Neonatal General
Category: Abstract Submission
Neonatology General 10: ID - Inflammation - COVID
328 - The effect of SARS-CoV-2 on the rates of breastfeeding in the newborn nursery
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 328
Publication Number: 328.439
Publication Number: 328.439
John Wang, Keck School of Medicine of the University of Southern California, Los Angeles, CA, United States; Anitha F. Ahmed, Keck School of Medicine of the University of Southern California, Los Angeles, CA, United States; Rangasamy Ramanathan, Keck School of Medicine of USC, Los Angeles, CA, United States; Amy Yeh, Keck School of Medicine of the University of Southern California, Los Angeles, CA, United States
- JW
John Wang, DO/MPH
Resident Physician
University of Southern California/LAC+USC Medical Center
Los Angeles, California, United States
Presenting Author(s)
Background:
Exclusive breastfeeding for the first six months of life is recommended by the American Academy of Pediatrics and the Centers for Disease Control for its benefits to infant immunity, maternal-child bonding, and long-term health. While these benefits are well studied, the SARS-CoV-2 pandemic raises questions about the safety of breastfeeding among SARS-CoV-2-positive mothers. In addition, the pandemic’s effects on hospital staffing, patient-provider facetime, and healthcare access may impact breastfeeding rates.
Objective:
This study aims to explore the effect of the SARS-CoV-2 pandemic on breastfeeding in the newborn nursery at a single center.
Design/Methods:
