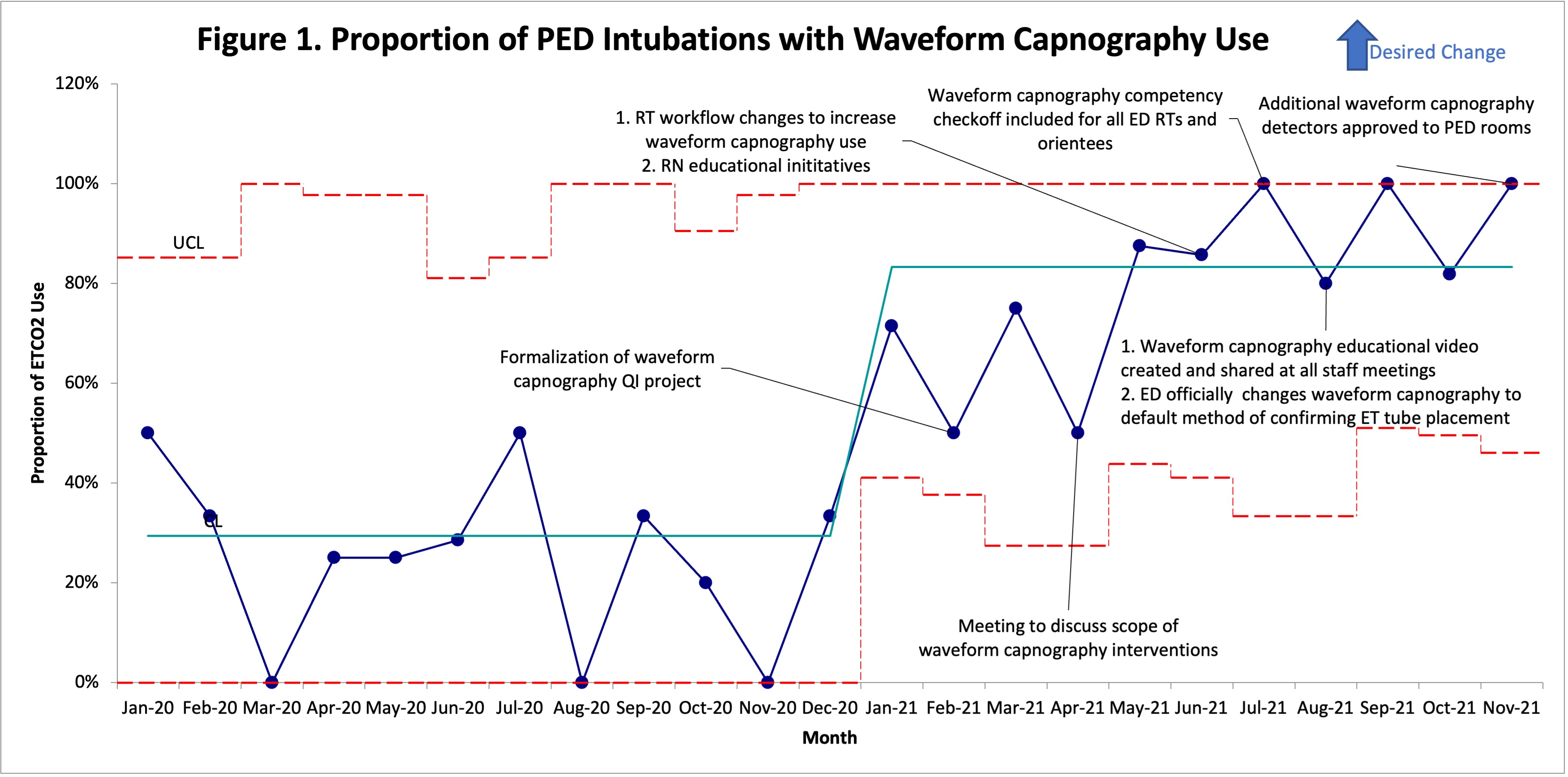 The proportion of waveform capnography use in PED intubations per month from January 2020 to November 2021
The proportion of waveform capnography use in PED intubations per month from January 2020 to November 2021Figure 2. Proportion of PED Cardiac Arrests with Waveform Capnography Use
