Breastfeeding/Human Milk
Category: Abstract Submission
Breastfeeding/Human Milk I
414 - Development and Efficacy of a NICU/PICU Breastfeeding Champion Course
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 414
Publication Number: 414.301
Publication Number: 414.301
Sarah Jordan-Crowe, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Julie Patterson, Northern Illinois University, DeKalb, IL, United States; Stacia Tietje, Northern Illinois University, DeKalb, IL, United States; Stephanie J. Attarian, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States

Sarah Jordan-Crowe, MD
Neonatal/Perinatal Medicine Fellow
UH Rainbow Babies & Children's Hospital
Cleveland, Ohio, United States
Presenting Author(s)
Background: The use of mother’s own milk (MOM) partially mitigates preterm infants’ increased risk of morbidities such as sepsis, retinopathy of prematurity, and delayed growth and neurodevelopment. Mother/infant dyads in the intensive care unit setting have unique lactation needs and challenges. Currently there are no Neonatal Intensive Care Unit (NICU) and Pediatric Intensive Care Unit (PICU) professional lactation support training programs available for health care providers (HCPs).
Objective: Develop, implement, and evaluate a NICU/PICU lactation support course for HCPs.
Design/Methods: Multidisciplinary expert team at the Institute for Advancement of Breastfeeding and Lactation Education (IABLE) developed a 5.25 hour-long course. Course was advertised via IABLE and the Academy of Breastfeeding Medicine. The program was administered live to over 300 participants with an additional 260 participants who watched a recorded version. All course participants were invited to complete assessments administered before and after completing the course. Assessments contained 6 case study scenarios with a series of re-occurring questions to assess participants’ capabilities, opportunities, and motivations (the COM-B theoretical construct) to engage in providing lactation support using a 5-point Likert scale. An additional 10 open-ended questions were included along with demographic characteristics. Significance assessed using binomial test.
