Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine IV
80 - Impact of Pediatric Emergency Department Zoning During the COVID-19 Pandemic
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 80
Publication Number: 80.106
Publication Number: 80.106
Zachary K. Manier, Nicklaus Children’s Hospital, Miami, FL, United States; Barbara Pena, Nicklaus Children’s Hospital, Miami, FL, United States; David Lowe, Nicklaus Children’s Hospital, Miami, FL, United States; Juan Lozano, Florida International University Herbert Wertheim College of Medicine, Miami, FL, United States

Zachary K. Manier, MD
Pediatric Emergency Medicine Fellow
Nicklaus Children’s Hospital
Miami, Florida, United States
Presenting Author(s)
Background: The WHO declared COVID-19 a global pandemic in March 2020, and hospitals across the globe quickly acted to implement appropriate protocols. Our pediatric emergency department was separated into zones to more easily identify those with increased likelihood of having COVID-19. This was accomplished in triage based on screening questions and specific predetermined symptoms.
Objective: The primary objective is to assess the efficacy of zoning in the pediatric emergency department (PED) during the COVID-19 pandemic, determining if splitting the PED into “clean” and “dirty” zones effectively identifies those patients more likely to have COVID-19.
Design/Methods: Single institution retrospective cohort study of pediatric patients ages 0-21 years who presented to the ED between April 2020 and October 2020. Data was extracted from the hospital electronic data warehouse. COVID-19 test results, zone location, and other demographics were documented for all patients in each zone. Baseline characteristics were described, and bivariate analyses were conducted to compare the distribution of the baseline features according to the ED zone to which patients were assigned. Finally, multivariate logistic regression was used to assess the association between the COVID-19 zone and test result while controlling for potential confounders.
Results: A total of 24,237 patients were included in the study, and 7853 (32.3%) had a COVID-19 test completed. Of them, 1777 were positive, 6044 negative and 14 were pending/unknown. Patients in the COVID-19 zone were 2.5 times more likely to have a positive result than those in the non-COVID-19 zone (RR 2.5, 95% CI 2.2 to 2.8, p value < 0.0001). The association between the COVID-19 zone and a positive test result remained significant after adjusting for confounders (aOR 2.2, 95% CI 1.9 to 2.5, p-value < 0.0001), which included age, insurance status, ESI level, month of arrival, and other lab work ordered.Conclusion(s): There was a significant difference in the frequency of positive COVID-19 tests
