Hospital Medicine: Hospital Medicine Quality Improvement
Category: Abstract Submission
Hospital Medicine: QI
331 - Improving Documentation of Reaction Characteristics for Pediatric Inpatients with a History of Penicillin and Cephalosporin Allergies: A Step Towards Better Antibiotic Stewardship
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 331
Publication Number: 331.323
Publication Number: 331.323
Stephanie Prudencio, University of Florida College of Medicine - Jacksonville, Jacksonville, FL, United States; Lisa M. Awe, University of Florida College of Medicine, Saint Johns, FL, United States; Matthew D. Garber, University of Florida Jacksonville/Wolfson CH, JACKSONVILLE, FL, United States; Ana M. Alvarez, University of Florida College of Medicine, Jacksonville, FL, United States

Stephanie Prudencio, DO
Resident Physician
University of Florida College of Medicine - Jacksonville
Jacksonville, Florida, United States
Presenting Author(s)
Background: 10% of children have a reported penicillin allergy, but most are found not to be truly allergic when formally tested. Cephalosporin allergy is presumed despite mostly low levels of cross-reactivity for individual drugs. Allergy reaction characteristics help determine the risk for a true allergy. This risk can guide the appropriate setting and precautions for drug challenge. Erroneous allergy labels promote unnecessary broad spectrum antibiotic use which increases cost and bacterial resistance.
Objective: Our global aim was to improve antibiotic stewardship by avoiding unnecessary broad spectrum antibiotics given because of reported allergy. Our specific aim was to increase the percentage of patients admitted to Wolfson Children’s Hospital with a reported penicillin or cephalosporin allergy who had reaction symptoms documented to 80% by December 2021.
Design/Methods: We reviewed baseline data from 2020. In February 2021, we proposed our QI initiative to hospital leadership. Bedside nurses and nursing leaders collaborated with the team to develop flyers outlining appropriate reaction characteristics and the documentation process (Figure 1). We presented these flyers during morning and evening bedside nursing huddles on four Med-Surg floors and provided updates to the Antibiotic Stewardship Committee. We developed a tool for risk classification and presented a Noon Conference on focused allergy history and antibiotic selection. In lieu of a balancing measure, we informally surveyed bedside nurses on their perceptions of the new process. We also developed protocols to educate families about current and future antibiotic use.
Results: In the baseline period, 40% percent of patients had reaction characteristics documented. This increased to 80% by October 2021 (Figure 2). Special cause variation was noted in August 2021, 2 months after our major intervention with nursing. Nurses reported a good understanding of the project rationale and the documentation process which was generally quick and not overly burdensome.Conclusion(s): We achieved our goal of 80% documentation of allergy reaction characteristics. We believe nursing participation increased buy in and created a streamlined process that matched workflow and routines, especially since this occurred during our busiest COVID-19 surge in July to October 2021. We are tracking but have not yet analyzed documentation through a smart phrase of hospitalist recommendations to families or outpatient providers about future antibiotic restrictions or evaluations. We are also tracking patients whose inpatient antibiotics were broadened based on low-risk reactions.
