Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: Sepsis & Antimicrobials
549 - Early antimicrobial exposure and weight gain in extremely low gestation age infants without culture-proven sepsis or intestinal pathologies.
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 549
Publication Number: 549.428
Publication Number: 549.428
Prakesh Shah, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Marc Beltempo, McGill University, Montreal, PQ, Canada; Jennifer Toye, University of Alberta Faculty of Medicine and Dentistry, Edmonton, AB, Canada; Faiza Khurshid, Queen's University Faculty of Health Sciences, Kingston, ON, Canada; Xiang Y. Ye, MiCare research Center, Mount Sinai Hospital, Toronto, ON, Canada, Toronto, ON, Canada; Joseph Ting, University of Alberta, Edmonton, AB, Canada
Joseph Ting, MD, MPH
Associate Professor
University of Alberta
Edmonton, Alberta, Canada
Presenting Author(s)
Background: Early antimicrobial exposure may result in alternation of microbiome, leading to long-lasting perturbations of metabolic pathways and other health consequences. There is a paucity of data on the impact of antimicrobial exposure in the neonatal intensive care unit (NICU) on growth among preterm infants in their early childhood.
Objective: To determine the association between antimicrobial use and change in weight z score from birth to early childhood among extremely low gestational age neonates (ELGAN) without culture-proven sepsis, spontaneous intestinal perforation (SIP) or necrotizing enterocolitis (NEC) in the NICU.
Design/Methods: We conducted a retrospective cohort study of preterm neonates born at < 29 weeks’ gestation age [GA] who were admitted between Apr 2010 and Dec 2017 to NICUs participating in the Canadian Neonatal Network and Canadian Neonatal Follow-up Network. Only infants without culture-proven sepsis, SIP or ≥Stage II NEC were included in this study. Antimicrobial utilization rate (AUR), defined as the number of days an infant is exposed to at least one antimicrobial agent divided by the total length of NICU stay, was compared with the change in weight z-score from birth to 18-24months’ corrected age (CA) using univariate and multivariable general linear models adjusted for potential confounders.
Results: There were 2377 eligible infants in our study (Figure 1), with a median AUR of 12 days (IQR, 6-20) and a median GA of 27 weeks (IQR, 26-28). The mean weight z-score (WT z-score) decreased from 0.04±0.82 at birth to -0.59±1.10 at 18-24 months’ CA, with a mean difference in weight z-score (ΔWT z-score) of -0.62±1.10. There was a negative correlation between ΔWT z-score and AUR (Figure 2). After adjusting for potential confounders identified in the univariate analysis, the AUR was still negatively associated with ΔWT z-score at 18-24 month’s CA from birth (p=0.035, Table 1). Subgroup analyses were also conducted among those who received probiotics (23.8% or 566/2377) and those born small-for-gestational age (SGA) (6.6% or 156/2377). We revealed a negative association between AUR and ΔWT z-score (p=0.037) in those who received probiotics, but no such correlation was found among infants born SGA (p=0.819). Conclusion(s): Higher AUR during NICU stay among preterm infants of < 29 weeks’ gestation without sepsis or intestinal pathologies was negatively correlated with change in weight z-score reflecting reduced interval weight gain from birth to early childhood. This association highlights the need to better understand the effects of early antimicrobial exposure on early childhood health.
