Breastfeeding/Human Milk
Category: Abstract Submission
Breastfeeding/Human Milk I
422 - Provision of Human Milk at NICU Discharge for Preterm Infants during the COVID-19 Pandemic
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 422
Publication Number: 422.301
Publication Number: 422.301
Lauren E. Boudreau, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Betty R. Vohr, Women & Infants Hospital of Rhode Island; Alpert Medical School of Brown University, Providence, SD, United States; Richard Tucker, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Elisabeth McGowan, Women & Infants Hospital of Rhode Island, Providence, RI, United States

Lauren E. Boudreau, DO
Fellow in Neonatal-Perinatal Medicine
Women & Infants Hospital of Rhode Island
Providence, Rhode Island, United States
Presenting Author(s)
Background: The mother-baby dyad faces many challenges in the COVID-19 pandemic, yet effects on the provision of human milk (HM) for preterm (PT) infants remain unclear.
Objective: To investigate the impact of the COVID-19 pandemic on provision of HM at the time of discharge (DC) home from the NICU in a cohort of survivors born < 34 weeks gestational age.
Design/Methods: Retrospective analysis of prospectively collected data from the Women & Infants Follow-up Clinic database. 532 PT infants born between 1/1/2019 and 3/30/2021 who survived to DC are included. Infants born during the COVID-19 period (defined as 3/1/20 to 4/30/21) were compared to infants born pre-COVID (defined as 1/1/19 to 2/29/20), and the primary outcome was the provision of any HM at NICU DC. Lactation support team services for NICU families were unchanged during the pandemic (Figure 1). Secondary analyses were performed by public and private insurance. Multivariable regression analyses were run for the total cohort and by health insurance, adjusting for socio-economic demographics and medical risks. An interaction term for public insurance and COVID-19 period was also tested.
Results: Infants born during the COVID-19 pandemic were larger than infants born pre-COVID (Table 1). There were more mothers who identified as single prior to pandemic onset, and more cases of chorioamnionitis after pandemic onset (Table 1). Rates of public insurance were similar between groups (55% pre-COVID and 50% COVID). There was no change in provision of any HM at DC between time periods, 63% to 71%; p=0.08 (Table 1). Provision of any HM at DC increased from 77% to 88%; p=.02 for those on private insurance and remained unchanged for infants on public insurance; 52% to 53%; p=.92 (Table 1). In regression analyses, mothers with private insurance were twice as likely to provide HM at DC during the COVID period compared to pre-COVID. OR; CI (2.07; 1.06-4.03); p=.03 (Table 2). For those on public insurance, the odds for HM provision during COVID versus pre-COVID were 0.95; 0.55-1.66; p=.85 NS, with a 2% decrease in odds for each day in the NICU (Table 2). The interaction term showed lower odds of HM for public vs private insurance during the COVID-19 period (OR 0.41; 0.17-0.98; p=0.05).Conclusion(s): Mothers with private insurance were twice as likely to provide HM at DC during the COVID-19 pandemic, whereas there was no change in provision among families with public insurance. We speculate that both the dedication of our lactation support team and health care disparities contributed to this difference in outcomes by insurance status.
