Neonatal Neurology: Clinical
Category: Abstract Submission
Neurology 7: Neonatal Neurology Term Imaging
343 - Abnormal neuroimaging findings in infants evaluated for but not treated with therapeutic hypothermia
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 343
Publication Number: 343.443
Publication Number: 343.443
Kirsten Thiim, Brigham and Women's Hospital, Boston, MA, United States; Sarah S. Lee, Harvard Medical School, Boston, MA, United States; Elizabeth Singh, Brigham and Women's Hospital, Boston, MA, United States; Aisling A. Garvey, INFANT Research Centre, Boston, MA, United States; Tina M. Steele, Brigham and Women's Hospital, Boston, MA, United States; Hoda Elshibiny, Birgham and Women's Hospital, Boston, MA, United States; Terrie E. Inder, Harvard Medical School, Boston, MA, United States; Mohamed El-Dib, Harvard Medical School, Boston, MA, United States
- KT
Kirsten Thiim, BS
Research Assistant
Brigham and Women's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Therapeutic hypothermia (TH) is the standard of care for neonatal encephalopathy (NE). In recent years, many centers, including ours at Brigham and Women’s Hospital (BWH), have broadened their TH treatment criteria to include infants with mild NE. Our protocol uses both history of perinatal insult (e.g. sentinel event, low Apgars, resuscitation) and a quantitative Neonatal Encephalopathy Score (NES) of four or more to decide on TH treatment eligibility. Amplitude integrated EEG (aEEG) is also used as an adjunct in evaluation. Whether these criteria, inclusive of mild encephalopathy, are capable of screening out those with no acute brain injury who might benefit from TH is unknown.
Objective: Our primary aim was to evaluate short-term MRI outcomes in infants evaluated for TH.
Design/Methods: We enrolled infants who were screened for but not treated with TH between April 2019 and August 2021. All brain MRIs were obtained within the first week of life at a BWH in-hospital scanner and MRI reports were used in the analysis.
Results: Thirty-nine infants were enrolled in the study with their detailed demographic and clinical characteristics reported in Table 1. Of the 39 infants, 34 (87.2%) had no evidence of acute perinatally acquired hypoxic ischemic brain injury. Three of these infants had evidence of chronic punctate white matter injury, and one infant showed a medullary tumor incidental finding. Five infants (12.8%) had MRI findings suggestive of acute brain injury displayed by acute diffusion weighted imaging. Three of these cases were small foci of restricted diffusion in the fronto-parietal white matter. The fourth case displayed restriction focally in the left posterior cerebral artery territory. The fifth case displayed acute watershed ischemic injury most notably in the left parieto-occipital lobe. Clinical characteristics, MRI findings, and aEEG patterns of these five cases are displayed in Table 2.Conclusion(s): Results suggest that the current expanded TH criteria, inclusive of mild NE, is effective at detecting most infants with acute hypoxic ischemic injuries. Notably, two infants with more significant injury displayed a posterior predominant lesion suggesting that clinical exam and aEEG may be less reliable for such focal lesions. Application of neuroimaging in infants considered for cooling but not receiving treatment remains worthy of consideration.
Table 1.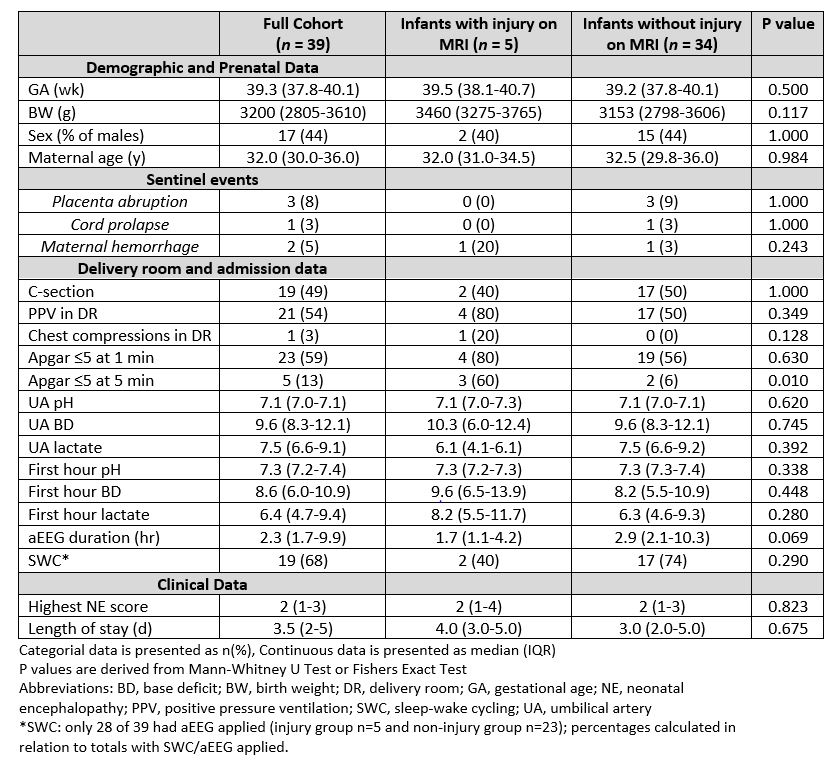 Demographical and clinical characteristics of the study cohort (n=39).