This is a retrospective cohort study comparing breastfeeding rates between neonates at LAC+USC Medical Center Newborn Nursery from January 2019 to April 2021. We defined the pre-SARS-CoV- 2 group as all neonates born prior to April 2020, and the during-SARS-CoV-2 group as those born from April 2020 to April 2021. Maternal data gathered included gravidity and parity, ethnicity, age, mode of delivery, and pregnancy complications. Infant data gathered included gestational age, birth weight, sex, and hyperbilirubinemia requiring intensive phototherapy. Newborns with maternal contraindications to breastfeeding, such as positive toxicology screen, positive HIV status, incarceration, and placement in foster care were excluded. Rates of exclusive breastfeeding and any breastfeeding were calculated for each month within this time period and compared using T-test. P-value less than 0.05 was considered significant.
Results:
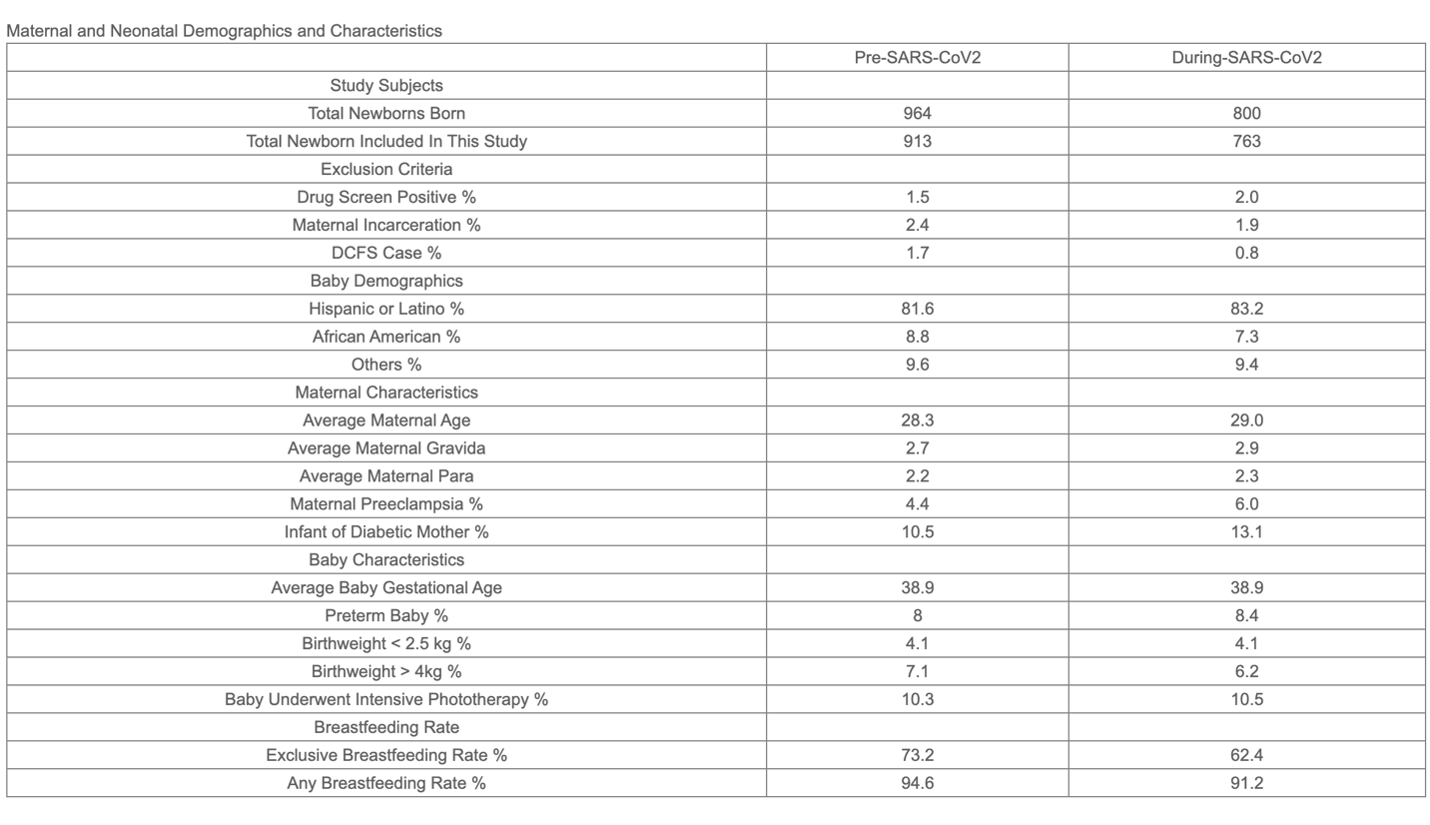
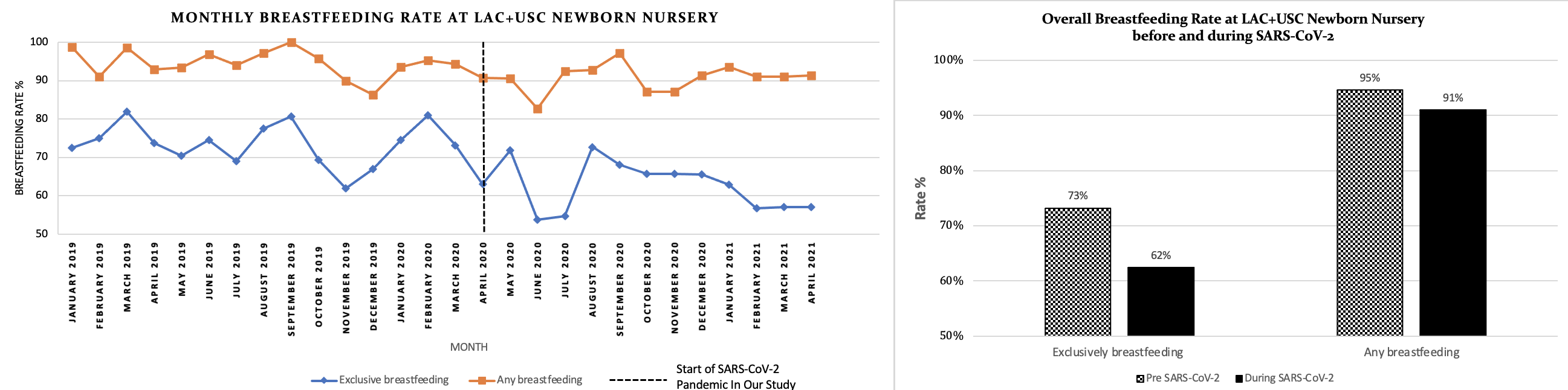
Of the 964 newborns screened in the pre-SARS-CoV-2 cohort, 913 were included. Of the 800 screened during-SARS-CoV-2 cohort, 763 newborns were included. There were no significant differences in the demographics between the two cohorts (Table 1). We found a 11% decrease in the rate of exclusive breastfeeding (p < 0.05) and a 4% decrease in any breastfeeding (p < 0.05) during the SARS-CoV-2 period (Image 1).
Conclusion(s):
The SARS-CoV-2 pandemic had a negative impact on the rates of both exclusive breastfeeding and any breastfeeding among newborns in the normal nursery from a single center in Los Angeles. These results prompted the creation of a specific task force to counter the detrimental effect of the pandemic on breastfeeding. Prospective studies would be useful in assessing the long-term effects of the SARS-CoV-2 pandemic on breastfeeding rates and associated effects on infant immunity, maternal-child bonding, and long- term health.
