Health Services Research
Category: Abstract Submission
Health Services Research II
204 - Deconstructing the Maternal Vulnerability Index: Examining Associations of the 6 Themes with Preterm Birth
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 204
Publication Number: 204.320
Publication Number: 204.320
Sara C. Handley, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Diana Montoya-Williams, Children’s Hospital of Philadelphia, Philadelphia, PA, United States; Molly Passarella, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Carolyn M. McGann, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Elizabeth G. Salazar, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Kathryn Paul, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Daria Murosko, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Michelle-Marie Peña, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Robin Ortiz, NYU Grossman School of Medicine, New York, NY, United States; Heather Burris, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Scott A. Lorch, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States

Sara C. Handley, MD, MSCE (she/her/hers)
Assistant Professor of Pediatrics
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: The Maternal Vulnerability Index (MVI) is a novel tool designed to quantify maternal vulnerability to adverse health outcomes. The MVI is a composite measure of 43 area-level indicators, which are categorized into 6 themes: 1) reproductive healthcare, 2) physical health, 3) mental health and substance abuse, 4) general healthcare, 5) socioeconomic determinants, and 6) physical environment. These themes reflect the varied drivers of adverse outcomes, yet the influence of each of these themes on perinatal outcomes, including preterm birth (PTB), is unknown.
Objective:
To examine associations of each of the 6 MVI themes with PTB.
Design/Methods: This is a retrospective observational cohort study of singleton infants born in 2018 at 22-44 weeks’ gestation captured in national birth certificate data. The exposure was each MVI theme for the maternal county of residence. The primary outcome was PTB ( < 37 weeks’ gestation). Associations were assessed using logistic regression without and with adjustment for perinatal and geographic characteristics, clustered by county, with state as a fixed effect. To examine geographic variation in drivers of PTB, the MVI theme most strongly associated with PTB was mapped by state.
Results: Among 3,659,099 infants, 298,847 (8.2%) were born preterm (Table 1). In the unadjusted analysis, increasing vulnerability within each theme was associated with an increased odds of PTB (Table 2). In adjusted models, very high vulnerability in community physical health, mental health and substance abuse, and general healthcare all remained significantly associated with PTB, while there was no positive association detected with reproductive healthcare, socioeconomic determinants, or physical environment (Table 2). The theme with the strongest association with PTB varied by state, though physical health (19 states) and mental health and substance abuse (16 states) were most common (Figure 1).Conclusion(s): The 6 themes comprising the MVI are all associated with PTB, with increased area-level vulnerability associated with increased PTB. Theme associations with PTB were not consistent after adjustment, suggesting differences in uniqueness, theme overlap, and the influence of additional perinatal patient characteristics. State-based variation in strongly associated themes highlights the need to tailor efforts to improve outcomes for the local population. Further study of the relationship between these themes and nuances at the county or census tract level are needed.
Table 1. Geographic and Dyad Characteristics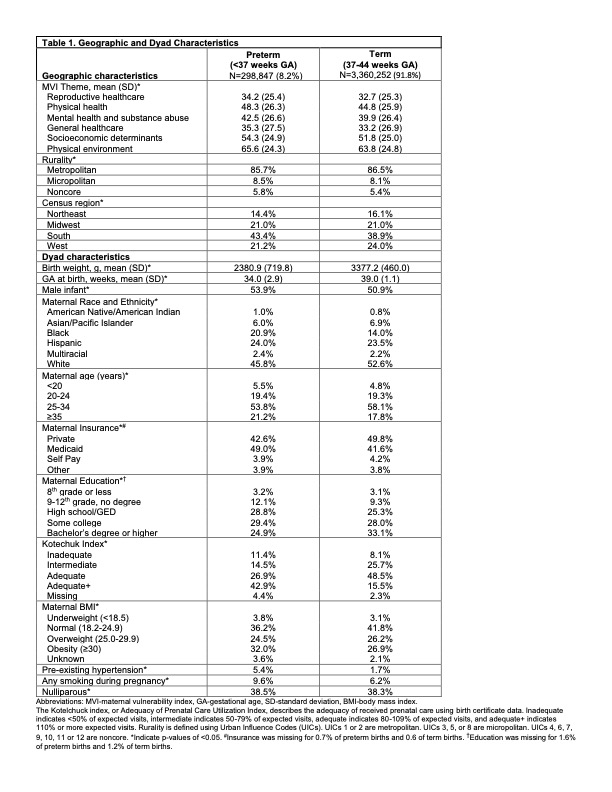
Table 2. Associations of each MVI Theme with PTB.jpg)
Objective:
To examine associations of each of the 6 MVI themes with PTB.
