Neonatal Neurology: Clinical
Category: Abstract Submission
Neurology 7: Neonatal Neurology Term Imaging
349 - Early impairment of metabolic-oxygenation reactivity index relates to neurological outcome following neonatal encephalopathy.
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 349
Publication Number: 349.443
Publication Number: 349.443
Kelly Harvey-Jones, University College London, UK, London, England, United Kingdom; Frédéric Lange, University College London, London, England, United Kingdom; Alan Bainbridge, University College London Hospitals, London, England, United Kingdom; Gemma Bale, University of Cambridge, Cambridge, England, United Kingdom; Francisco Torrealdea, Uclh, London, England, United Kingdom; Magdalena Sokolska, UCLH, London, England, United Kingdom; Giles S. Kendall, University College London, London, England, United Kingdom; Nicola J. Robertson, University College London, Bicester, England, United Kingdom; Ilias TACHTSIDIS, University College London, London, England, United Kingdom; Subhabrata Mitra, Institute for Women's Health, University College London, London, England, United Kingdom

Kelly Harvey-Jones, MBBS
Clinical research fellow
University College London
London, England, United Kingdom
Presenting Author(s)
Background:
The long-term sequalae of neonatal encephalopathy (NE) remains a significant worldwide problem (1). An early cot-side biomarker that provides injury stratification and predicts neurological outcome would support current and emerging neuroprotective strategies. Autoregulatory and metabolic dysfunction underpin NE, and previous work using broadband near-infrared spectroscopy (BNIRS), which monitors real-time changes in mitochondrial metabolism (oxCCO) and cerebral oxygenation (HbD), demonstrates that pressure passive cerebral metabolism at 48h of life predicts poor neurological outcome (2). In a recent animal model of NE, by combining BNIRS with diffuse correlation spectroscopy (DCS) in an advanced hybrid platform, additionally monitoring brain perfusion, we have demonstrated earlier metabolic and haemodynamic reactivity indices can predict injury severity and neurological outcome (3).
Objective:
Utilising the same novel neuromonitoring platform in this clinical study of NE, we hypothesised that optical reactivity indices on day one would predict neurological outcome.
Design/Methods:
Continuous BNIRS-DCS monitoring was performed in 11 newborns undergoing therapeutic hypothermia for NE in a tertiary neonatal unit within the first 18 hours of age (average length of monitoring was 5.4 hours). Reactivity indices were calculated using wavelet analysis to determine mean semblance scores (phase difference of slow wave oscillations) between oxCCO and HbD over one hour (2). Babies underwent MR imaging and proton MR spectroscopy in a 3T scanner between day 4 and 8 of life. Thalamic Lac/NAA was used as the primary outcome biomarker for neurological outcome as per the national guidance (4,5).
Results:
A linear regression analysis revealed a significant correlation between oxCCO-HbD semblance (metabolic-oxygenation reactivity) and thalamic Lac/NAA score (p=0.026, r2 0.48) (fig 1) with rising semblance scores denoting increasingly impaired reactivity and higher lac/NAA denoting poorer neurological outcome. Other haemodynamic reactivity indices didn’t reveal any significant relationship during this period with thalamic lac/NAA.
Conclusion(s):