Table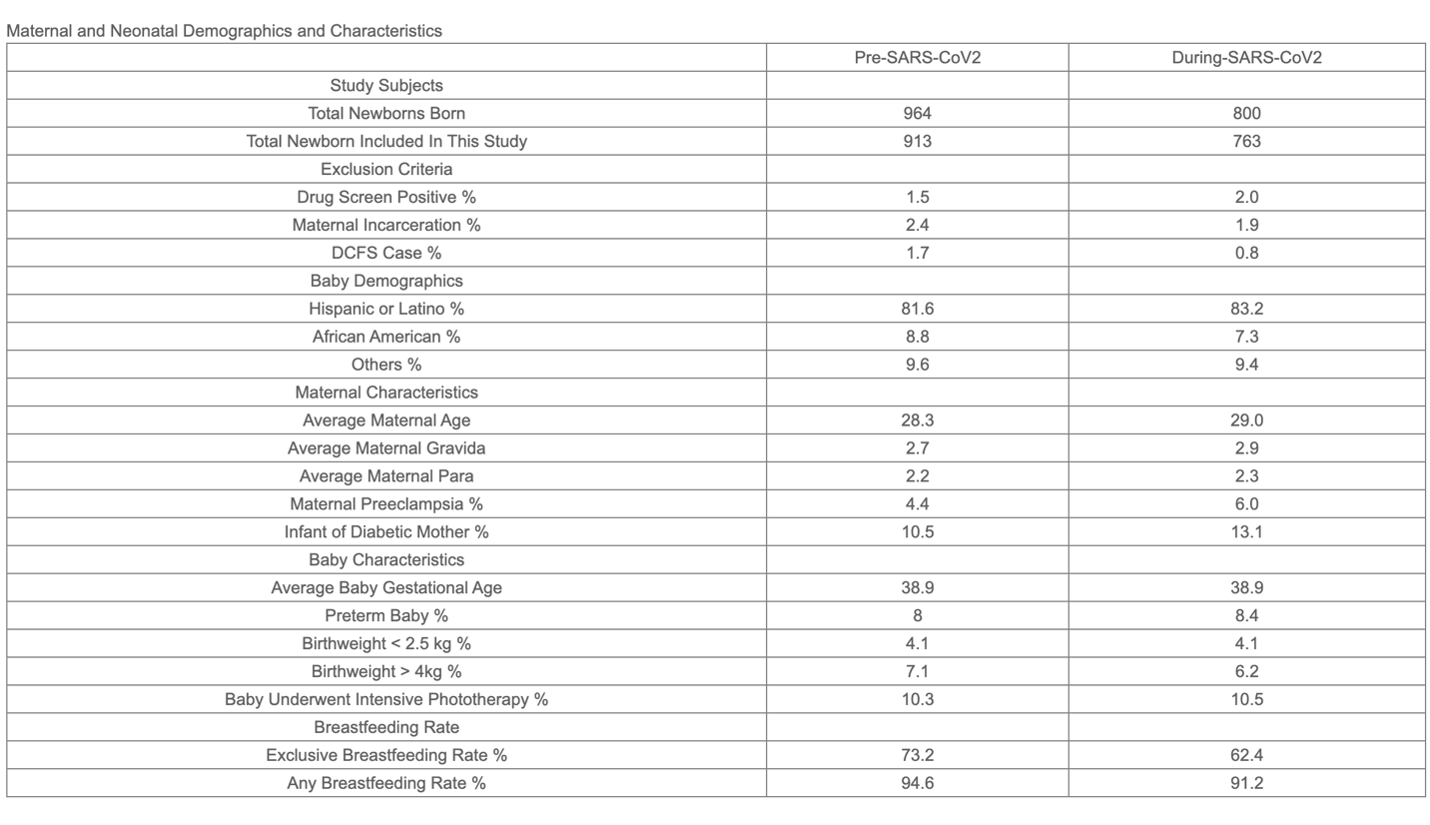 Maternal and Neonatal Demographics and Characteristics
Maternal and Neonatal Demographics and Characteristics
Image 1.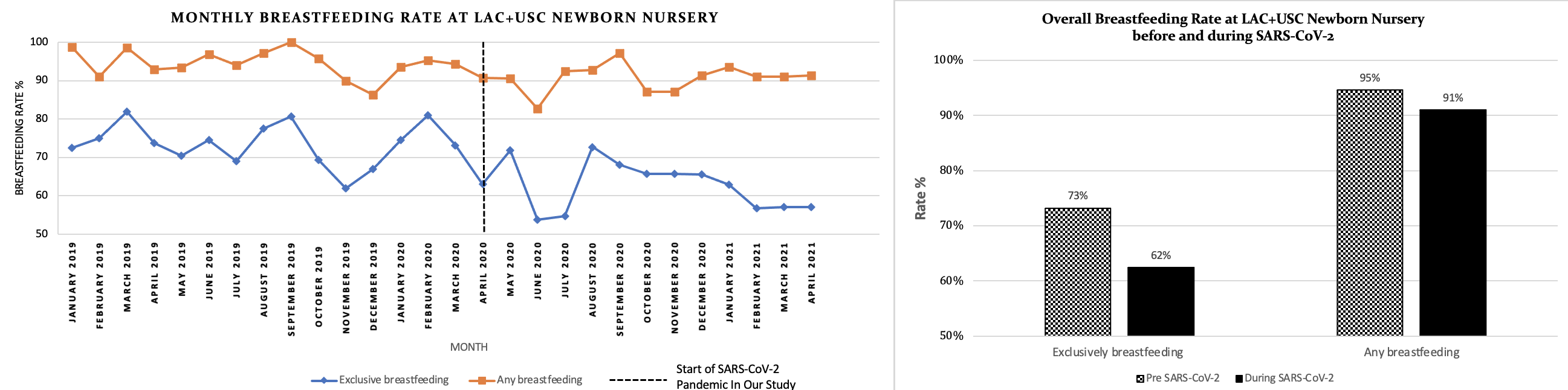 Breastfeeding Rate at LAC+USC Medical Center before and during SARS-CoV-2
Breastfeeding Rate at LAC+USC Medical Center before and during SARS-CoV-2
Exclusive breastfeeding for the first six months of life is recommended by the American Academy of Pediatrics and the Centers for Disease Control for its benefits to infant immunity, maternal-child bonding, and long-term health. While these benefits are well studied, the SARS-CoV-2 pandemic raises questions about the safety of breastfeeding among SARS-CoV-2-positive mothers. In addition, the pandemic’s effects on hospital staffing, patient-provider facetime, and healthcare access may impact breastfeeding rates.
Objective:
This study aims to explore the effect of the SARS-CoV-2 pandemic on breastfeeding in the newborn nursery at a single center.
Design/Methods:
This is a retrospective cohort study comparing breastfeeding rates between neonates at LAC+USC Medical Center Newborn Nursery from January 2019 to April 2021. We defined the pre-SARS-CoV- 2 group as all neonates born prior to April 2020, and the during-SARS-CoV-2 group as those born from April 2020 to April 2021. Maternal data gathered included gravidity and parity, ethnicity, age, mode of delivery, and pregnancy complications. Infant data gathered included gestational age, birth weight, sex, and hyperbilirubinemia requiring intensive phototherapy. Newborns