Neonatal General
Category: Abstract Submission
Neonatology General 4
397 - Quality of Death of Actively Treated Extremely Premature Infants
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 397
Publication Number: 397.134
Publication Number: 397.134
Lyubov Tiegs, Medical College of Wisconsin, Wauwatosa, WI, United States; Erin Rholl, Children's National Hospital, Washington, DC, United States; Siobhan M. McDonnell, Medical College of Wisconsin, Germantown, WI, United States; Jacquelyn Paradise, Children's Hospital of Wisconsin, Franklin, WI, United States; Michael Uhing, Medical College of Wisconsin, Milwaukee, WI, United States; Mir A. Basir, Medical College of Wisconsin, Wauwatosa, WI, United States
Lyubov (Libby) Tiegs, B.S., B.A.
Medical Student
Medical College of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
Background: For extremely premature infants (EPI) at the edge of viability, there is equipoise regarding the benefits and harms of intensive care (IC) treatment at birth. The Neonatal Research Network and other organizations publish outcome data for EPI who survive with IC treatment to inform clinician and parent treatment decisions. However, a similar number of EPI survive or die with IC treatment, but little information is disseminated about the experiences of EPI who die. The experienced pain and quality of death are important considerations when parents make treatment choices for their children.
Objective: Determine if EPI who die with IC face more treatment-associated negative experiences over the same time frame than EPI who survive.
Design/Methods: We designed a 1:1 case-control study and screened medical records of all inborn 22 to 25 weeks gestational age (GA) infants admitted to the neonatal intensive care unit (NICU) from 2014 to 2020, excluding infants with birth defects. Cases included all infants who died with IC treatment. We matched each case by GA and birth weight to an infant who survived (control). Data for cases were collected for the period of IC treatment, and data for controls were collected for the same timeframe as their matched case. Collected