Health Equity/Social Determinants of Health
Category: Abstract Submission
Health Equity/Social Determinants of Health IV
162 - Social Needs Screening During Pediatric Emergency Department Visits: Disparities in Unmet Social Needs by Language
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 162
Publication Number: 162.411
Publication Number: 162.411
Natalie J. Tedford, University of Utah/Primary Children's Hospital, Salt Lake City, UT, United States; Elizabeth M. Keating, University of Utah, Salt Lake City, UT, United States; Zhining Ou, University of Utah - Salt Lake City, UT, Salt Lake City, UT, United States; Maija Holsti, University of Utah School of Medicine, SALT LAKE CITY, UT, United States; Andrea S. Wallace, University of Utah College of Nursing, Salt Lake City, UT, United States; Jeff Robison, University of Utah School of Medicine, Salt Lake City, UT, United States
- EK
Elizabeth M. Keating, MD, MSPH (she/her/hers)
Assistant Professor
University of Utah
Salt Lake City, Utah, United States
Presenting Author(s)
Background: A pediatric emergency department (PED) serves as part of the social safety net for families who lack consistent primary care access and have limited English proficiency (LEP). PED visits are an opportunity to identify children with unmet social needs (USN) and connect families to community resources. The prevalence of USN and disparities by language preference in the PED are insufficiently described to guide screening processes.
Objective: To define the prevalence of USN in the patient population of a PED and examine disparities in USN by self-selected language and patient demographics.
Design/Methods: We conducted this cross-sectional, descriptive study at a free-standing children’s hospital and level 1 trauma center. Research assistants approached a convenience sample of English- and Spanish-speaking caregivers of patients < 18 years of age. Each enrolled caregiver was offered a pediatric version of the validated Screener for Intensifying Community Referrals for Health (p-SINCERE) and given United Way 211 resource cards. In the caregiver’s self-selected language, the survey assessed patient demographics and 10 social needs. The primary outcome was prevalence of USN. We summarized and compared variables between self-selected language using descriptive statistics. We used multivariable logistic regression (LR) to assess the association between self-selected language and presence of USN.
Results: Of the 10156 patients who presented to the PED during the study hours of 6am to midnight from 4/1/2021 to 8/3/2021, there were 9922 (97.7%) eligible, 5357 (52.7%) approached, and 3987 (39.3%) enrolled caregivers (see Figure 1). Of the 3987 caregivers enrolled, selected language was English for 3662 (91.8%) and Spanish for 325 (8.2%). Enrolled patients were mostly male (52%), non-Hispanic (71%), White/Caucasian (68%), had private health insurance (55%), had an English-speaking caregiver (92%), and had no USN (55%). There were 1680 (42%) enrolled caregivers with presence of USN, representing 39.7% of English-speaking caregivers and 70.2% of Spanish-speaking caregivers (p < 0.001). Patient characteristics are stratified in Table 1 by language selection. The odds of having USN present was higher in Spanish-speakers (OR = 2.06, 95% CI: 1.27-3.36, p-value = 0.004) than in English-speakers (see Table 2 for LR results).Conclusion(s): This single-center analysis of social needs screening during PED visits found higher USN in Spanish-speaking caregivers. The large percentage of patients with USN and higher odds of USN in Spanish-speaking caregivers highlights the importance for social needs screening during PED visits.