Demographical and clinical characteristics of the study cohort (n=39).
Table 2.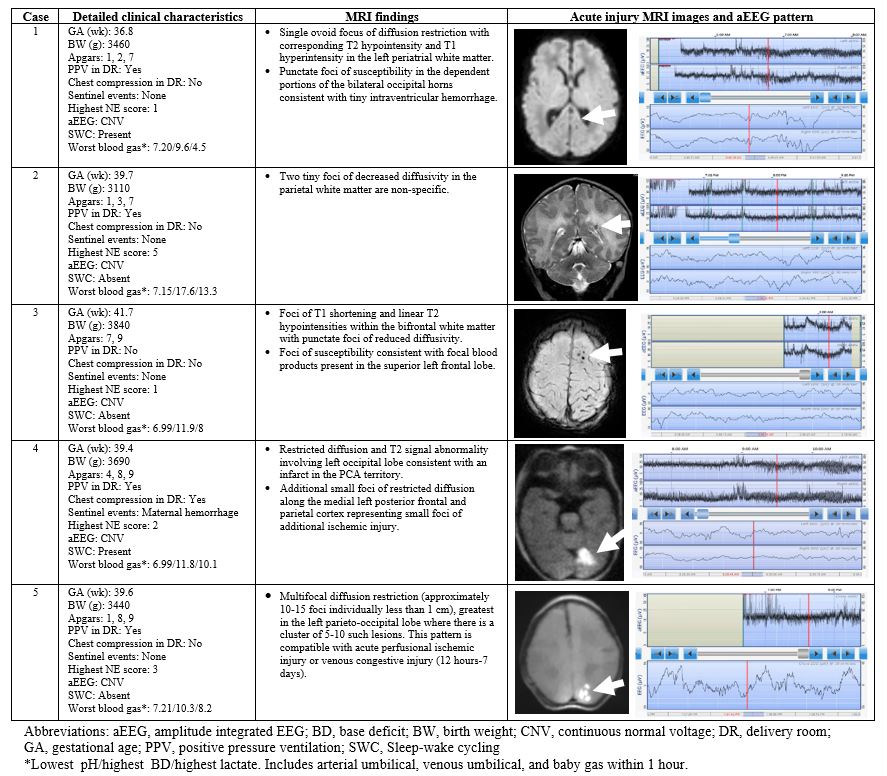 Detailed characteristics of five cases with acute injuries along with the MRI images and aEEG patterns. MRI images include case 1: Axial DWI, case 2: Coronal T2, case 3: Axial SWI, case 4: Axial DWI, and case 5: Axial DWI.
Detailed characteristics of five cases with acute injuries along with the MRI images and aEEG patterns. MRI images include case 1: Axial DWI, case 2: Coronal T2, case 3: Axial SWI, case 4: Axial DWI, and case 5: Axial DWI.
Objective: Our primary aim was to evaluate short-term MRI outcomes in infants evaluated for TH.
Design/Methods: We enrolled infants who were screened for but not treated with TH between April 2019 and August 2021. All brain MRIs were obtained within the first week of life at a BWH in-hospital scanner and MRI reports were used in the analysis.
Results: Thirty-nine infants were enrolled in the study with their detailed demographic and clinical characteristics reported in Table 1. Of the 39 infants, 34 (87.2%) had no evidence of acute perinatally acquired hypoxic ischemic brain injury. Three of these infants had evidence of chronic punctate white matter injury, and one infant showed a medullary tumor incidental finding. Five infants (12.8%) had MRI findings suggestive of acute brain injury displayed by acute diffusion weighted imaging. Three of these cases were small foci of restricted diffusion in the fronto-parietal white matter. The fourth case displayed restriction focally in the left posterior cerebral artery territory. The fifth case displayed acute watershed ischemic injury most notably in the left parieto-occipital lobe. Clinical characteristics, MRI findings, and aEEG patterns of these five cases are displayed in Table 2.Conclusion(s): Results suggest that the current expanded TH criteria, inclusive of mild NE, is effective at detecting most infants with acute hypoxic ischemic injuries. Notably, two infants with more significant injury displayed a posterior predominant lesion suggesting that clinical exam and aEEG may be less reliable for such focal lesions. Application of neuroimaging in infants considered for cooling but not receiving treatment remains worthy of consideration.
Table 1.