between patients in the COVID-19 and non-COVID-19 zones. Splitting the PED into zones based on pre-screening questions and appropriate symptoms effectively separated those patients more likely to have COVID-19. When resources, such as personal protective equipment, are scarce, this allows PED personnel to utilize these resources more effectively, while maximizing both patient and provider safety through zoning separation.
Table 2B.png) Baseline characteristics of patients in the COVID and non-COVID zones according to COVID test results and other characteristics
Baseline characteristics of patients in the COVID and non-COVID zones according to COVID test results and other characteristics
Table 4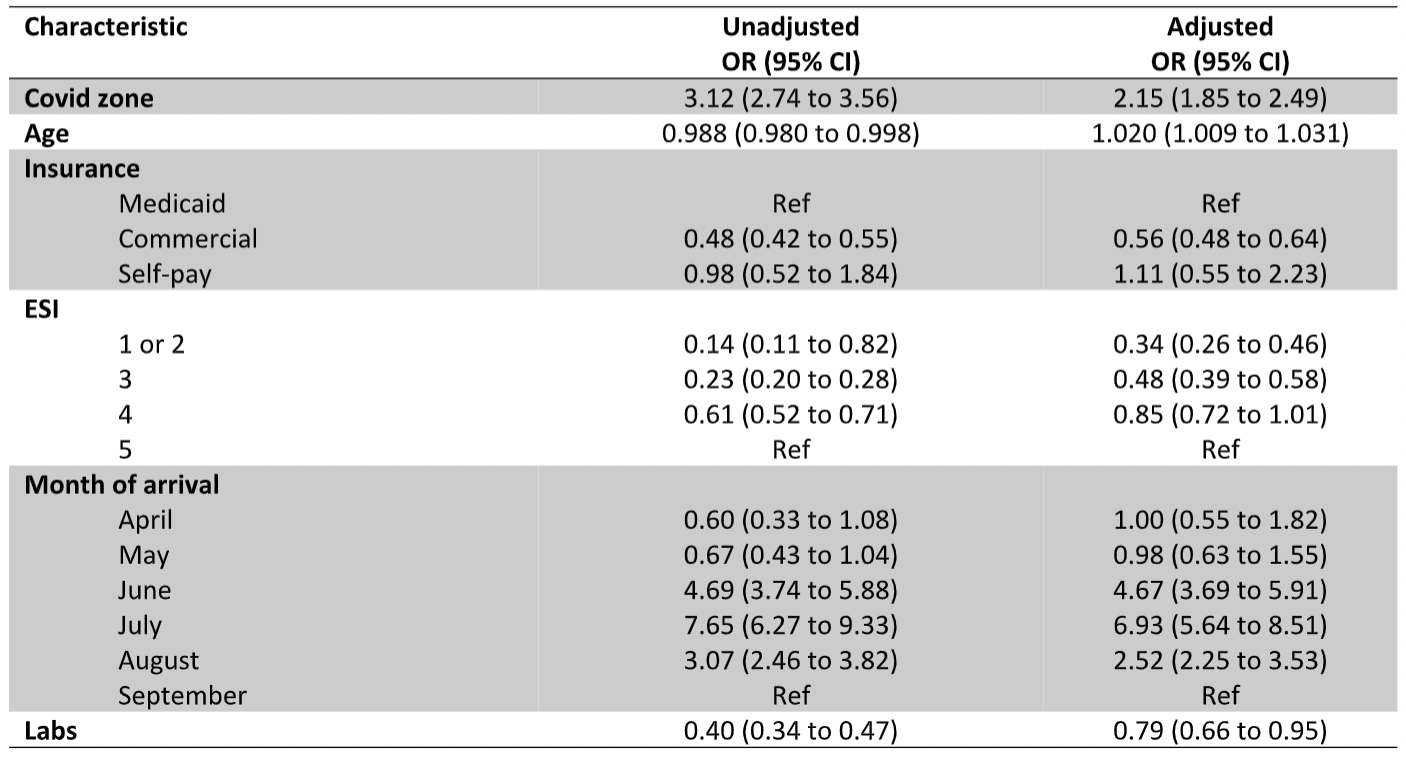 Unadjusted and adjusted associations between the COVID zone/confounders included in the model and COVID test results
Unadjusted and adjusted associations between the COVID zone/confounders included in the model and COVID test results
Objective: The primary objective is to assess the efficacy of zoning in the pediatric emergency department (PED) during the COVID-19 pandemic, determining if splitting the PED into “clean” and “dirty” zones effectively identifies those patients more likely to have COVID-19.
Design/Methods: Single institution retrospective cohort study of pediatric patients ages 0-21 years who presented to the ED between April 2020 and October 2020. Data was extracted from the hospital electronic data warehouse. COVID-19 test results, zone location, and other demographics were documented for all patients in each zone. Baseline characteristics were described, and bivariate analyses were conducted to compare the distribution of the baseline features according to the ED zone to which patients were assigned. Finally, multivariate logistic regression was used to assess the association between the COVID-19 zone and test result while controlling for potential confounders.
Results: A total of 24,237 patients were included in the study, and 7853 (32.3%) had a COVID-19 test completed. Of them, 1777 were positive, 6044 negative and 14 were pending/unknown. Patients in the COVID-19 zone were 2.5 times more likely to have a positive result than those in the non-COVID-19 zone (RR 2.5, 95% CI 2.2 to 2.8, p value < 0.0001). The association between the COVID-19 zone and a positive test result remained significant after adjusting for confounders (aOR 2.2, 95% CI 1.9 to 2.5, p-value < 0.0001), which included age, insurance status, ESI level, month of arrival, and other lab work ordered.Conclusion(s): There was a significant difference in the frequency of positive COVID-19 tests
between patients in the COVID-19 and non-COVID-19 zones. Splitting the PED into zones based on pre-screening questions and appropriate symptoms effectively separated those patients more likely to have COVID-19. When resources, such as personal protective equipment, are scarce, this allows PED personnel to utilize these resources more effectively, while maximizing both patient and provider safety through zoning separation.