Curriculum Vitae - Natalie J Tedford, MDCV_Fellowship_NJT.pdf
Table 1: Patient Characteristics and Needs Stratified by Caregiver’s Self-Selected Language of Survey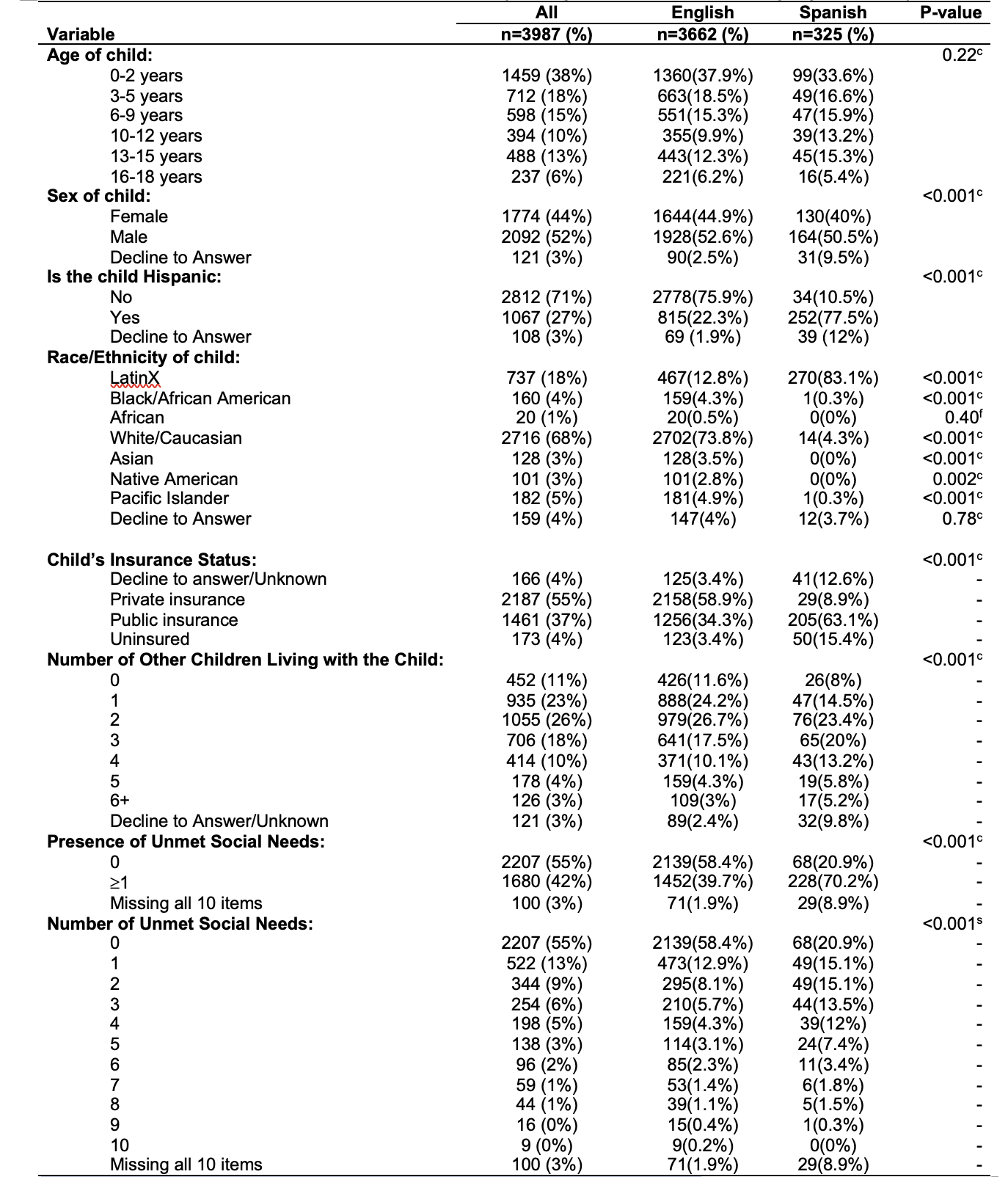 c Chi-squared test, f Fisher's exact test, s Chi-squared test by Montecarlo simulation.
c Chi-squared test, f Fisher's exact test, s Chi-squared test by Montecarlo simulation.
Objective: To define the prevalence of USN in the patient population of a PED and examine disparities in USN by self-selected language and patient demographics.
Design/Methods: We conducted this cross-sectional, descriptive study at a free-standing children’s hospital and level 1 trauma center. Research assistants approached a convenience sample of English- and Spanish-speaking caregivers of patients < 18 years of age. Each enrolled caregiver was offered a pediatric version of the validated Screener for Intensifying Community Referrals for Health (p-SINCERE) and given United Way 211 resource cards. In the caregiver’s self-selected language, the survey assessed patient demographics and 10 social needs. The primary outcome was prevalence of USN. We summarized and compared variables between self-selected language using descriptive statistics. We used multivariable logistic regression (LR) to assess the association between self-selected language and presence of USN.
Results: Of the 10156 patients who presented to the PED during the study hours of 6am to midnight from 4/1/2021 to 8/3/2021, there were 9922 (97.7%) eligible, 5357 (52.7%) approached, and 3987 (39.3%) enrolled caregivers (see Figure 1). Of the 3987 caregivers enrolled, selected language was English for 3662 (91.8%) and Spanish for 325 (8.2%). Enrolled patients were mostly male (52%), non-Hispanic (71%), White/Caucasian (68%), had private health insurance (55%), had an English-speaking caregiver (92%), and had no USN (55%). There were 1680 (42%) enrolled caregivers with presence of USN, representing 39.7% of English-speaking caregivers and 70.2% of Spanish-speaking caregivers (p < 0.001). Patient characteristics are stratified in Table 1 by language selection. The odds of having USN present was higher in Spanish-speakers (OR = 2.06, 95% CI: 1.27-3.36, p-value = 0.004) than in English-speakers (see Table 2 for LR results).Conclusion(s): This single-center analysis of social needs screening during PED visits found higher USN in Spanish-speaking caregivers. The large percentage of patients with USN and higher odds of USN in Spanish-speaking caregivers highlights the importance for social needs screening during PED visits.
