Neonatal Pulmonology
Category: Abstract Submission
Neonatal Pulmonology V: Preclinical studies and Clinical Care Issues
481 - Studying the Effect of Nutritional Status on Lung Development in Premature Neonates Using UTE MRI
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 481
Publication Number: 481.433
Publication Number: 481.433
Ekaterina Dianova, Cincinnati Children's Hospital Medical Center, Union, KY, United States; Paul Kingma, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Kera M. McNelis, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Jason C. Woods, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States; Nara S. Higano, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States
- ED
Ekaterina Dianova, MD
clinical fellow physician
Cincinnati Children's Hospital Medical Center
Union, KY, United States
Presenting Author(s)
Background: Restricted fetal and neonatal growth is a known risk factor for bronchopulmonary dysplasia (BPD), the leading cause of mortality and morbidity in preterm neonates. There is a poor understanding of how nutritional intake and growth are directly related to lung growth and development in infants with BPD.
Objective: This study aims to identify the effect of neonatal nutritional status on lung growth and development by comparing caloric and protein intake, weight gain, and linear growth to lung volumes, lung mass, and lung density using ultrashort echo time (UTE) MRI.
Design/Methods: In this retrospective study, we included infants born before 32 weeks gestational age (GA) with birth weight (BW) < 1500g and diagnosed with BPD of any severity who underwent UTE MRI. Caloric, protein, and fluid daily intake for the first four weeks of life and weekly growth parameters along with respiratory parameters including lung volume, mass, and lung density, obtained with UTE MRI, were analyzed.
Results: The cohort included 95 neonates with mean GA 26.1 weeks and BW 790 g. Nineteen (20%) infants had mild, 32 (34%) moderate, and 44 (46%) severe BPD. Infants with severe and moderate BPD were born at earlier GA, had lower BW and z-scores for weight, length, head circumference at birth (p < 0.05), were shorter for PMA at 4 weeks of life, 36 weeks PMA, and term PMA (p < 0.05). Infants with moderate and severe BPD had less caloric and protein intake than infants with mild BPD (96 and 98 vs 106 kcal/kg/d; 3.79 and 3.75 vs 3.99 g/kg/d; p < 0.05). No significant difference in fluid intake was identified. UTE MRI showed that lung volume and lung mass (normalized by body surface area) increased with increasing BPD severity (443, 534, 738 ml/m2 and 237, 311, 384 g/m2 for mild, moderate, and severe, respectively, p < 0.05). There was a significant negative correlation of total lung mass per BSA with caloric intake during the first four weeks of life (r=-0.23, p < 0.05). The proportion of lung tissue with normal density significantly declined with increasing BPD severity (69% - non-BPD, 65% - mild, 57% - moderate, and 52% - severe BPD; p < 0.05).Conclusion(s): Lower caloric and protein intake during the first four weeks of life is significantly associated with more severe BPD, poor linear growth from birth to term PMA, increased lung volume, and lung mass.
CV Ekaterina Dianova, clinical fellow, MDCV Dianova Fellowship.pdf
Table 2. MRI related patient’s characteristics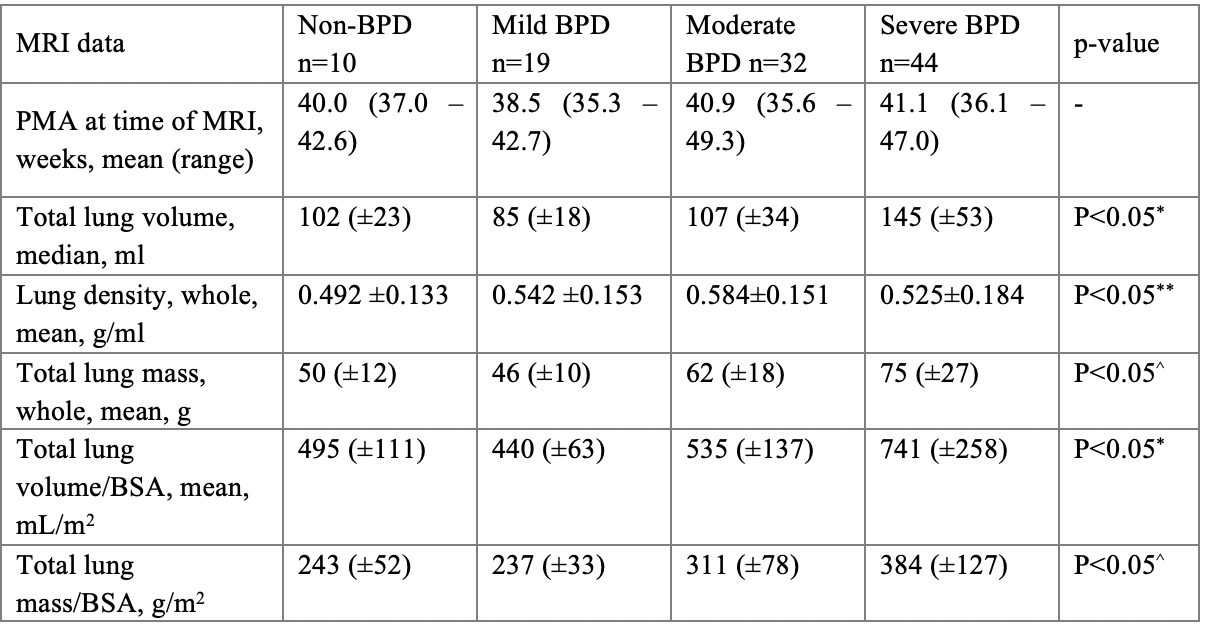 P < 0.05* – one-way ANOVA test was significant; post hoc test was significant between all groups except not significant between control and mild and control and moderate BPD.
