Medical Education: Resident
Category: Abstract Submission
Medical Education 14 - Medical Education: Resident V
273 - Drivers and Barriers to resident participation in relationships with caregivers of children with medical complexity: a qualitative assessment of reflective writing
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 273
Publication Number: 273.420
Publication Number: 273.420
Kira R. Sieplinga, Pediatric Residency - Helen DeVos Children's Hospital/Spectrum Health, Grand Rapids, MI, United States; Christopher J. Kruger, Michigan State University College of Human Medicine, Grand Rapids, MI, United States; Denise M. Acevedo, Michigan State University, East Lansing, MI, United States; J.M.Monica van de Ridder, Michigan State University College of Human Medicine/ Spectrum Health, Grand Rapids, MI, United States

Christopher J. Kruger, MS4
Medical Student
Michigan State University College of Human Medicine
Grand Rapids, Michigan, United States
Presenting Author(s)
Background: Children with Medical Complexity (CMC) comprise a small portion of the pediatric population yet a large share of healthcare effort. Pediatric residents do not feel comfortable with care for CMC upon graduation and list lack of connection with CMC caregivers as a barrier. Pre-training drivers and barriers for CMC care are not known.
Objective: To explore drivers and barriers for CMC care present at the beginning of pediatric residency prior to implementation of a longitudinal relationship-based curriculum.
Design/Methods: In July 2021, the authors utilized a social capital framework to create a longitudinal curriculum entitled: “Building Connections: A year-long journey with a CMC.” The curriculum pairs pediatric interns with a caregiver of a CMC and seeks to increase empathy through guided conversations and