Design/Methods: This is a retrospective observational cohort study of singleton infants born in 2018 at 22-44 weeks’ gestation captured in national birth certificate data. The exposure was each MVI theme for the maternal county of residence. The primary outcome was PTB ( < 37 weeks’ gestation). Associations were assessed using logistic regression without and with adjustment for perinatal and geographic characteristics, clustered by county, with state as a fixed effect. To examine geographic variation in drivers of PTB, the MVI theme most strongly associated with PTB was mapped by state.
Results: Among 3,659,099 infants, 298,847 (8.2%) were born preterm (Table 1). In the unadjusted analysis, increasing vulnerability within each theme was associated with an increased odds of PTB (Table 2). In adjusted models, very high vulnerability in community physical health, mental health and substance abuse, and general healthcare all remained significantly associated with PTB, while there was no positive association detected with reproductive healthcare, socioeconomic determinants, or physical environment (Table 2). The theme with the strongest association with PTB varied by state, though physical health (19 states) and mental health and substance abuse (16 states) were most common (Figure 1).Conclusion(s): The 6 themes comprising the MVI are all associated with PTB, with increased area-level vulnerability associated with increased PTB. Theme associations with PTB were not consistent after adjustment, suggesting differences in uniqueness, theme overlap, and the influence of additional perinatal patient characteristics. State-based variation in strongly associated themes highlights the need to tailor efforts to improve outcomes for the local population. Further study of the relationship between these themes and nuances at the county or census tract level are needed.
Table 1. Geographic and Dyad Characteristics
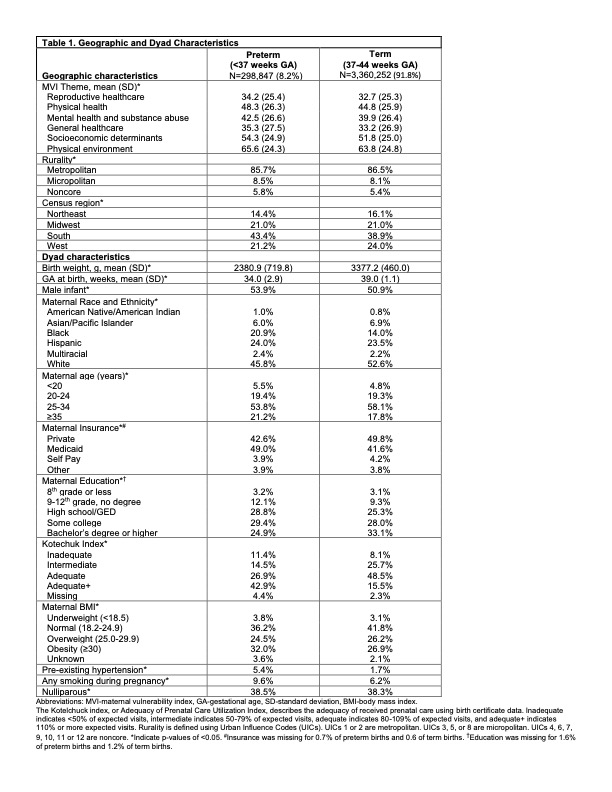
Table 2. Associations of each MVI Theme with PTB
.jpg)