P < 0.05* – one-way ANOVA test was significant; post hoc test was significant between all groups except not significant between control and mild and control and moderate BPD.
P < 0.05** - one-way ANOVA test was significant; post hoc test was significant between all groups except not significant between mild and severe, and control and severe BPD.
P < 0.05^ – one-way ANOVA test was significant; post hoc test was significant between all groups except not significant between control and mild BPD.
Objective: This study aims to identify the effect of neonatal nutritional status on lung growth and development by comparing caloric and protein intake, weight gain, and linear growth to lung volumes, lung mass, and lung density using ultrashort echo time (UTE) MRI.
Design/Methods: In this retrospective study, we included infants born before 32 weeks gestational age (GA) with birth weight (BW) < 1500g and diagnosed with BPD of any severity who underwent UTE MRI. Caloric, protein, and fluid daily intake for the first four weeks of life and weekly growth parameters along with respiratory parameters including lung volume, mass, and lung density, obtained with UTE MRI, were analyzed.
Results: The cohort included 95 neonates with mean GA 26.1 weeks and BW 790 g. Nineteen (20%) infants had mild, 32 (34%) moderate, and 44 (46%) severe BPD. Infants with severe and moderate BPD were born at earlier GA, had lower BW and z-scores for weight, length, head circumference at birth (p < 0.05), were shorter for PMA at 4 weeks of life, 36 weeks PMA, and term PMA (p < 0.05). Infants with moderate and severe BPD had less caloric and protein intake than infants with mild BPD (96 and 98 vs 106 kcal/kg/d; 3.79 and 3.75 vs 3.99 g/kg/d; p < 0.05). No significant difference in fluid intake was identified. UTE MRI showed that lung volume and lung mass (normalized by body surface area) increased with increasing BPD severity (443, 534, 738 ml/m2 and 237, 311, 384 g/m2 for mild, moderate, and severe, respectively, p < 0.05). There was a significant negative correlation of total lung mass per BSA with caloric intake during the first four weeks of life (r=-0.23, p < 0.05). The proportion of lung tissue with normal density significantly declined with increasing BPD severity (69% - non-BPD, 65% - mild, 57% - moderate, and 52% - severe BPD; p < 0.05).Conclusion(s): Lower caloric and protein intake during the first four weeks of life is significantly associated with more severe BPD, poor linear growth from birth to term PMA, increased lung volume, and lung mass.
CV Ekaterina Dianova, clinical fellow, MDCV Dianova Fellowship.pdf
Table 2. MRI related patient’s characteristics
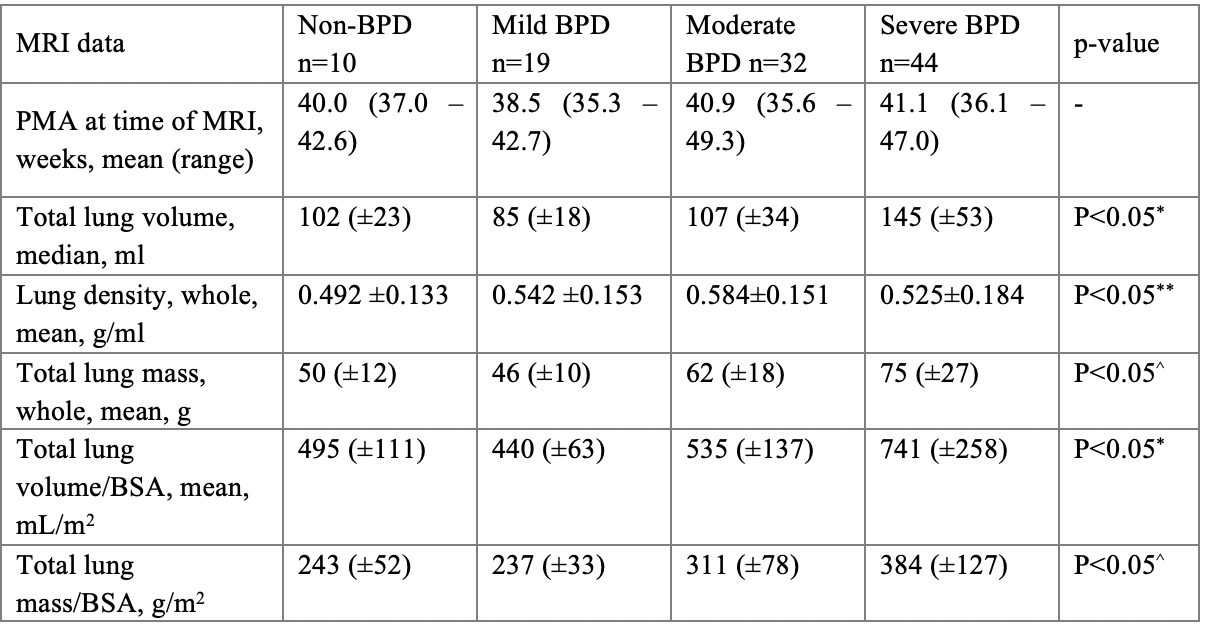 P < 0.05* – one-way ANOVA test was significant; post hoc test was significant between all groups except not significant between control and mild and control and moderate BPD.
P < 0.05* – one-way ANOVA test was significant; post hoc test was significant between all groups except not significant between control and mild and control and moderate BPD.P < 0.05** - one-way ANOVA test was significant; post hoc test was significant between all groups except not significant between mild and severe, and control and severe BPD.
P < 0.05^ – one-way ANOVA test was significant; post hoc test was significant between all groups except not significant between control and mild BPD.