Table 2B
.png) Baseline characteristics of patients in the COVID and non-COVID zones according to COVID test results and other characteristics
Baseline characteristics of patients in the COVID and non-COVID zones according to COVID test results and other characteristicsTable 4
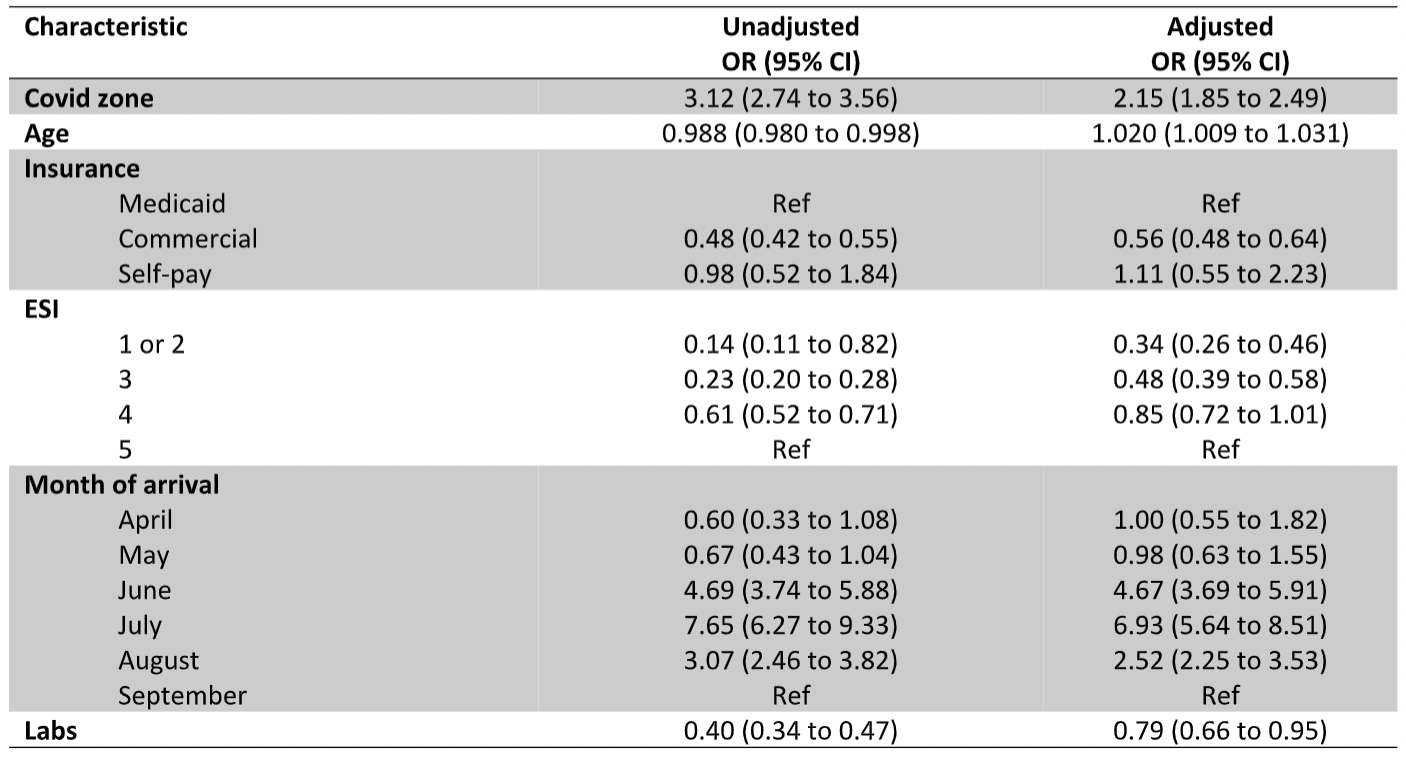 Unadjusted and adjusted associations between the COVID zone/confounders included in the model and COVID test results
Unadjusted and adjusted associations between the COVID zone/confounders included in the model and COVID test results