reflective writing. During a single in-person session, 22 pediatric interns were taught about CMC, social capital, and reflective writing. Participants were then enrolled in the curriculum and asked to submit reflective writing pieces with a prompt created by local experts informed by the reflective learning framework. 22 pieces were received and analyzed utilizing grounded theory through several rounds of induction and comparison. Inferential statistics were applied to code frequencies (table 1) using a two-sample T-test.
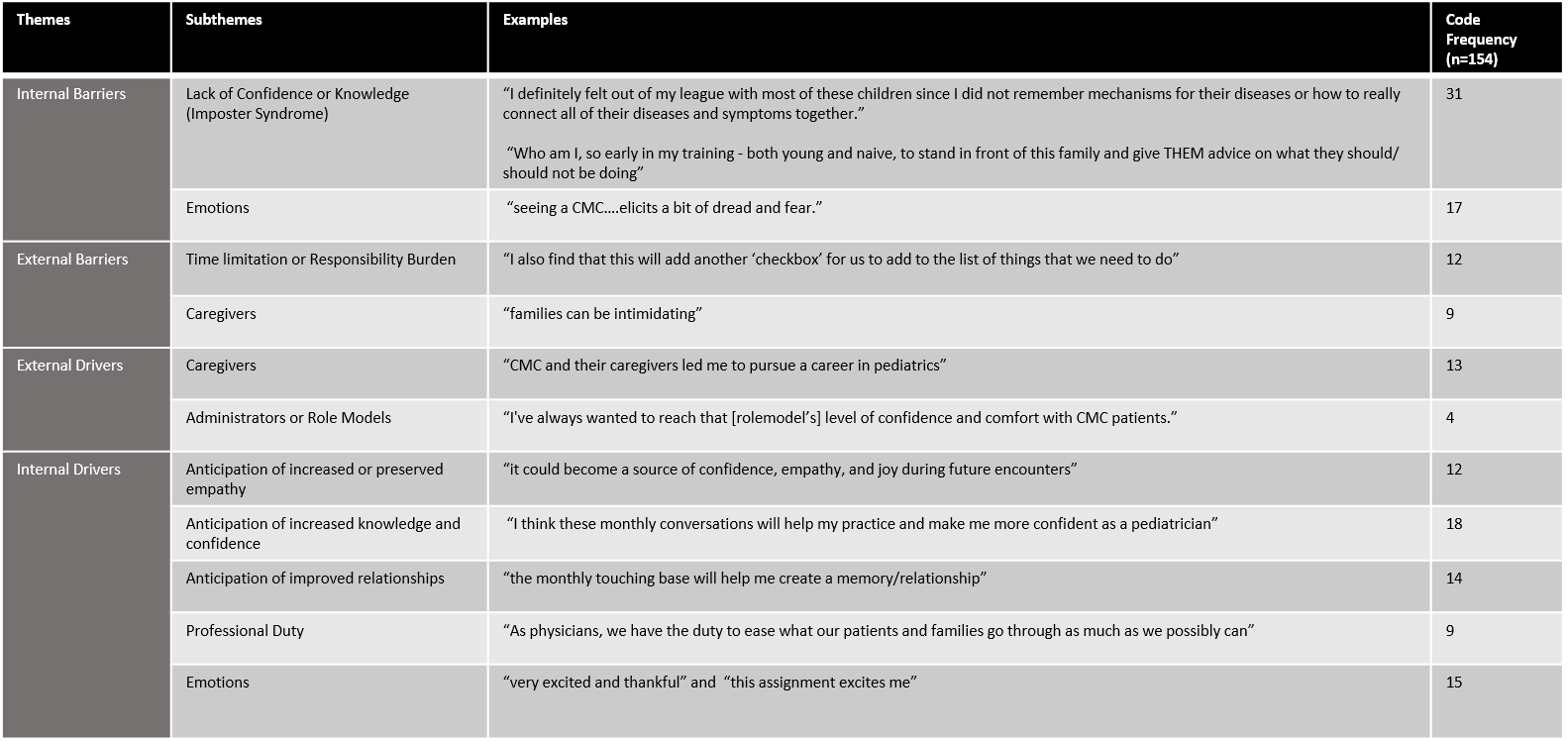
Results: Analysis of responses to the prompt question stem that explored past experiences and current feelings toward a longitudinal relationship with a caregiver of CMC revealed 4 themes and 11 sub-themes with respect to anticipated participation in the curriculum. These were organized into internal and external drivers and barriers, and code frequencies were determined. A total of 154 codes were categorized. Internal factors (116/154) were mentioned more frequently than external factors (38/154, p < 0.001) and of the internal factors, drivers (68/116) were noted more frequently then barriers (48/116, p < 0.003). Caregivers of CMC were categorized as both drivers and barriers. Individual reflective writing pieces tended to lack balance and were frequently weighted either toward drivers or barriers. Conclusion(s): Pediatric residents at the beginning of their training approach relationships with caregivers of CMC with pre-established drivers and barriers to participation. Pediatric educators should recognize residents’ mindset upon arrival to residency and design curriculum with a goal of maximizing drivers and minimizing barriers. Caregivers serve as both drivers and barriers and may play a valuable role in further curricular development.
