Neonatal Fetal Nutrition & Metabolism
Category: Abstract Submission
Neonatal Fetal Nutrition & Metabolism I
276 - Impact of Maternal Diabetes on Neonatal Body Composition, Energy Homeostasis and Hypothalamic Salivary Gene Expression
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 276
Publication Number: 276.119
Publication Number: 276.119
Dara Azuma, Tufts Medical Center, Boston, MA, United States; Yvette Penner, Tufts Childrens Hospital, Brighton, MA, United States; Tomoko Kaneko-Tarui, Tufts Medical Center, Boston, MA, United States; Taysir Mahmoud, Tufts Medical Center, Boston, MA, United States; Perrie O'Tierney-Ginn, Tufts University School of Medicine, Boston, MA, United States; Jill Maron, Women & Infants Hospital of Rhode Island, Providence, RI, United States
- DA
Dara Azuma, MD
Neonatologist
Tufts Medical Center
Boston, Massachusetts, United States
Presenting Author(s)
Background: Infants of diabetic mothers (IDMs) may exhibit decreased oral intake, requiring nasogastric feedings and prolonged hospitalization.
Objective: We hypothesize that increased insulin exposure and resulting overgrowth in utero disrupts hypothalamic regulation of food intake, correlates to body composition and impacts feeding in IDMs.
Design/Methods: Infants born at ≥ 35 weeks’ gestation to mothers with gestational or type II diabetes (IDM cohort) and normoglycemic mothers (control cohort) were recruited. Infants born to mothers with Type I DM or preeclampsia and/or with a history of fetal growth restriction, opioid exposure, or major congenital anomalies were excluded. Salivary