data included the number of invasive procedures, major surgeries, and the use of medications for pain. Invasive procedures consisted of heel-stick and placement of peripheral arterial line, peripherally inserted central catheter, and peripheral intravenous line. We also collected information about positive NICU experiences, such as enteral feedings and being held by the family.
Results: There were 20 cases matched to 20 controls. Infant and family demographics were similar (Table 1). The median (range) of IC for cases was 8(0-93) days. The mean (SD) number of invasive procedures was higher for the cases than the controls, 34 (30) vs. 24 (22), p=0.004 (Figure 1). Additionally, cases underwent 8 major surgeries compared to 4 in the controls. Major surgeries included laparotomy, thoracotomy, peritoneal drain, and ventricular reservoir. Cases spent more NICU time than controls needing pain medications (64% vs. 27%, p< 0.001) and without being fed (54% vs. 39%, p< 0.001). Half of the cases were never held by parents until the day they died.Conclusion(s): Our results suggest EPI at the edge of viability who die despite IC face a higher treatment burden than those who survive. More studies evaluating the experience of EPI who die with IC are needed to ensure that parents and clinicians have the necessary information to make informed treatment choices.
Figure 1A and 1B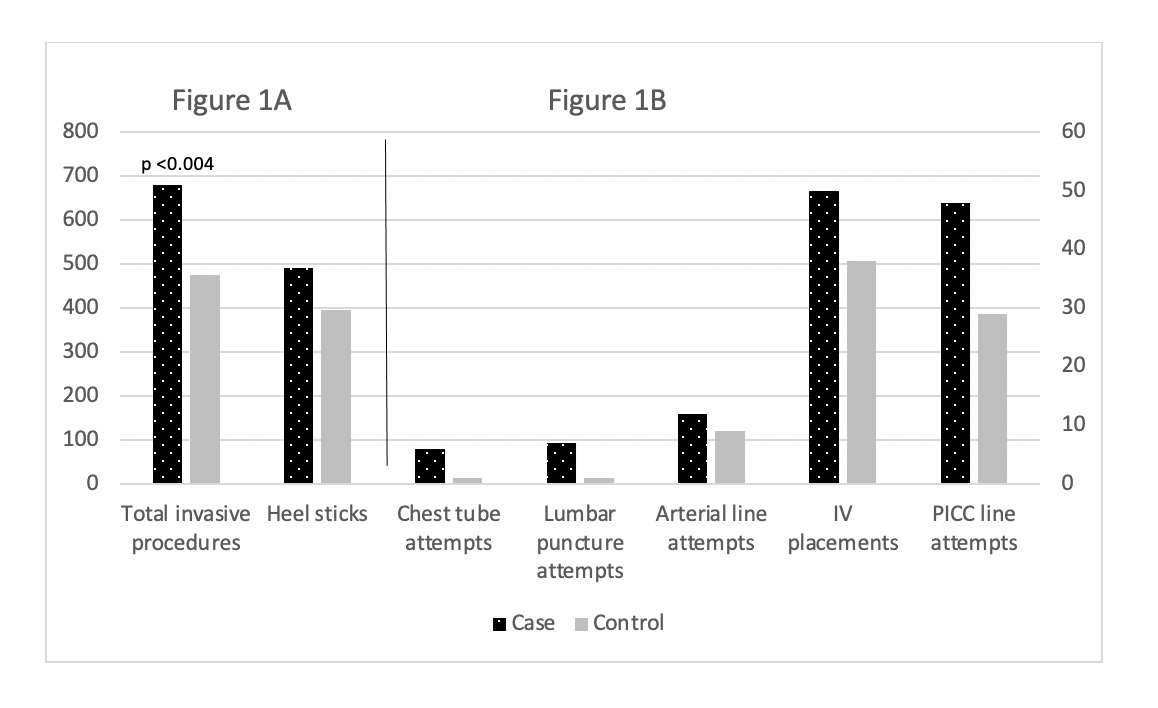 Frequencies of invasive procedures performed on 22-25 weeks GA infants who died (cases) and infants who survived (controls). Infants who died underwent more invasive procedures, p=0.004. Figures were separated to maintain scale
Frequencies of invasive procedures performed on 22-25 weeks GA infants who died (cases) and infants who survived (controls). Infants who died underwent more invasive procedures, p=0.004. Figures were separated to maintain scale
Table 1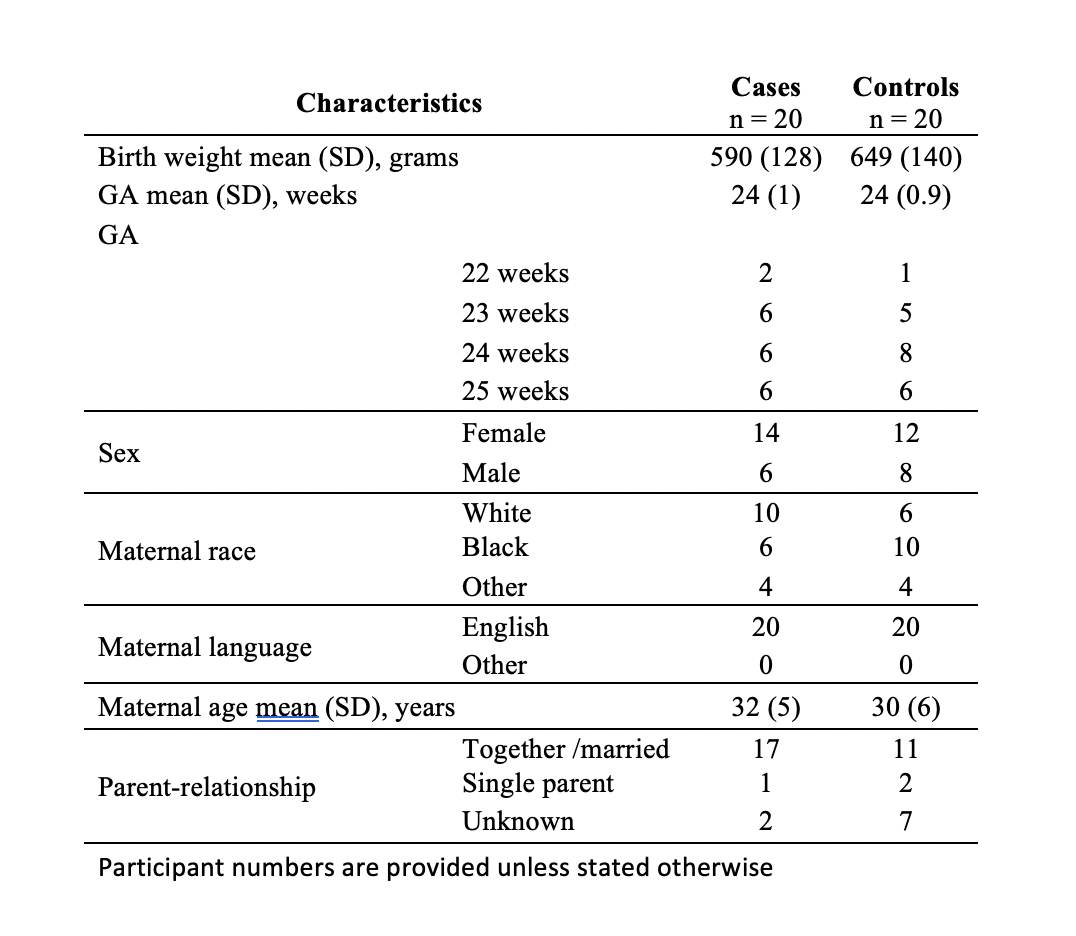 Demographic Information
Demographic Information
Objective: Determine if EPI who die with IC face more treatment-associated negative experiences over the same time frame than EPI who survive.