Figure 1: Introduction module writing prompt presented to participants utilizing an anonymous online portal.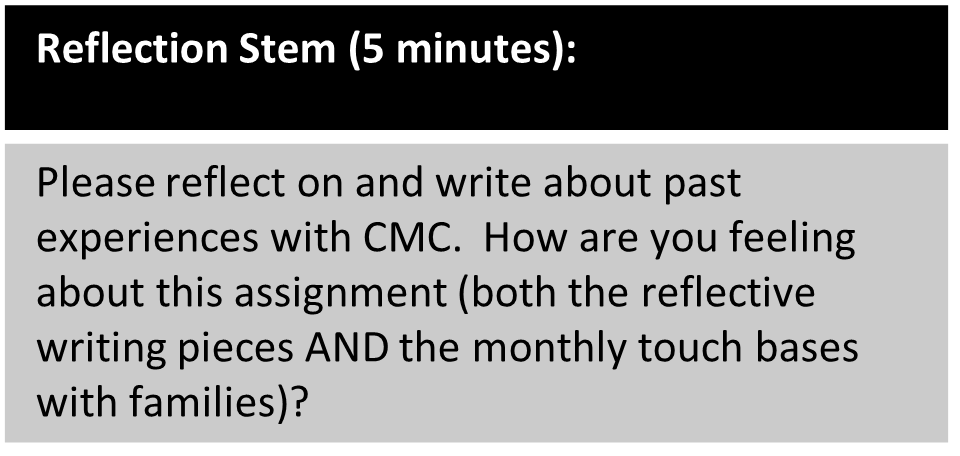
Table 1: Barriers and Drivers identified through analysis of reflective writing pieces submitted prior to initiation of a longitudinal relationship pairing pediatric interns with caregivers of Children with Medical Complexity (n=22)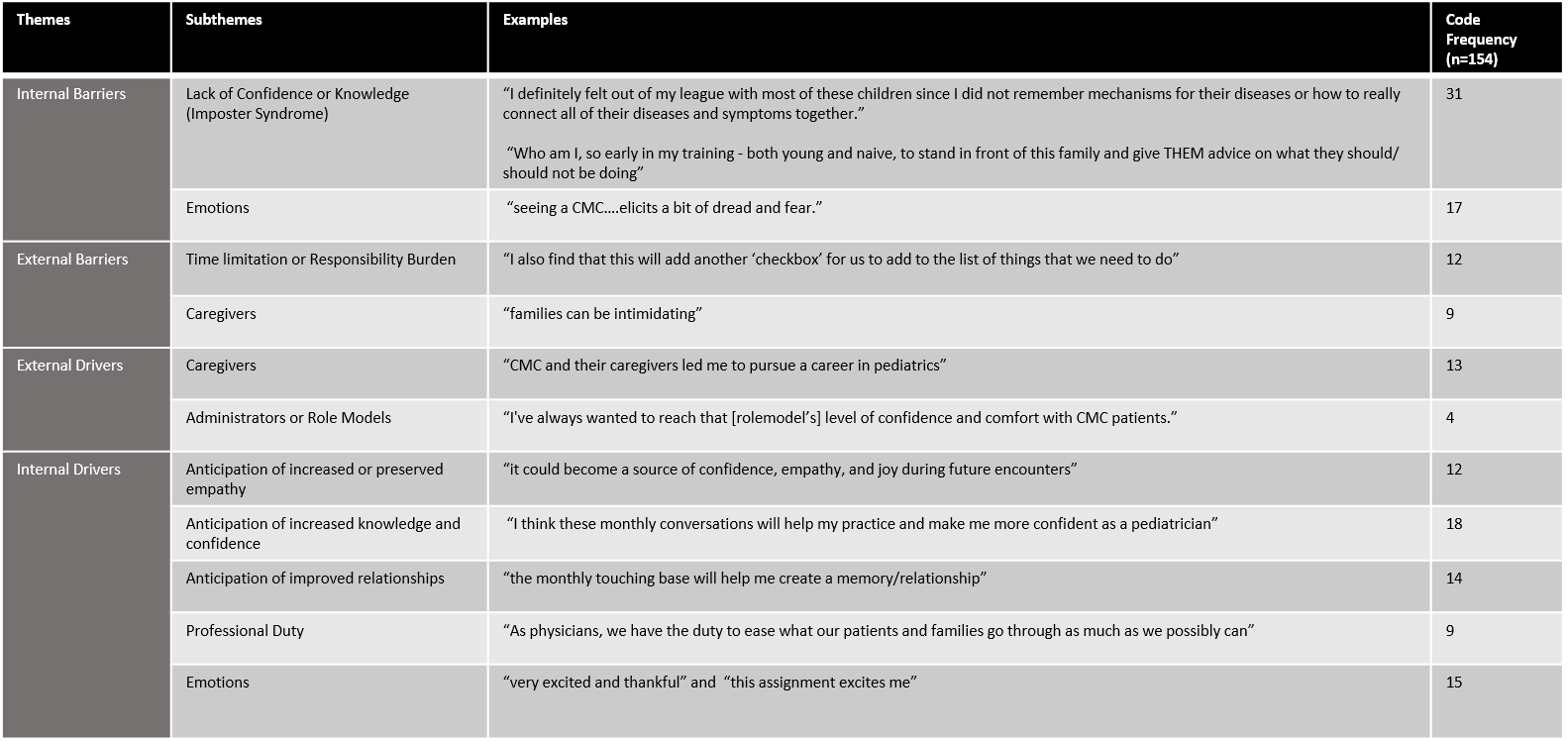
Objective: To explore drivers and barriers for CMC care present at the beginning of pediatric residency prior to implementation of a longitudinal relationship-based curriculum.