Early impairment of cerebral metabolic-oxygenation reactivity was associated with worsening neurological outcome in a clinical cohort undergoing therapeutic hypothermia for NE. This study suggests an early cot-side optical monitoring tool to support management and prognostication of this disease as well as future clinical trials for emerging neuroprotective therapies.
Fig 1. Day 1 Metabolic-oxygenation reactivity vs neurological outcome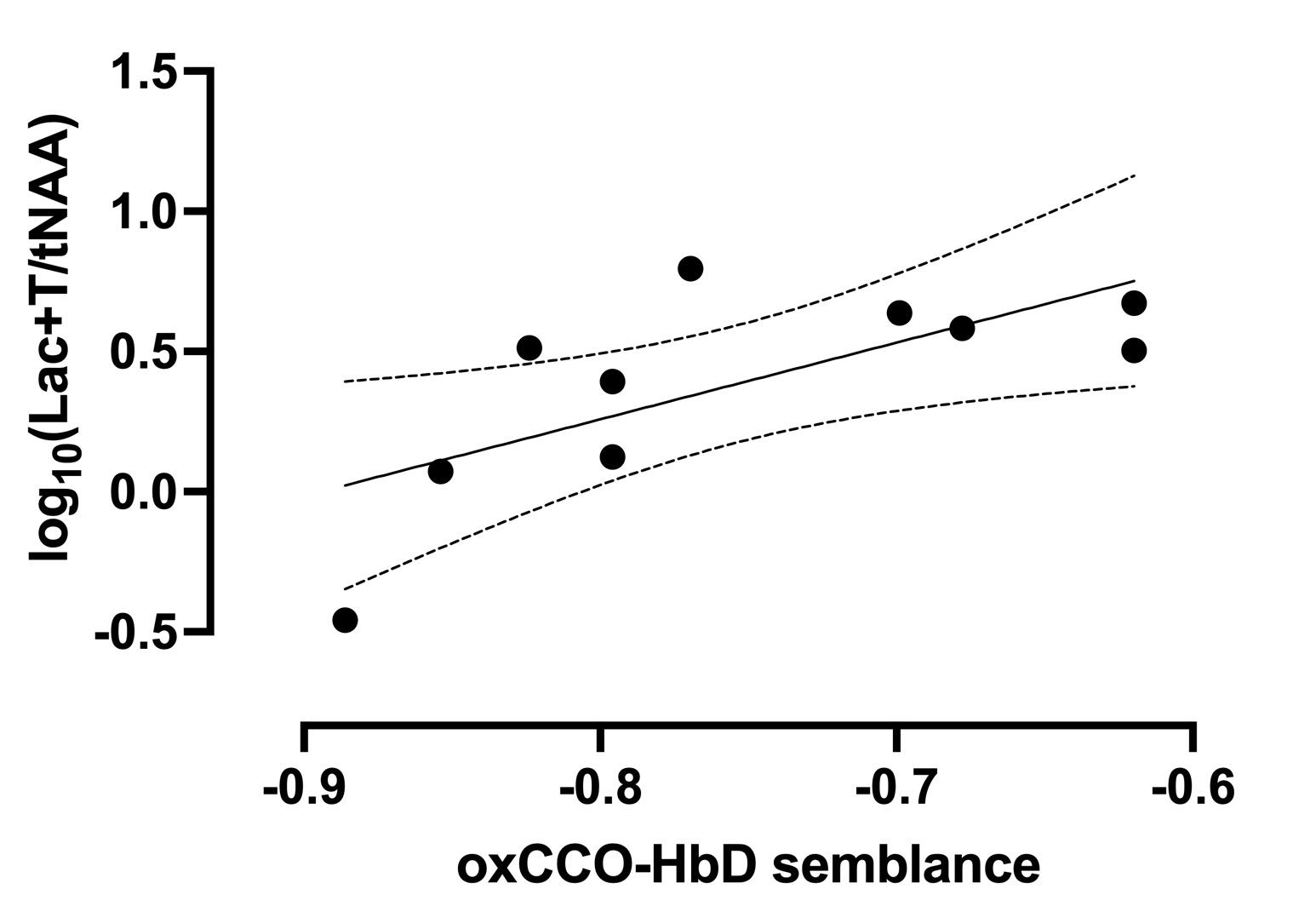 Linear regression analysis between oxCCO-HbD semblance and thalamic Lac/NAA, p=0.026 r2 0.48
Linear regression analysis between oxCCO-HbD semblance and thalamic Lac/NAA, p=0.026 r2 0.48
The long-term sequalae of neonatal encephalopathy (NE) remains a significant worldwide problem (1). An early cot-side biomarker that provides injury stratification and predicts neurological outcome would support current and emerging neuroprotective strategies. Autoregulatory and metabolic dysfunction underpin NE, and previous work using broadband near-infrared spectroscopy (BNIRS), which monitors real-time changes in mitochondrial metabolism (oxCCO) and cerebral oxygenation (HbD), demonstrates that pressure passive cerebral metabolism at 48h of life predicts poor neurological outcome (2). In a recent animal model of NE, by combining BNIRS with diffuse correlation spectroscopy (DCS) in an advanced hybrid platform, additionally monitoring brain perfusion, we have demonstrated earlier metabolic and haemodynamic reactivity indices can predict injury severity and neurological outcome (3).
Objective:
Utilising the same novel neuromonitoring platform in this clinical study of NE, we hypothesised that optical reactivity indices on day one would predict neurological outcome.
Design/Methods:
Continuous BNIRS-DCS monitoring was performed in 11 newborns undergoing therapeutic hypothermia for NE in a tertiary neonatal unit within the first 18 hours of age (average length of monitoring was 5.4 hours). Reactivity indices were calculated using wavelet analysis to determine mean semblance scores (phase difference of slow wave oscillations) between oxCCO and HbD over one hour (2). Babies underwent MR imaging and proton MR spectroscopy in a 3T scanner between day 4 and 8 of life. Thalamic Lac/NAA was used as the primary outcome biomarker for neurological outcome as per the national guidance (4,5).
Results:
A linear regression analysis revealed a significant correlation between oxCCO-HbD semblance (metabolic-oxygenation reactivity) and thalamic Lac/NAA score (p=0.026, r2 0.48) (fig 1) with rising semblance scores denoting increasingly impaired reactivity and higher lac/NAA denoting poorer neurological outcome. Other haemodynamic reactivity indices didn’t reveal any significant relationship during this period with thalamic lac/NAA.
Conclusion(s):
Early impairment of cerebral metabolic-oxygenation reactivity was associated with worsening neurological outcome in a clinical cohort undergoing therapeutic hypothermia for NE. This study suggests an early cot-side optical monitoring tool to support management and prognostication of this disease as well as future clinical trials for emerging neuroprotective therapies.
Fig 1. Day 1 Metabolic-oxygenation reactivity vs neurological outcome
 Linear regression analysis between oxCCO-HbD semblance and thalamic Lac/NAA, p=0.026 r2 0.48
Linear regression analysis between oxCCO-HbD semblance and thalamic Lac/NAA, p=0.026 r2 0.48