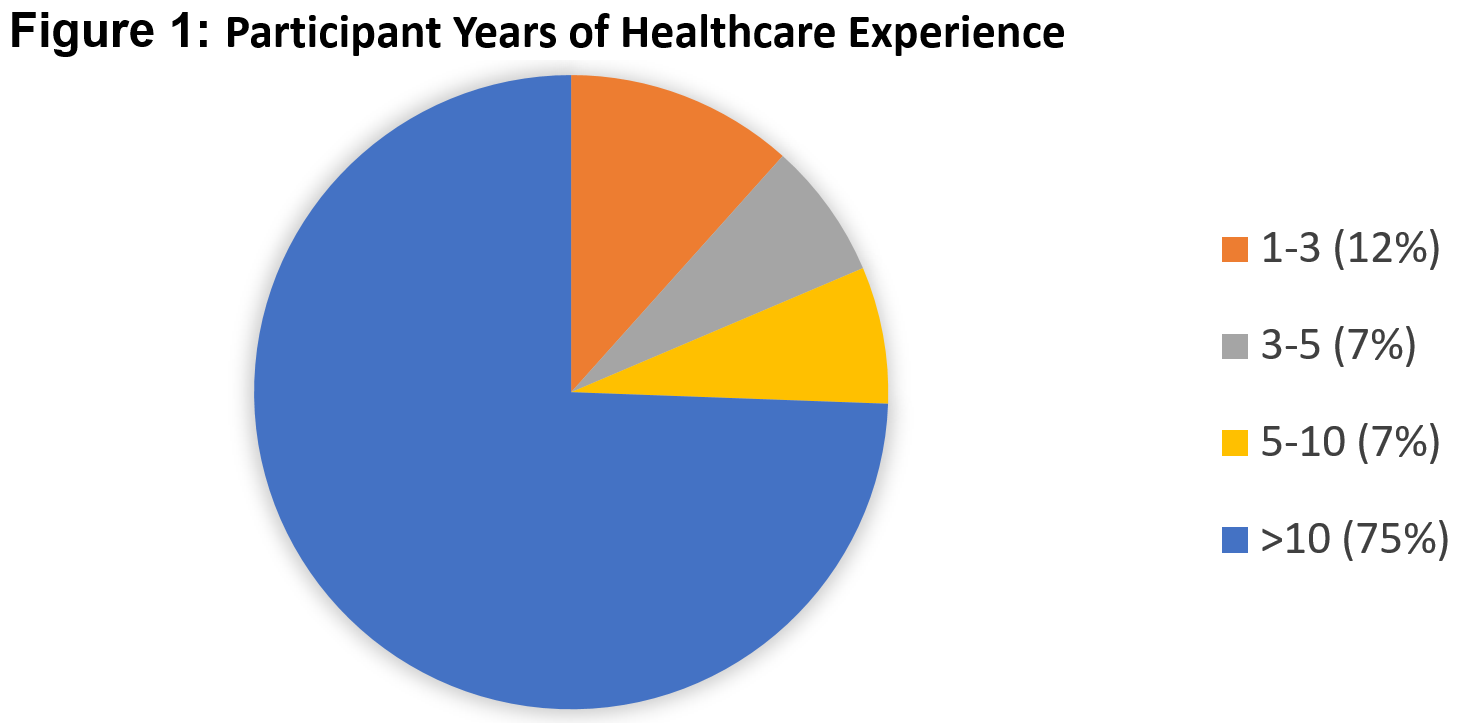
Results: Of 560 course participants, 168 completed the pre-survey and 99 completed the post-survey. Participants pre- and post- surveys were matched (n=45) for comparison using a unique identifier. Of those, 33% had received their International Board Certified Lactation Consultant (IBCLC) certification and 24% had received other lactation certification. Seventy-one percent of respondents had been in healthcare for over 10 years and 80% had received more than 19 hours of breastfeeding education in the past three years. (Figure 1) Providers showed an increase in confidence in multiple areas such as assessing for contraindications to MOM (85%, p=0.02), positioning and latch (85%, p=0.02), hypoglycemia (75%, p=0.01), and maintenance of milk production (75%, p=0.04). (Table 1)Conclusion(s): The course increased confidence of HCPs in managing a variety of areas specific to neonatal breastfeeding medicine, despite the majority of them having received certification in lactation and practicing for >10 years. These findings may indicate need for lactation curriculums to include additional information specific to intensive care population.
CV - Sarah Jordan-CroweCV - Sarah Jordan-Crowe.pdf
Figure 1: Participant Years of Healthcare Experience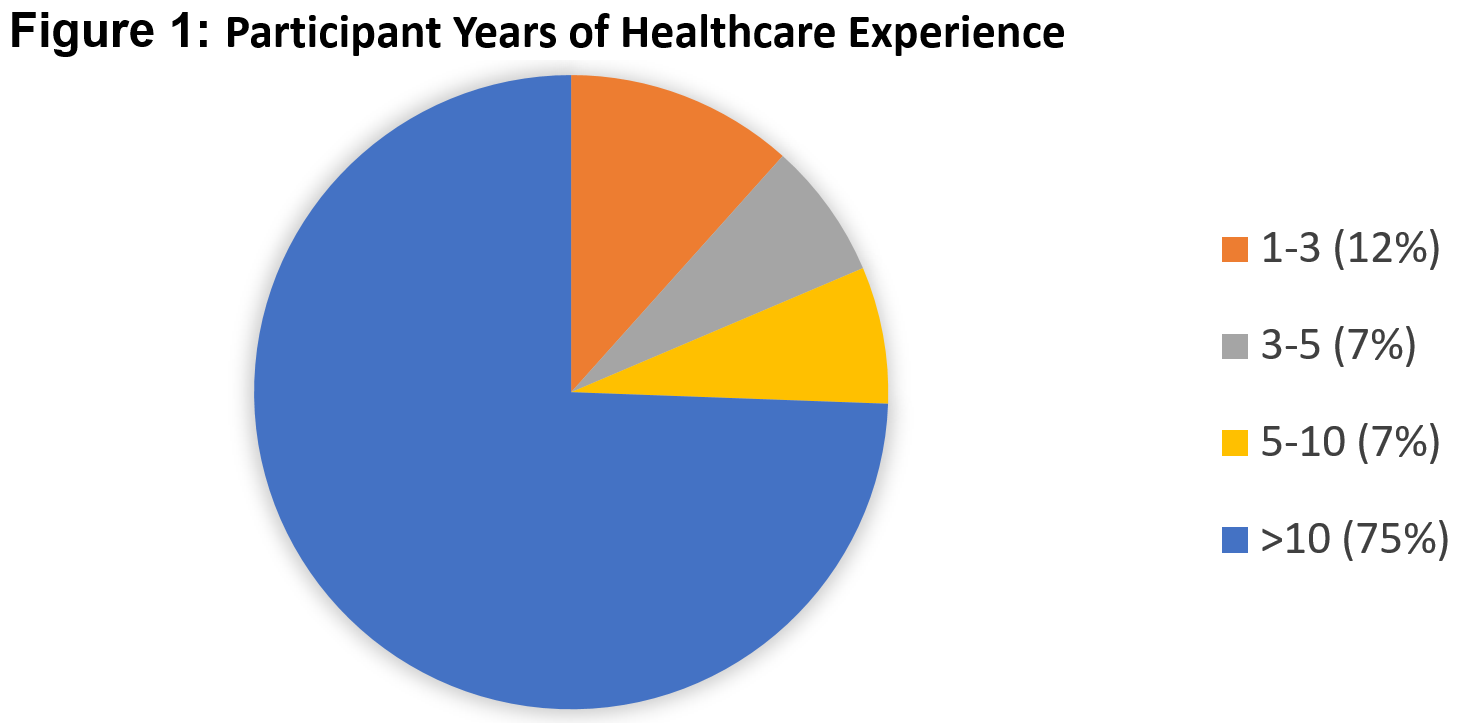
Objective: Develop, implement, and evaluate a NICU/PICU lactation support course for HCPs.