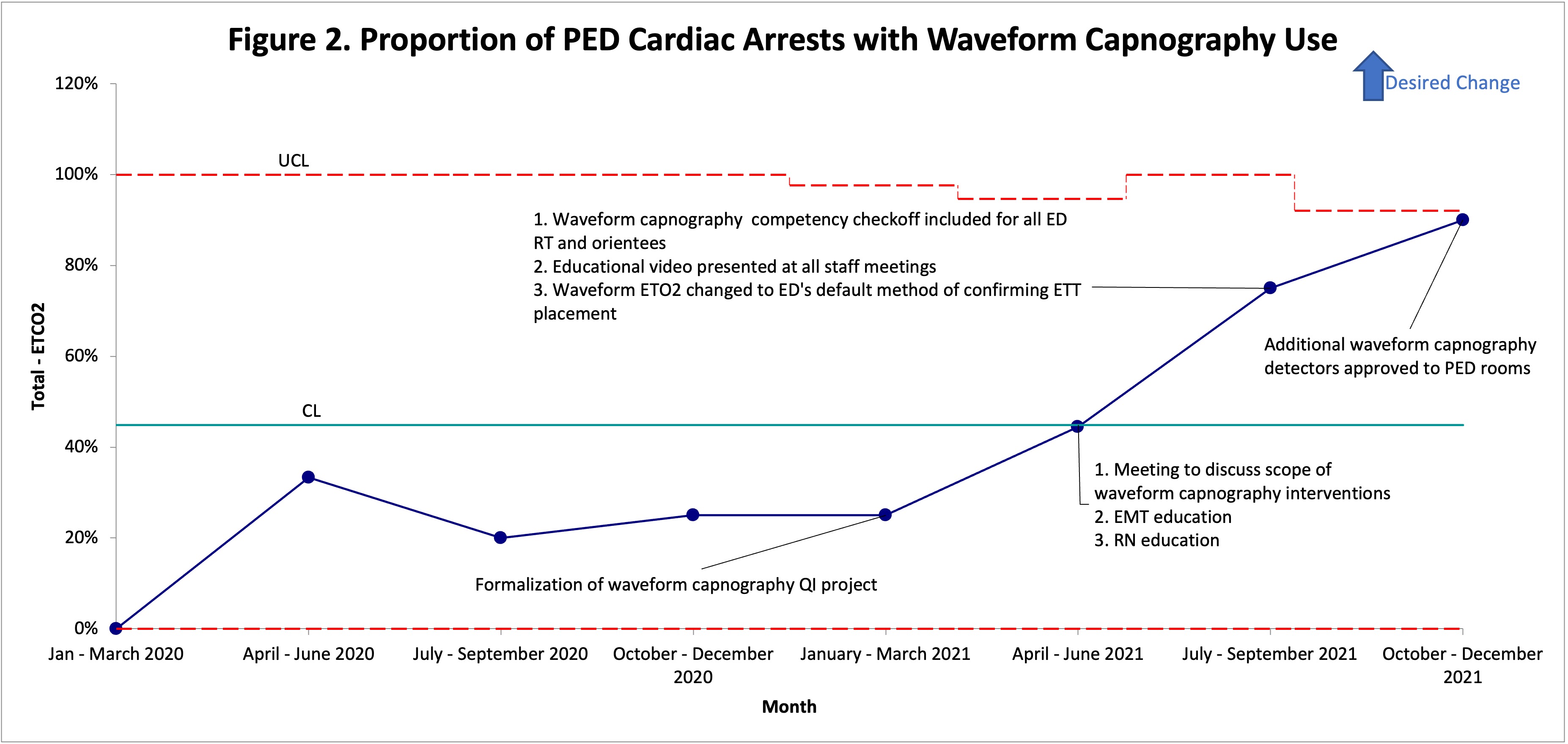 The proportion of waveform capnography use in PED cardiac arrests per quarter from January 2020 to November 2021
The proportion of waveform capnography use in PED cardiac arrests per quarter from January 2020 to November 2021