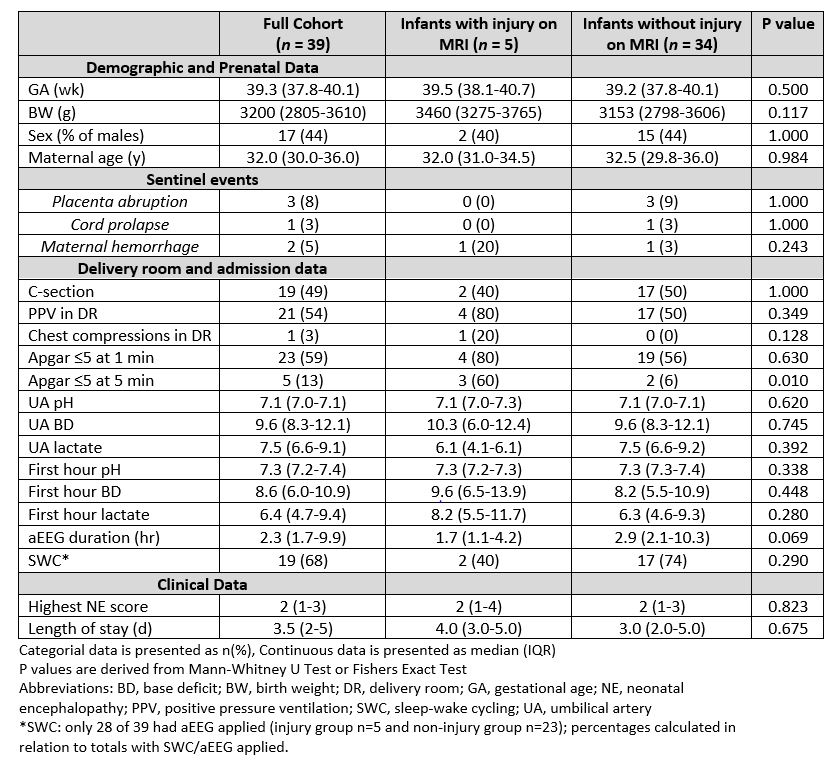 Demographical and clinical characteristics of the study cohort (n=39).
Demographical and clinical characteristics of the study cohort (n=39).Table 2.
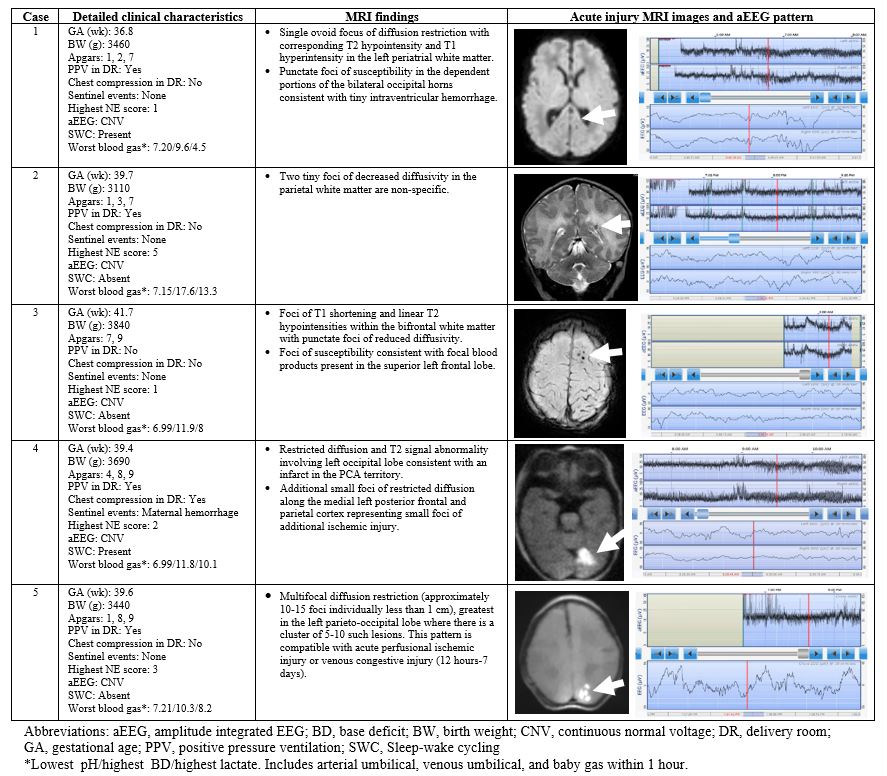 Detailed characteristics of five cases with acute injuries along with the MRI images and aEEG patterns. MRI images include case 1: Axial DWI, case 2: Coronal T2, case 3: Axial SWI, case 4: Axial DWI, and case 5: Axial DWI.
Detailed characteristics of five cases with acute injuries along with the MRI images and aEEG patterns. MRI images include case 1: Axial DWI, case 2: Coronal T2, case 3: Axial SWI, case 4: Axial DWI, and case 5: Axial DWI.