Curriculum Vitae - Natalie J Tedford, MDCV_Fellowship_NJT.pdf
Table 1: Patient Characteristics and Needs Stratified by Caregiver’s Self-Selected Language of Survey
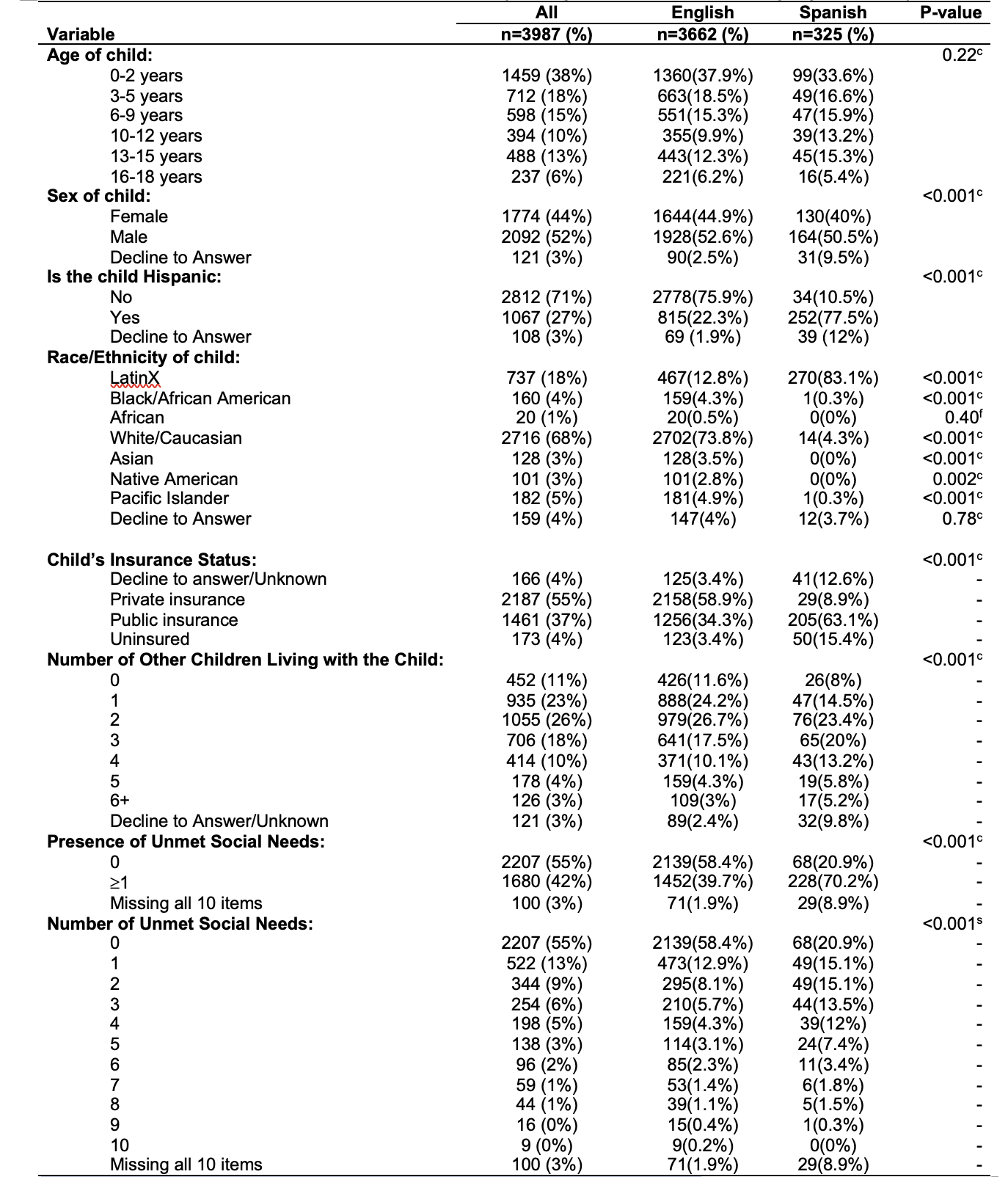 c Chi-squared test, f Fisher's exact test, s Chi-squared test by Montecarlo simulation.
c Chi-squared test, f Fisher's exact test, s Chi-squared test by Montecarlo simulation.