with maternal contraindications to breastfeeding, such as positive toxicology screen, positive HIV status, incarceration, and placement in foster care were excluded. Rates of exclusive breastfeeding and any breastfeeding were calculated for each month within this time period and compared using T-test. P-value less than 0.05 was considered significant.
Results:
Of the 964 newborns screened in the pre-SARS-CoV-2 cohort, 913 were included. Of the 800 screened during-SARS-CoV-2 cohort, 763 newborns were included. There were no significant differences in the demographics between the two cohorts (Table 1). We found a 11% decrease in the rate of exclusive breastfeeding (p < 0.05) and a 4% decrease in any breastfeeding (p < 0.05) during the SARS-CoV-2 period (Image 1).
Conclusion(s):
The SARS-CoV-2 pandemic had a negative impact on the rates of both exclusive breastfeeding and any breastfeeding among newborns in the normal nursery from a single center in Los Angeles. These results prompted the creation of a specific task force to counter the detrimental effect of the pandemic on breastfeeding. Prospective studies would be useful in assessing the long-term effects of the SARS-CoV-2 pandemic on breastfeeding rates and associated effects on infant immunity, maternal-child bonding, and long- term health.
Table
 Maternal and Neonatal Demographics and Characteristics
Maternal and Neonatal Demographics and CharacteristicsImage 1.
 Breastfeeding Rate at LAC+USC Medical Center before and during SARS-CoV-2
Breastfeeding Rate at LAC+USC Medical Center before and during SARS-CoV-2