Figure 1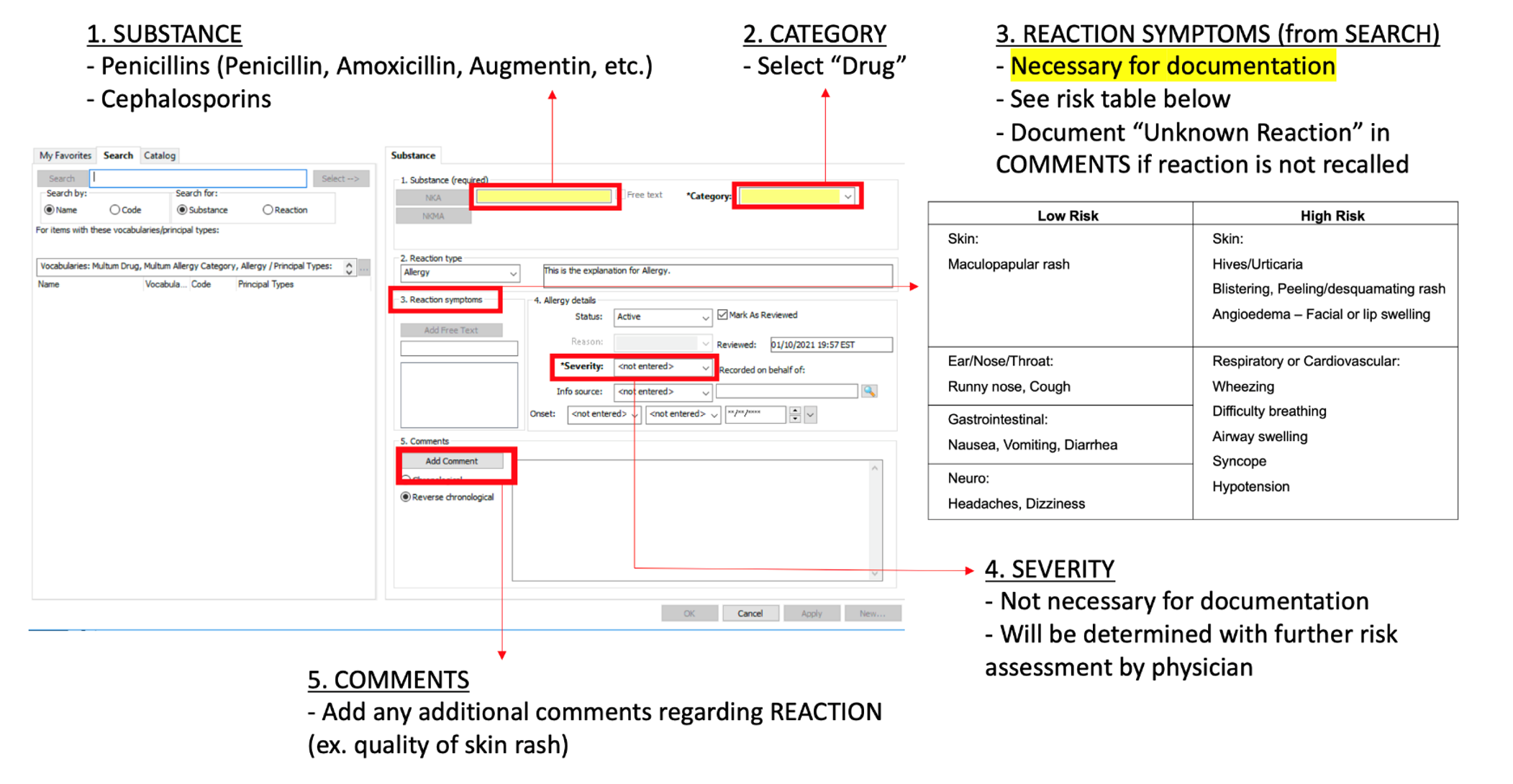 Flyer outlining documentation of drug allergy reaction characteristics
Flyer outlining documentation of drug allergy reaction characteristics
Figure 2.png) P-chart. Percentage of patients with documented drug allergy reaction characteristics
P-chart. Percentage of patients with documented drug allergy reaction characteristics
Objective: Our global aim was to improve antibiotic stewardship by avoiding unnecessary broad spectrum antibiotics given because of reported allergy. Our specific aim was to increase the percentage of patients admitted to Wolfson Children’s Hospital with a reported penicillin or cephalosporin allergy who had reaction symptoms documented to 80% by December 2021.
Design/Methods: We reviewed baseline data from 2020. In February 2021, we proposed our QI initiative to hospital leadership. Bedside nurses and nursing leaders collaborated with the team to develop flyers outlining appropriate reaction characteristics and the documentation process (Figure 1). We presented these flyers during morning and evening bedside nursing huddles on four Med-Surg floors and provided updates to the Antibiotic Stewardship Committee. We developed a tool for risk classification and presented a Noon Conference on focused allergy history and antibiotic selection. In lieu of a balancing measure, we informally surveyed bedside nurses on their perceptions of the new process. We also developed protocols to educate families about current and future antibiotic use.
Results: In the baseline period, 40% percent of patients had reaction characteristics documented. This increased to 80% by October 2021 (Figure 2). Special cause variation was noted in August 2021, 2 months after our major intervention with nursing. Nurses reported a good understanding of the project rationale and the documentation process which was generally quick and not overly burdensome.Conclusion(s): We achieved our goal of 80% documentation of allergy reaction characteristics. We believe nursing participation increased buy in and created a streamlined process that matched workflow and routines, especially since this occurred during our busiest COVID-19 surge in July to October 2021. We are tracking but have not yet analyzed documentation through a smart phrase of hospitalist recommendations to families or outpatient providers about future antibiotic restrictions or evaluations. We are also tracking patients whose inpatient antibiotics were broadened based on low-risk reactions.