Table 1: Maternal and Infant Characteristics and Medical Complications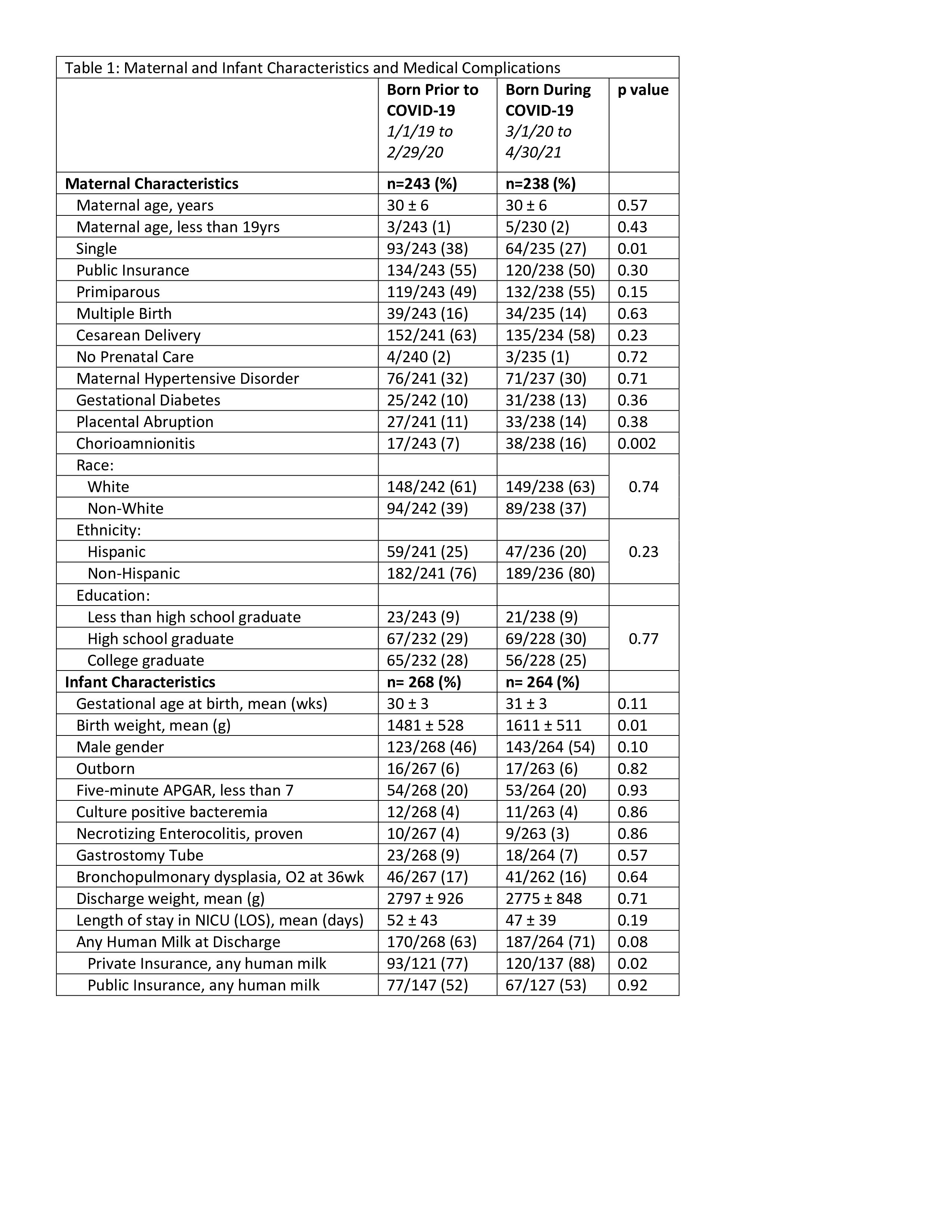
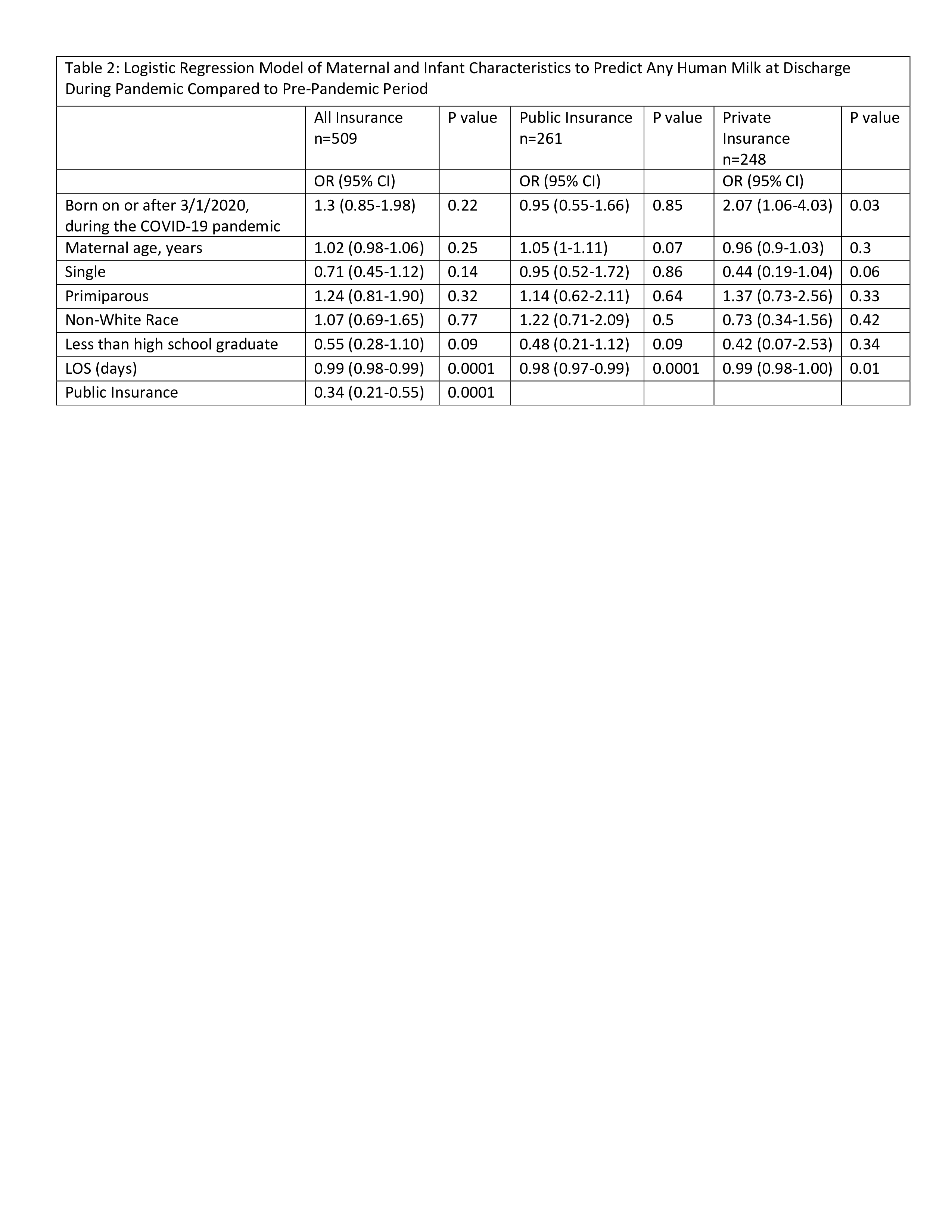
Table 2: Logistic Regression Model of Maternal and Infant Characteristics to Predict Any Human Milk at Discharge During Pandemic Compared to Pre-Pandemic Period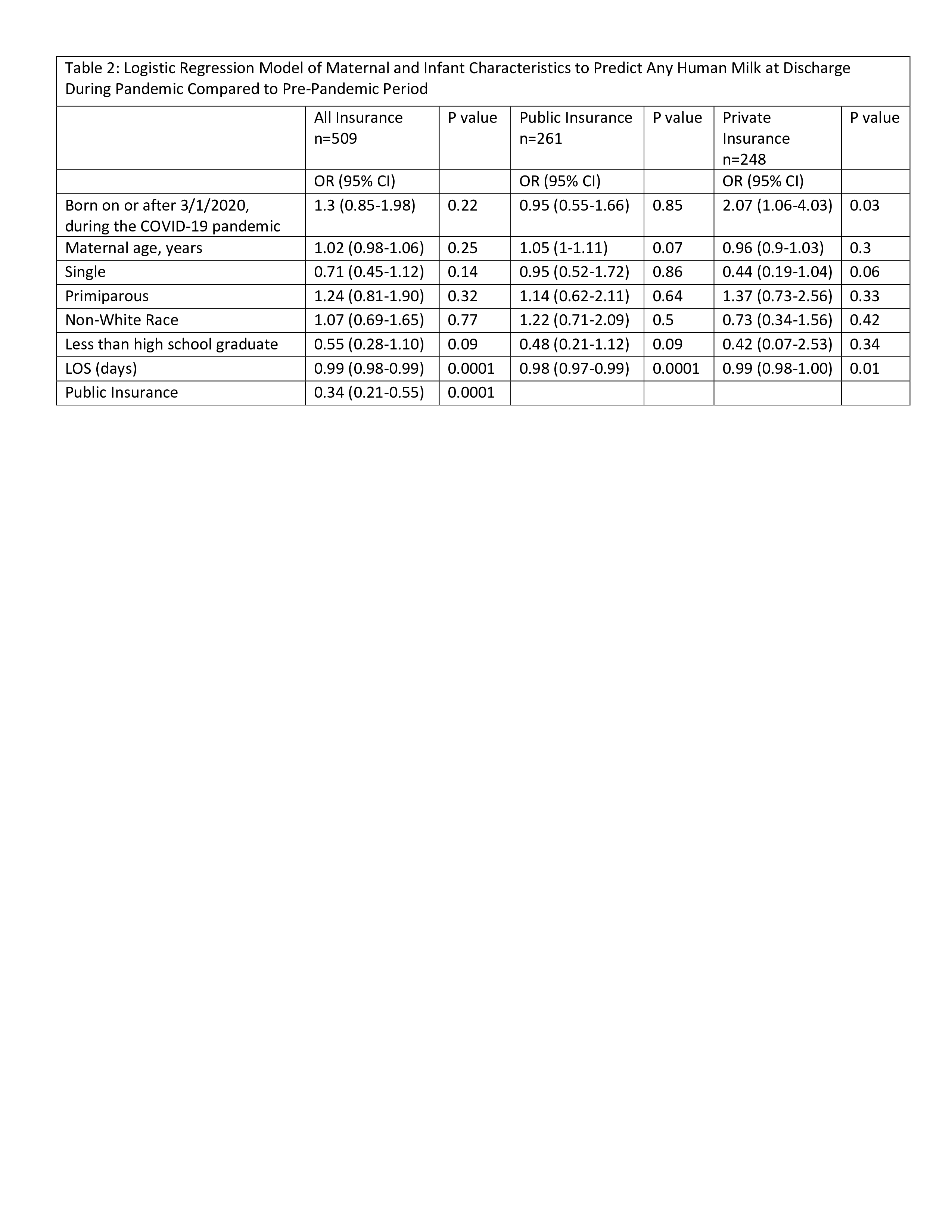
Objective: To investigate the impact of the COVID-19 pandemic on provision of HM at the time of discharge (DC) home from the NICU in a cohort of survivors born < 34 weeks gestational age.
Design/Methods: Retrospective analysis of prospectively collected data from the Women & Infants Follow-up Clinic database. 532 PT infants born between 1/1/2019 and 3/30/2021 who survived to DC are included. Infants born during the COVID-19 period (defined as 3/1/20 to 4/30/21) were compared to infants born pre-COVID (defined as 1/1/19 to 2/29/20), and the primary outcome was the provision of