Design/Methods: Multidisciplinary expert team at the Institute for Advancement of Breastfeeding and Lactation Education (IABLE) developed a 5.25 hour-long course. Course was advertised via IABLE and the Academy of Breastfeeding Medicine. The program was administered live to over 300 participants with an additional 260 participants who watched a recorded version. All course participants were invited to complete assessments administered before and after completing the course. Assessments contained 6 case study scenarios with a series of re-occurring questions to assess participants’ capabilities, opportunities, and motivations (the COM-B theoretical construct) to engage in providing lactation support using a 5-point Likert scale. An additional 10 open-ended questions were included along with demographic characteristics. Significance assessed using binomial test.
Results: Of 560 course participants, 168 completed the pre-survey and 99 completed the post-survey. Participants pre- and post- surveys were matched (n=45) for comparison using a unique identifier. Of those, 33% had received their International Board Certified Lactation Consultant (IBCLC) certification and 24% had received other lactation certification. Seventy-one percent of respondents had been in healthcare for over 10 years and 80% had received more than 19 hours of breastfeeding education in the past three years. (Figure 1) Providers showed an increase in confidence in multiple areas such as assessing for contraindications to MOM (85%, p=0.02), positioning and latch (85%, p=0.02), hypoglycemia (75%, p=0.01), and maintenance of milk production (75%, p=0.04). (Table 1)Conclusion(s): The course increased confidence of HCPs in managing a variety of areas specific to neonatal breastfeeding medicine, despite the majority of them having received certification in lactation and practicing for >10 years. These findings may indicate need for lactation curriculums to include additional information specific to intensive care population.
CV - Sarah Jordan-CroweCV - Sarah Jordan-Crowe.pdf
Figure 1: Participant Years of Healthcare Experience