Figure 1
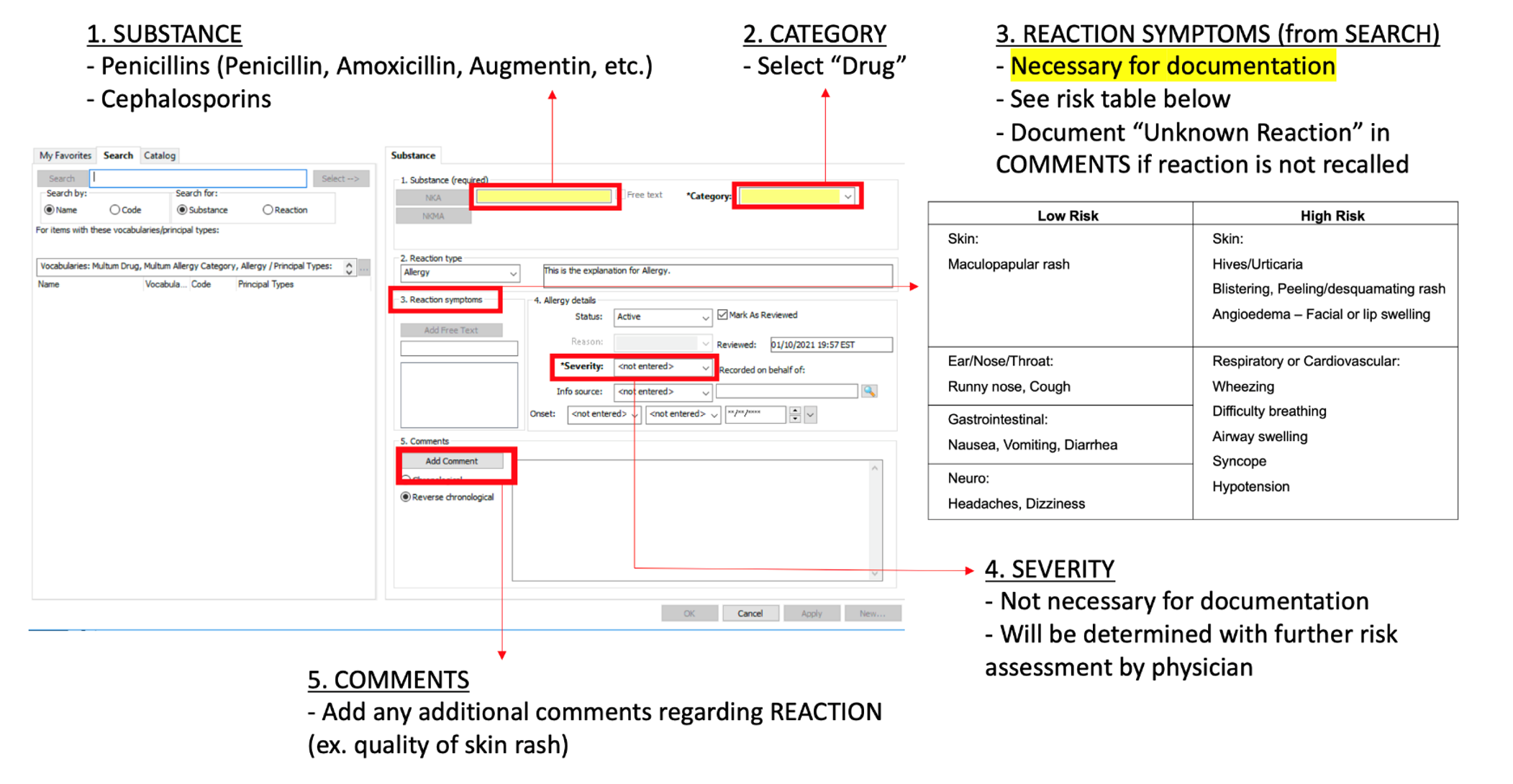 Flyer outlining documentation of drug allergy reaction characteristics
Flyer outlining documentation of drug allergy reaction characteristicsFigure 2
.png) P-chart. Percentage of patients with documented drug allergy reaction characteristics
P-chart. Percentage of patients with documented drug allergy reaction characteristics