Design/Methods: In July 2021, the authors utilized a social capital framework to create a longitudinal curriculum entitled: “Building Connections: A year-long journey with a CMC.” The curriculum pairs pediatric interns with a caregiver of a CMC and seeks to increase empathy through guided conversations and reflective writing. During a single in-person session, 22 pediatric interns were taught about CMC, social capital, and reflective writing. Participants were then enrolled in the curriculum and asked to submit reflective writing pieces with a prompt created by local experts informed by the reflective learning framework. 22 pieces were received and analyzed utilizing grounded theory through several rounds of induction and comparison. Inferential statistics were applied to code frequencies (table 1) using a two-sample T-test.
Results: Analysis of responses to the prompt question stem that explored past experiences and current feelings toward a longitudinal relationship with a caregiver of CMC revealed 4 themes and 11 sub-themes with respect to anticipated participation in the curriculum. These were organized into internal and external drivers and barriers, and code frequencies were determined. A total of 154 codes were categorized. Internal factors (116/154) were mentioned more frequently than external factors (38/154, p < 0.001) and of the internal factors, drivers (68/116) were noted more frequently then barriers (48/116, p < 0.003). Caregivers of CMC were categorized as both drivers and barriers. Individual reflective writing pieces tended to lack balance and were frequently weighted either toward drivers or barriers. Conclusion(s): Pediatric residents at the beginning of their training approach relationships with caregivers of CMC with pre-established drivers and barriers to participation. Pediatric educators should recognize residents’ mindset upon arrival to residency and design curriculum with a goal of maximizing drivers and minimizing barriers. Caregivers serve as both drivers and barriers and may play a valuable role in further curricular development.
Figure 1: Introduction module writing prompt presented to participants utilizing an anonymous online portal.
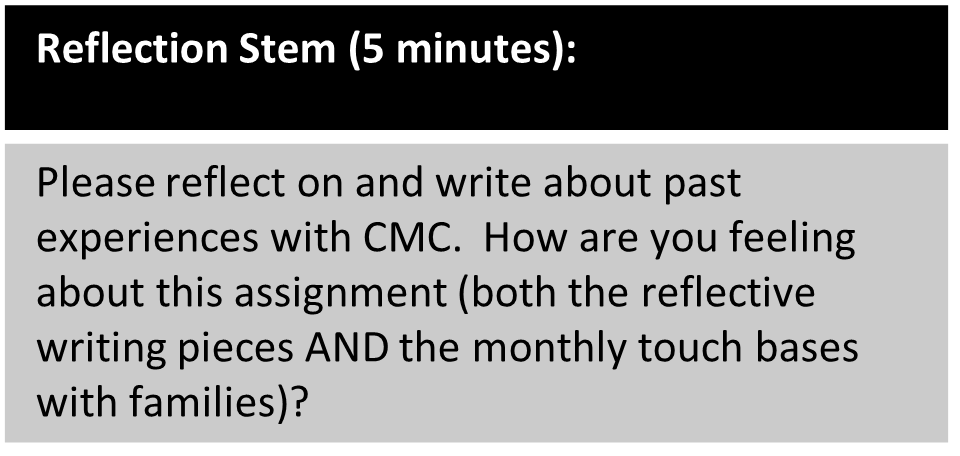
Table 1: Barriers and Drivers identified through analysis of reflective writing pieces submitted prior to initiation of a longitudinal relationship pairing pediatric interns with caregivers of Children with Medical Complexity (n=22)