any HM at NICU DC. Lactation support team services for NICU families were unchanged during the pandemic (Figure 1). Secondary analyses were performed by public and private insurance. Multivariable regression analyses were run for the total cohort and by health insurance, adjusting for socio-economic demographics and medical risks. An interaction term for public insurance and COVID-19 period was also tested.
Results: Infants born during the COVID-19 pandemic were larger than infants born pre-COVID (Table 1). There were more mothers who identified as single prior to pandemic onset, and more cases of chorioamnionitis after pandemic onset (Table 1). Rates of public insurance were similar between groups (55% pre-COVID and 50% COVID). There was no change in provision of any HM at DC between time periods, 63% to 71%; p=0.08 (Table 1). Provision of any HM at DC increased from 77% to 88%; p=.02 for those on private insurance and remained unchanged for infants on public insurance; 52% to 53%; p=.92 (Table 1). In regression analyses, mothers with private insurance were twice as likely to provide HM at DC during the COVID period compared to pre-COVID. OR; CI (2.07; 1.06-4.03); p=.03 (Table 2). For those on public insurance, the odds for HM provision during COVID versus pre-COVID were 0.95; 0.55-1.66; p=.85 NS, with a 2% decrease in odds for each day in the NICU (Table 2). The interaction term showed lower odds of HM for public vs private insurance during the COVID-19 period (OR 0.41; 0.17-0.98; p=0.05).Conclusion(s): Mothers with private insurance were twice as likely to provide HM at DC during the COVID-19 pandemic, whereas there was no change in provision among families with public insurance. We speculate that both the dedication of our lactation support team and health care disparities contributed to this difference in outcomes by insurance status.