expression of known hunger signaling genes 5’AMP-activated protein kinase(AMPK), Neuropeptide Y receptor Y2(NPY2R), leptin(LEP), ghrelin(GHRL), proopiomelanocortin(POMC), and adiponectin(ADIPOQ) were quantified using RT-qPCR. Body composition was assessed via skinfold measurements and compared and correlated between cohorts. Feeding outcomes were recorded.
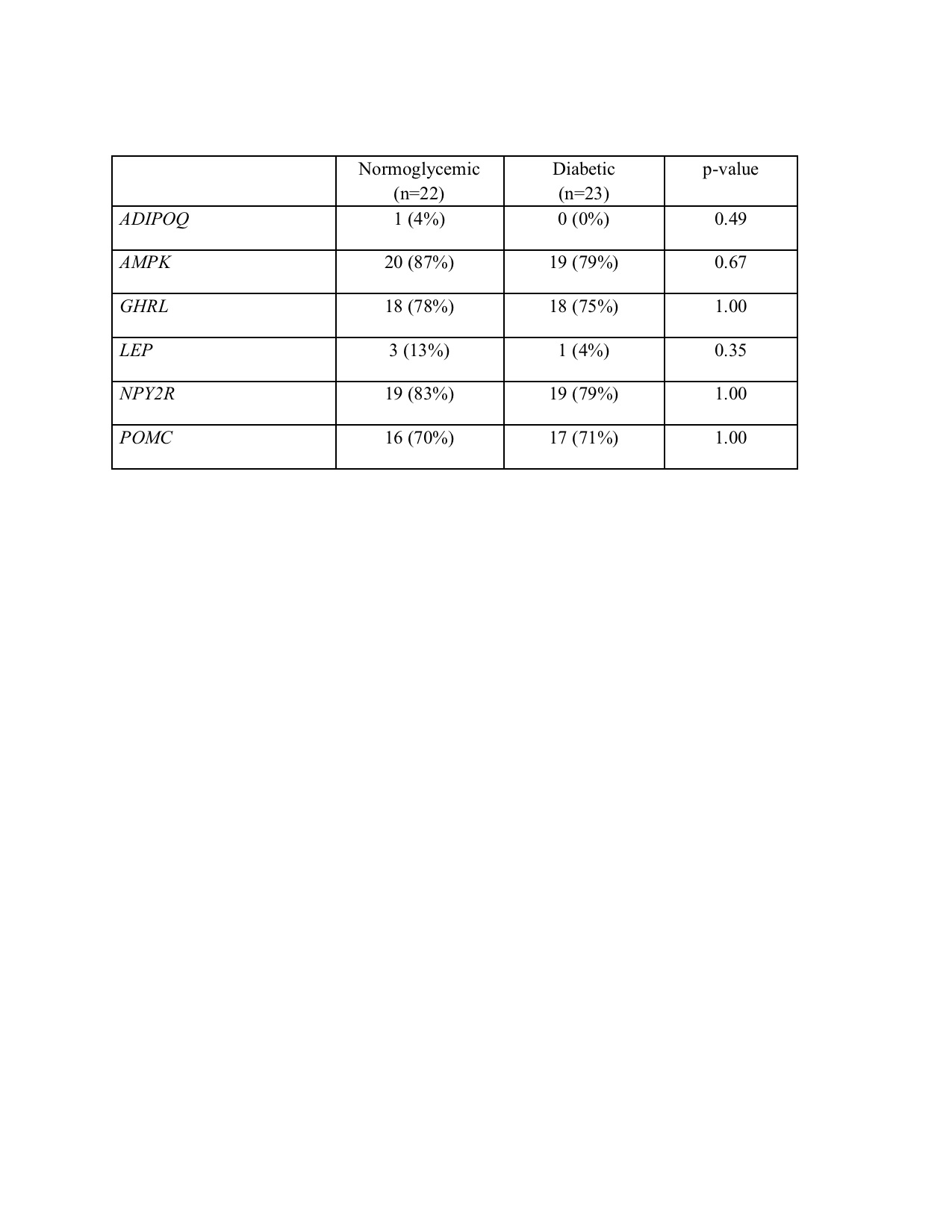
Results: 23 infants were recruited in the IDM cohort and 22 infants in the control cohort. LEP and ADIPOQ were not reliably detected in either cohort. Although statistical significance was not achieved, AMPK, GHRL and NPY2R were less likely to be detected in the IDM cohort, whereas POMC was more likely to be detected in the IDM cohort as compared to the normoglycemia cohort. Infants in the IDM cohort had greater adiposity as compared to infants in the normoglycemia cohort. When adjusting for sex and gestational age at birth, the IDM cohort had lower fat mass than the normoglycemia cohort but a greater percentage of fat mass. Three infants in the study had poor feeding noted in their medical record. These infants were IDMs born at lower gestational ages but had higher birth weights, birth weight percentiles, fat mass and percentile of fat mass, as compared to all infants who fed. GHRL, NPY2R, and POMC were expressed in all three non-feeders but AMPK was less frequently expressed in non-feeders as compared to orally feeding infants, independent of cohort.Conclusion(s): Non-invasive assessment of hunger signaling gene expression is possible through salivary analysis