Figure 1: Study population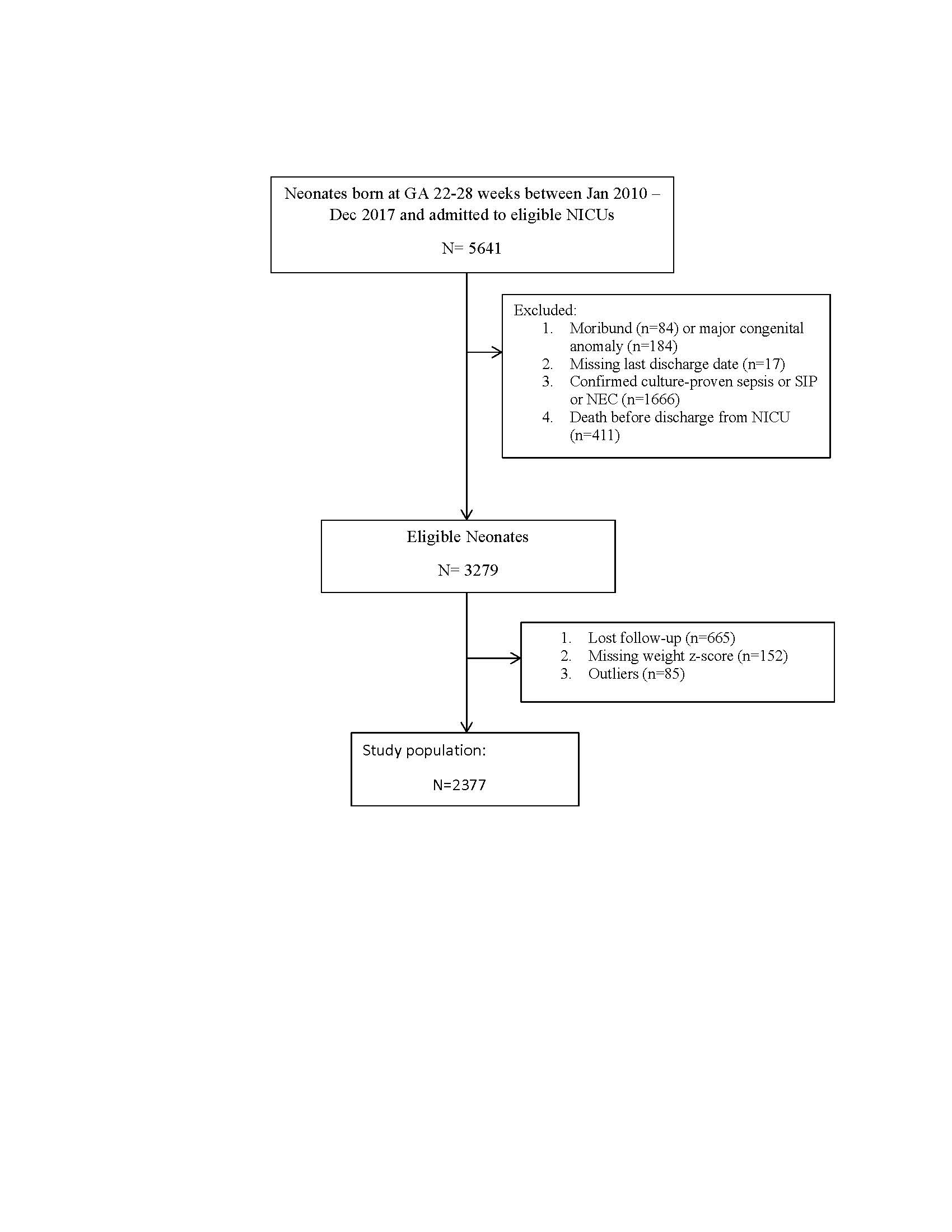
Figure 2: Linear relationship between ΔWT z-score and AUR for all infants.jpg)
Objective: To determine the association between antimicrobial use and change in weight z score from birth to early childhood among extremely low gestational age neonates (ELGAN) without culture-proven sepsis, spontaneous intestinal perforation (SIP) or necrotizing enterocolitis (NEC) in the NICU.
Design/Methods: We conducted a retrospective cohort study of preterm neonates born at < 29 weeks’ gestation age [GA] who were admitted between Apr 2010 and Dec 2017 to NICUs participating in the Canadian Neonatal Network and Canadian Neonatal Follow-up Network. Only infants without culture-proven sepsis, SIP or ≥Stage II NEC were included in this study. Antimicrobial utilization rate (AUR), defined as the number of days an infant is exposed to at least one antimicrobial agent divided by the total length of NICU stay, was compared with the change in weight z-score from birth to 18-24months’ corrected age (CA) using univariate and multivariable general linear models adjusted for potential confounders.
Results: There were 2377 eligible infants in our study (Figure 1), with a median AUR of 12 days (IQR, 6-20) and a median GA of 27 weeks (IQR, 26-28). The mean weight z-score (WT z-score) decreased from 0.04±0.82 at birth to -0.59±1.10 at 18-24 months’ CA, with a mean difference in weight z-score (ΔWT z-score) of -0.62±1.10. There was a negative correlation between ΔWT z-score and AUR (Figure 2). After adjusting for potential confounders identified in the univariate analysis, the AUR was still negatively associated with ΔWT z-score at 18-24 month’s CA from birth (p=0.035, Table 1). Subgroup analyses were also conducted among those who received probiotics (23.8% or 566/2377) and those born small-for-gestational age (SGA) (6.6% or 156/2377). We revealed a negative association between AUR and ΔWT z-score (p=0.037) in those who received probiotics, but no such correlation was found among infants born SGA (p=0.819). Conclusion(s): Higher AUR during NICU stay among preterm infants of < 29 weeks’ gestation without sepsis or intestinal pathologies was negatively correlated with change in weight z-score reflecting reduced interval weight gain from birth to early childhood. This association highlights the need to better understand the effects of early antimicrobial exposure on early childhood health.