Design/Methods: We designed a 1:1 case-control study and screened medical records of all inborn 22 to 25 weeks gestational age (GA) infants admitted to the neonatal intensive care unit (NICU) from 2014 to 2020, excluding infants with birth defects. Cases included all infants who died with IC treatment. We matched each case by GA and birth weight to an infant who survived (control). Data for cases were collected for the period of IC treatment, and data for controls were collected for the same timeframe as their matched case. Collected data included the number of invasive procedures, major surgeries, and the use of medications for pain. Invasive procedures consisted of heel-stick and placement of peripheral arterial line, peripherally inserted central catheter, and peripheral intravenous line. We also collected information about positive NICU experiences, such as enteral feedings and being held by the family.
Results: There were 20 cases matched to 20 controls. Infant and family demographics were similar (Table 1). The median (range) of IC for cases was 8(0-93) days. The mean (SD) number of invasive procedures was higher for the cases than the controls, 34 (30) vs. 24 (22), p=0.004 (Figure 1). Additionally, cases underwent 8 major surgeries compared to 4 in the controls. Major surgeries included laparotomy, thoracotomy, peritoneal drain, and ventricular reservoir. Cases spent more NICU time than controls needing pain medications (64% vs. 27%, p< 0.001) and without being fed (54% vs. 39%, p< 0.001). Half of the cases were never held by parents until the day they died.Conclusion(s): Our results suggest EPI at the edge of viability who die despite IC face a higher treatment burden than those who survive. More studies evaluating the experience of EPI who die with IC are needed to ensure that parents and clinicians have the necessary information to make informed treatment choices.
Figure 1A and 1B
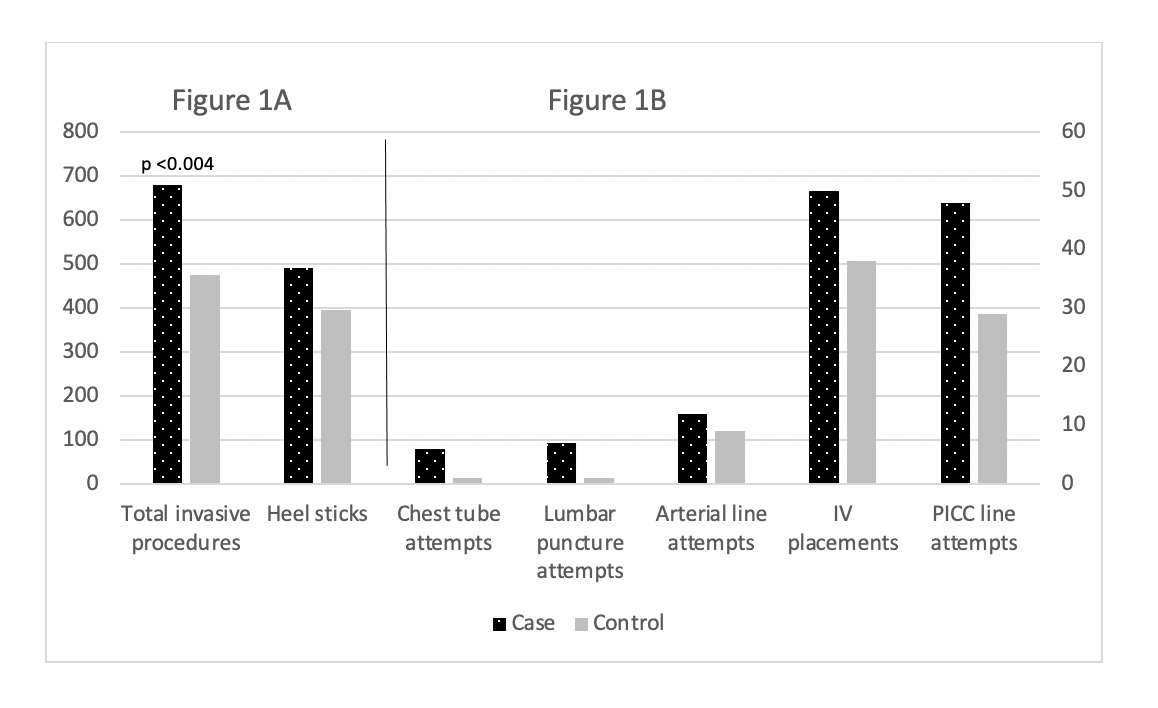 Frequencies of invasive procedures performed on 22-25 weeks GA infants who died (cases) and infants who survived (controls). Infants who died underwent more invasive procedures, p=0.004. Figures were separated to maintain scale
Frequencies of invasive procedures performed on 22-25 weeks GA infants who died (cases) and infants who survived (controls). Infants who died underwent more invasive procedures, p=0.004. Figures were separated to maintain scaleTable 1
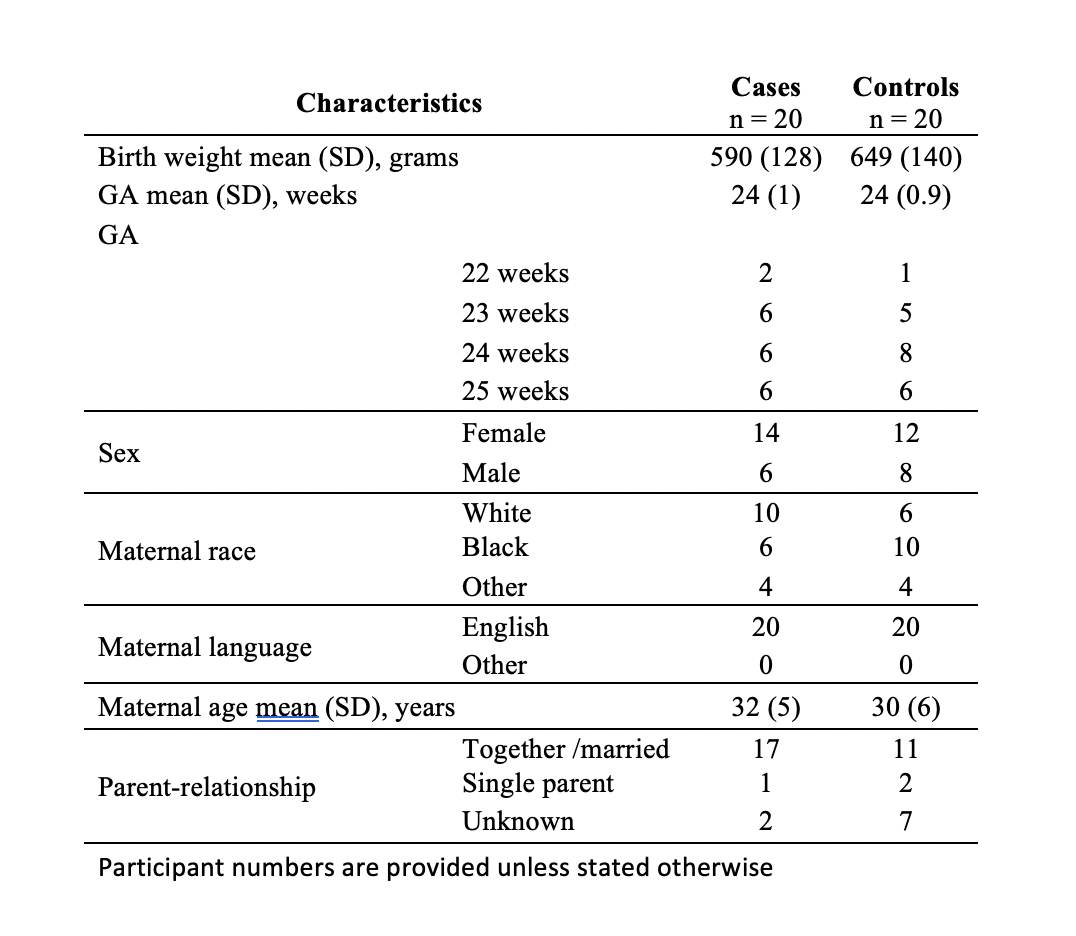 Demographic Information
Demographic Information