of AMPK, POMC, NPY2R, and GHRL. Although our numbers were limited, IDMs with poor feeding had greater fat mass and salivary expression profiles consistent with appetite suppression. Future studies should target IDMs requiring feeding support to understand mechanisms driving aberrant feeding behavior.
Figure 1. Proposed Mechanism of Altered Feeding Due to In utero Insulin Exposure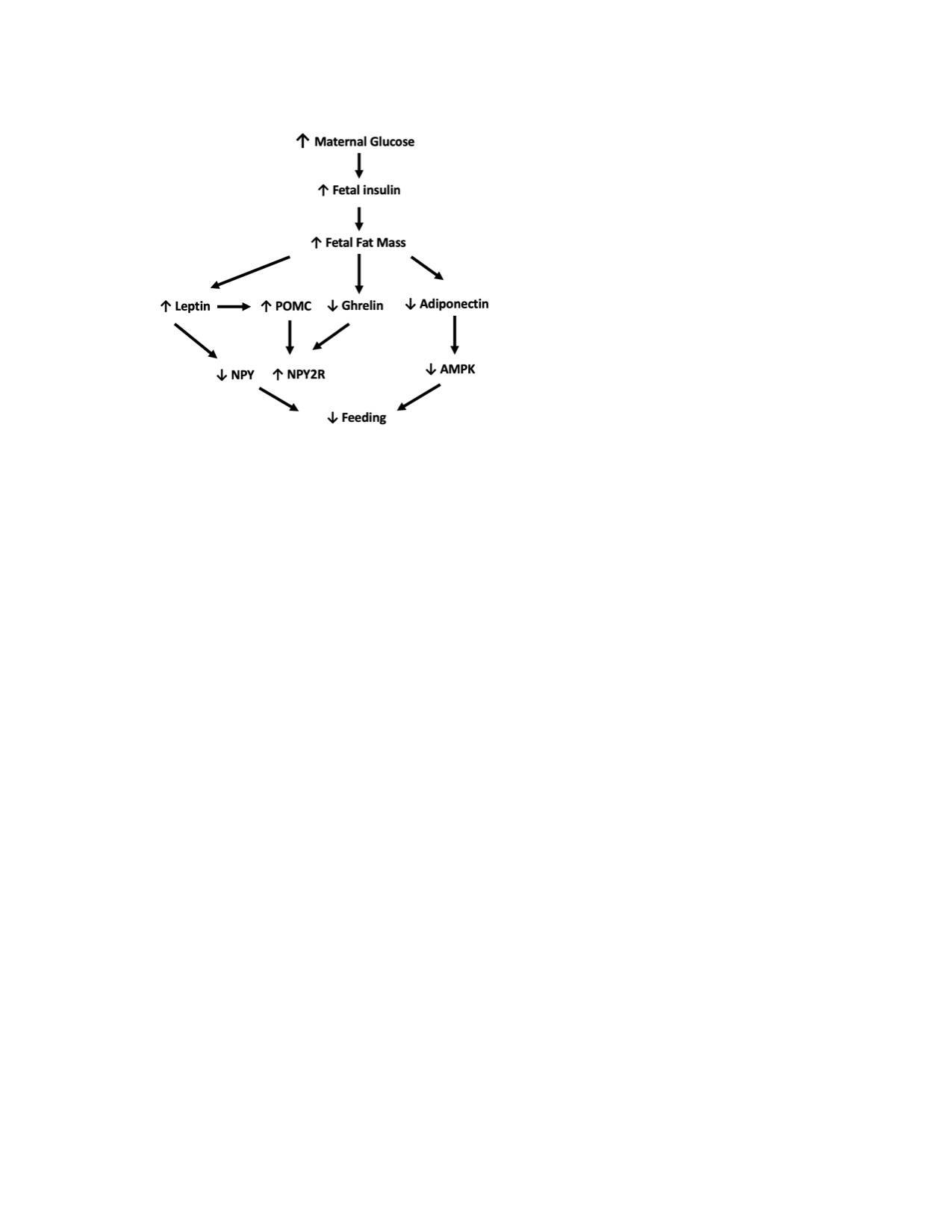 ↓:decrease, ↑:increase, POMC: proopiomelanocortin, AMPK: 5’AMP-activated protein kinase, NPY:Neuropeptide Y NPY2R; Neuropeptide Y 2 receptor
↓:decrease, ↑:increase, POMC: proopiomelanocortin, AMPK: 5’AMP-activated protein kinase, NPY:Neuropeptide Y NPY2R; Neuropeptide Y 2 receptor
Table 1. Gene Expression by Cohort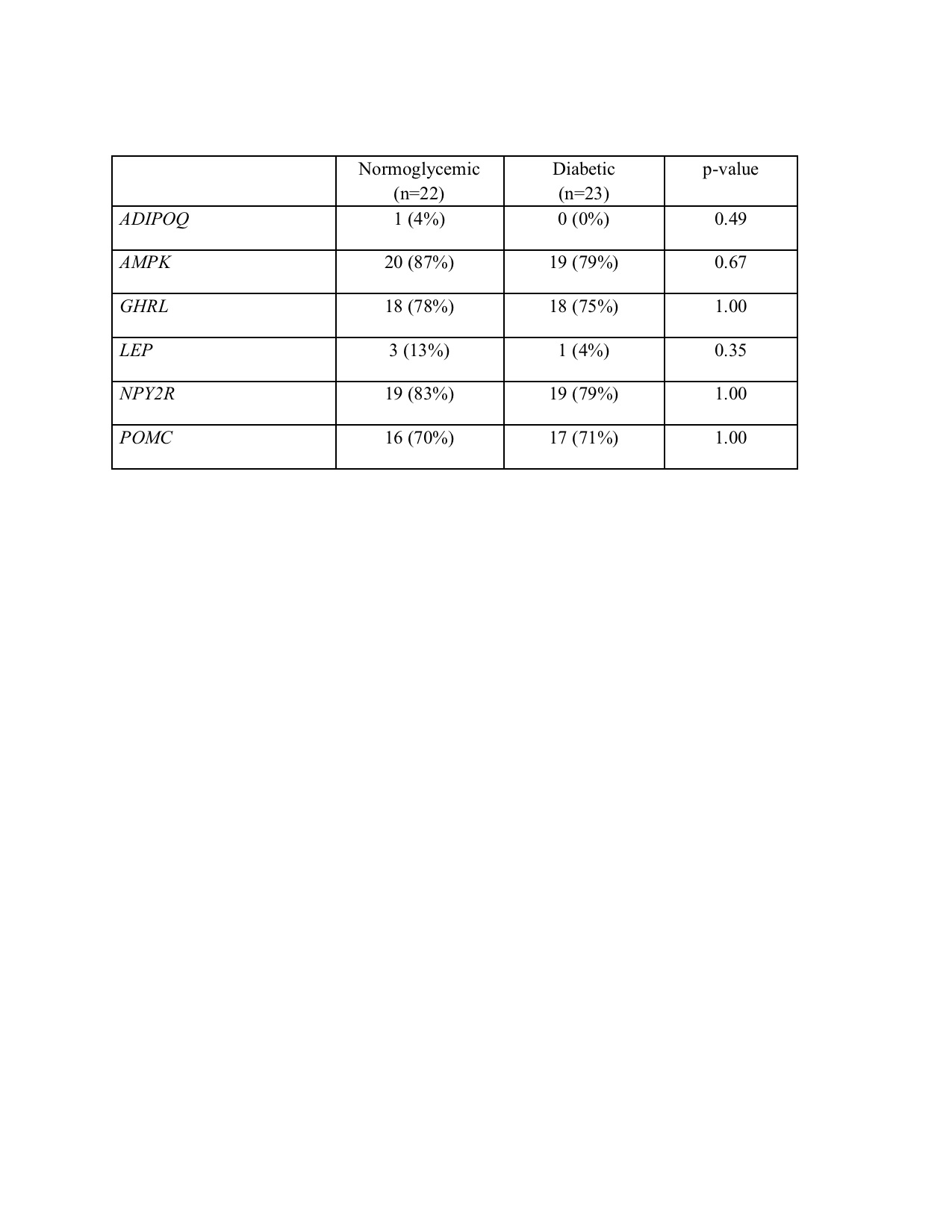
Objective: We hypothesize that increased insulin exposure and resulting overgrowth in utero disrupts hypothalamic regulation of food intake, correlates to body composition and impacts feeding in IDMs.
Design/Methods: Infants born at ≥ 35 weeks’ gestation to mothers with gestational or type II diabetes (IDM cohort) and normoglycemic mothers (control cohort) were recruited. Infants born to mothers with Type I DM or preeclampsia and/or with a history of fetal growth restriction, opioid exposure, or major congenital anomalies were excluded. Salivary expression of known hunger signaling genes 5’AMP-activated protein kinase(AMPK), Neuropeptide Y receptor Y2(NPY2R), leptin(LEP), ghrelin(GHRL), proopiomelanocortin(POMC), and adiponectin(ADIPOQ) were quantified using RT-qPCR. Body composition was assessed via skinfold measurements and compared and correlated between cohorts. Feeding outcomes were recorded.