Figure 1: Study population
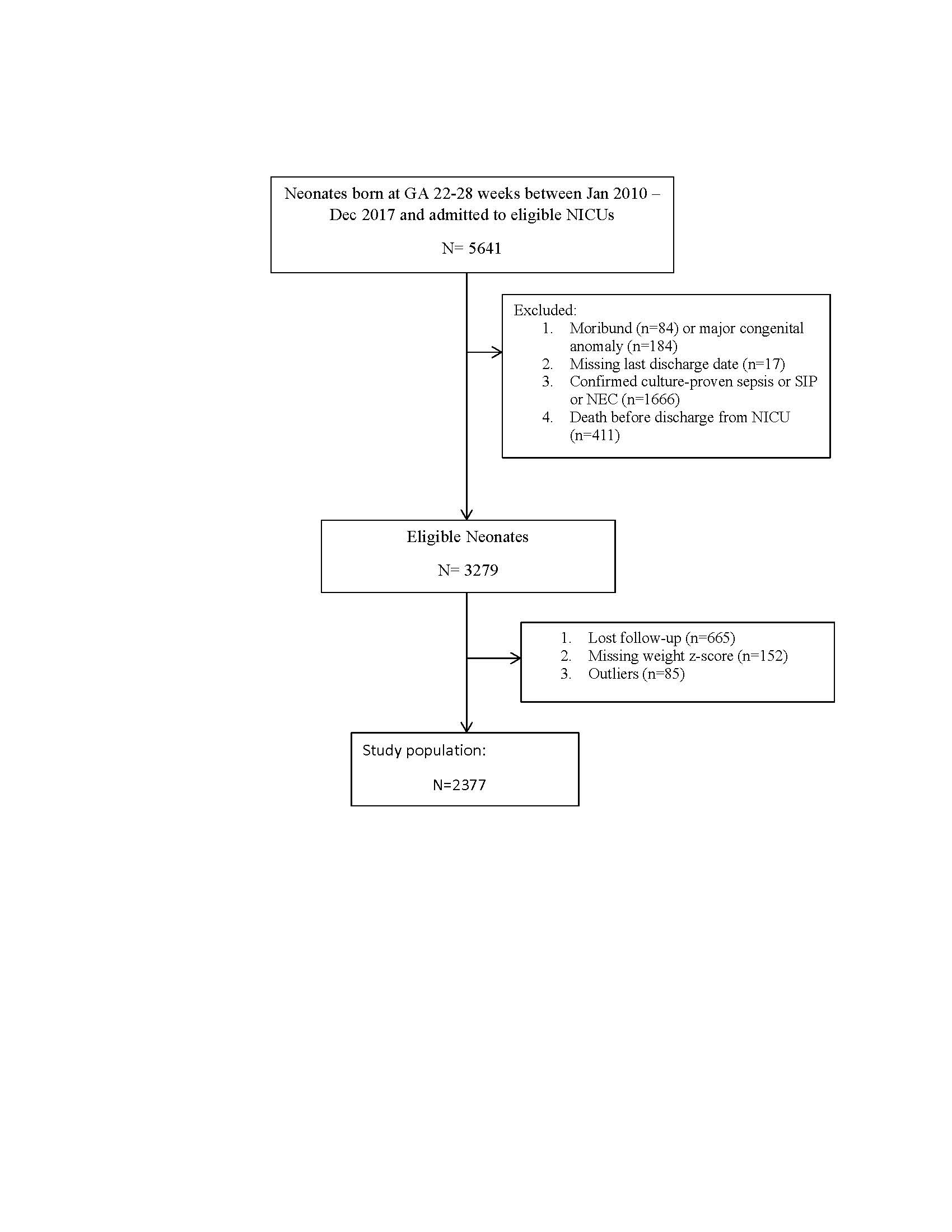
Figure 2: Linear relationship between ΔWT z-score and AUR for all infants
.jpg)