Table 1: Maternal and Infant Characteristics and Medical Complications
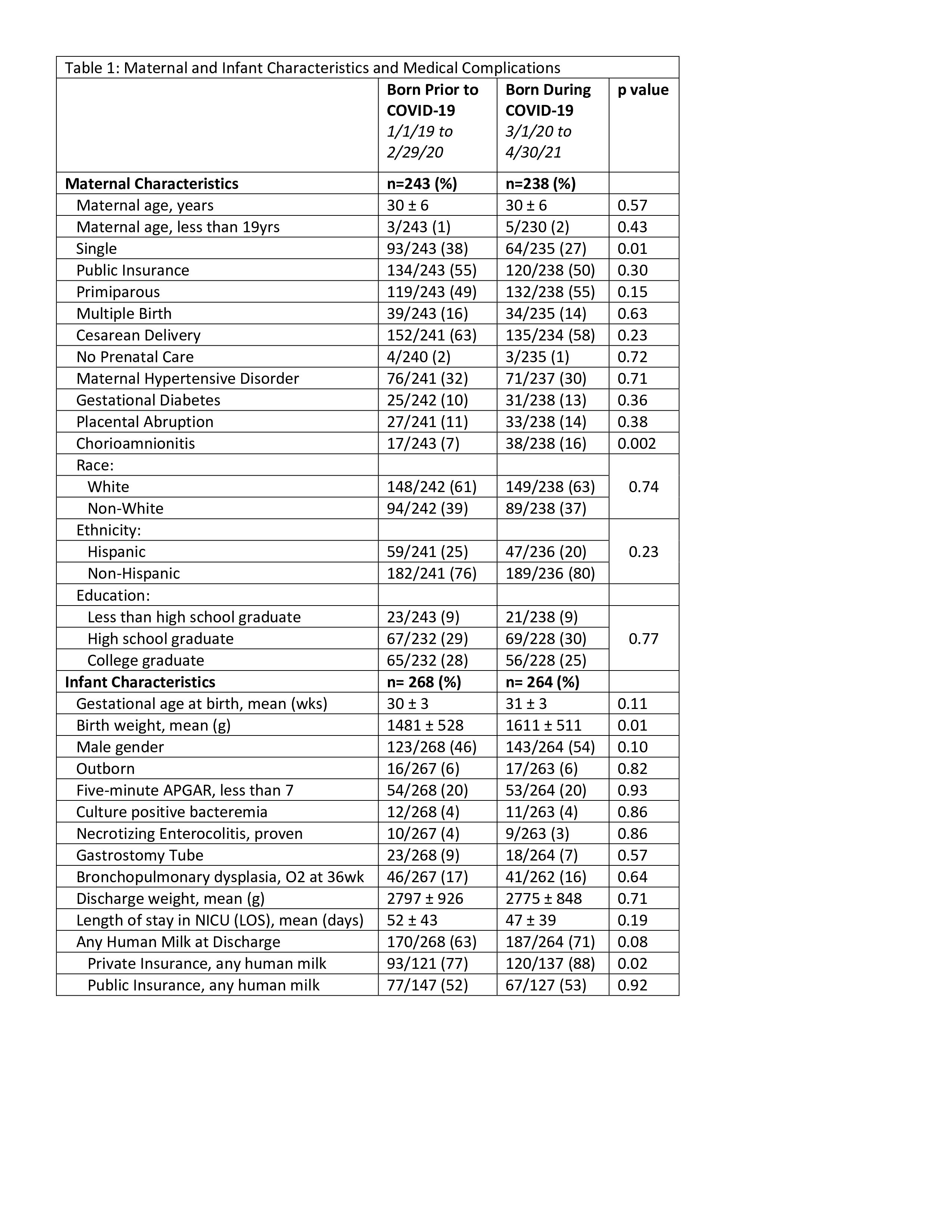
Table 2: Logistic Regression Model of Maternal and Infant Characteristics to Predict Any Human Milk at Discharge During Pandemic Compared to Pre-Pandemic Period