Results: 23 infants were recruited in the IDM cohort and 22 infants in the control cohort. LEP and ADIPOQ were not reliably detected in either cohort. Although statistical significance was not achieved, AMPK, GHRL and NPY2R were less likely to be detected in the IDM cohort, whereas POMC was more likely to be detected in the IDM cohort as compared to the normoglycemia cohort. Infants in the IDM cohort had greater adiposity as compared to infants in the normoglycemia cohort. When adjusting for sex and gestational age at birth, the IDM cohort had lower fat mass than the normoglycemia cohort but a greater percentage of fat mass. Three infants in the study had poor feeding noted in their medical record. These infants were IDMs born at lower gestational ages but had higher birth weights, birth weight percentiles, fat mass and percentile of fat mass, as compared to all infants who fed. GHRL, NPY2R, and POMC were expressed in all three non-feeders but AMPK was less frequently expressed in non-feeders as compared to orally feeding infants, independent of cohort.Conclusion(s): Non-invasive assessment of hunger signaling gene expression is possible through salivary analysis of AMPK, POMC, NPY2R, and GHRL. Although our numbers were limited, IDMs with poor feeding had greater fat mass and salivary expression profiles consistent with appetite suppression. Future studies should target IDMs requiring feeding support to understand mechanisms driving aberrant feeding behavior.
Figure 1. Proposed Mechanism of Altered Feeding Due to In utero Insulin Exposure
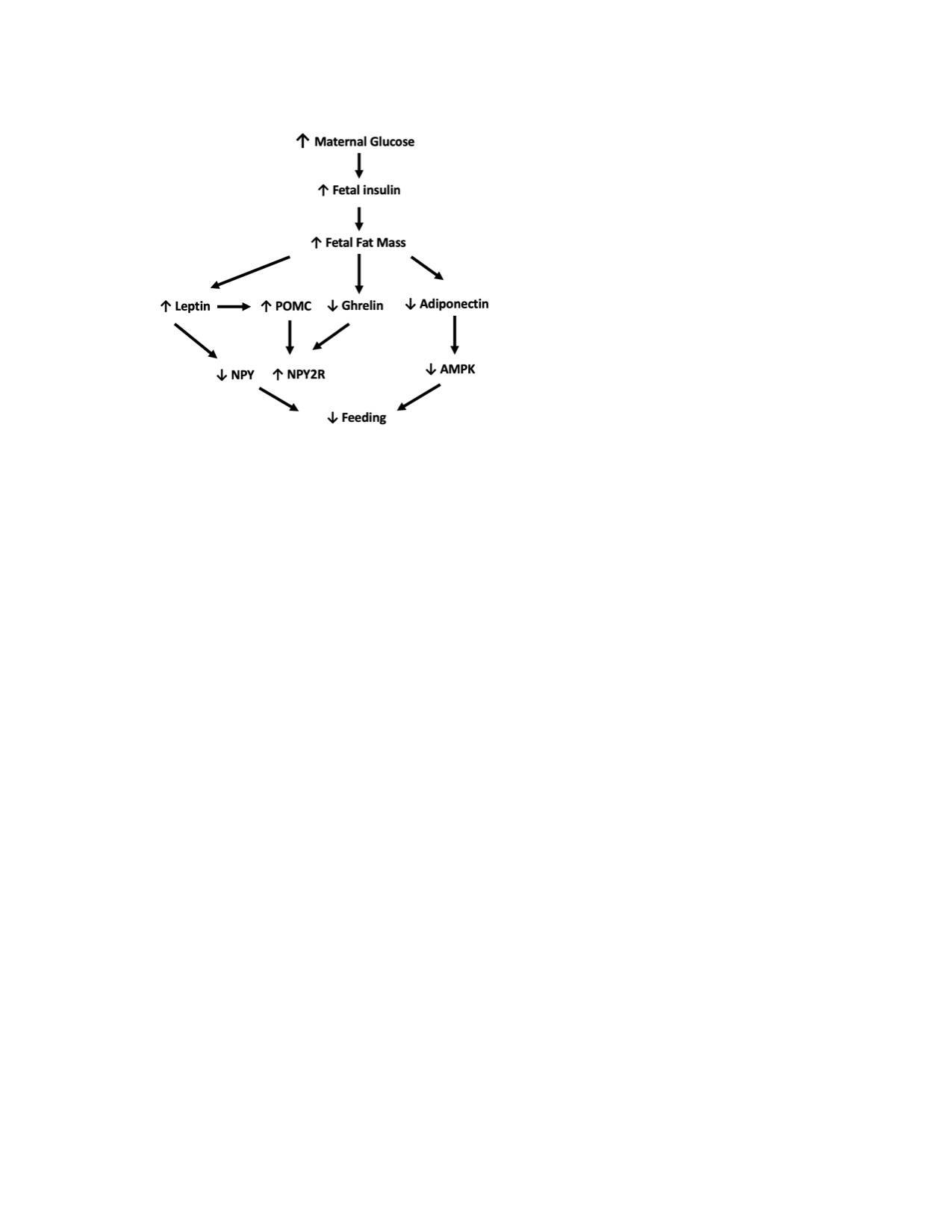 ↓:decrease, ↑:increase, POMC: proopiomelanocortin, AMPK: 5’AMP-activated protein kinase, NPY:Neuropeptide Y NPY2R; Neuropeptide Y 2 receptor
↓:decrease, ↑:increase, POMC: proopiomelanocortin, AMPK: 5’AMP-activated protein kinase, NPY:Neuropeptide Y NPY2R; Neuropeptide Y 2 receptorTable 1. Gene Expression by Cohort