General Pediatrics: Primary Care/Prevention
Category: Abstract Submission
General Pediatrics V
109 - The First Ten Minutes: Emergency Preparedness in the Outpatient Pediatric Office
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 109
Publication Number: 109.409
Publication Number: 109.409
Shareen F. Kelly, St. Christopher's Hospital for Children, Philadelphia, PA, United States; Catherine Clauss, St. Christopher's Hospital for Children, Riverton, NJ, United States; Anna Pak, Drexel University College of Medicine, Philadelphia, PA, United States; Michele Bresler, St. Christopher's Hospital for Children, Philadelphia, PA, United States; Paige Jarmuz, St. Christopher's Hospital for Children, Philadelphia, PA, United States; Sujung Kim, St. Christopher's Hospital for Children, Philadelphia, PA, United States; Brian Novi, St. Christopher's Hospital for Children, Philadelphia, PA, United States

Shareen F. Kelly, MD
Residency Program Director
St. Christopher's Hospital for Children
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Acutely ill or injured children who present to their primary care office may need timely escalation of care above what the primary office can offer. Practitioners may not feel adequately prepared or comfortable handling these cases. Training in emergency preparedness during residency will enable trainees to deliver better care and be more comfortable doing it.
Objective: We used low fidelity simulation of 8 commonly occurring pediatric scenarios to prepare our trainees to triage children in need of acute care, escalate care and/or begin the treatment needed.
Design/Methods: Using pre- and post-simulation surveys, we measured comfort level with management of the 8 scenarios and the use of equipment common in a primary office setting. Comfort in participation, leadership and the feedback aspects were also measured. Simulated cases are presented 1-2 times monthly to residents and students during the acute care rotation in our general pediatrics office. Junior residents and medical students participated in the scenarios and senior residents on the 'teach' rotation provided the debrief and teaching related to content.
Results: Prior to their participation in our project, almost half (45%) of the trainees had no exposure to emergency scenarios in the outpatient setting. Of the scenarios and associated skills, management of upper and lower airway distress was where the trainees felt most comfortable ( >50% answering somewhat or very comfortable). Comfort with participation in simulation increased between the pre- and post-surveys from 40% to 71%; similarly, comfort in receiving feedback rose from 85% to 100%. Most trainees did not feel comfortable leading the scenarios (86 and 95% respectively), but they had similar comfort with asking for help (75 and 71% respectively). Following simulation, 87.5% of trainees said they felt somewhat or very comfortable with the content of the scenario they had participated in.Conclusion(s): There are many areas where trainees do not have comfort with acute scenarios and the use of equipment in the primary care office. We anticipate increasing confidence as this training continues. Simulation resulted in increased comfort in participation and receiving feedback after the simulation. Trainees reported comfort in management of the scenario they had just participated in.
Summary of Simulation Participants' Experiences.png) Description of participants, their experience prior to and after simulation.
Description of participants, their experience prior to and after simulation.
Comfort with Scenarios, Equipment and Roles Pre- and Post-simulation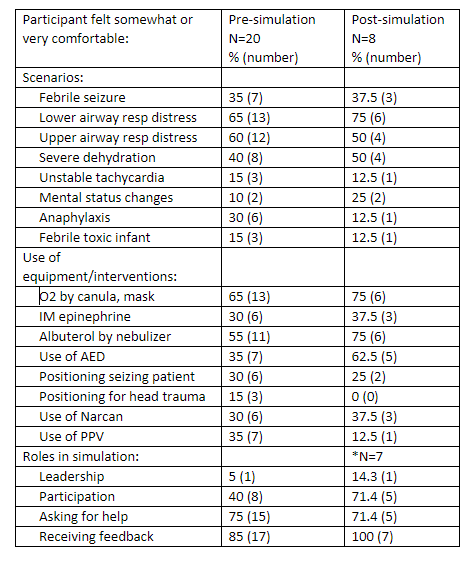 Participants' comfort levels with educational content, commonly used equipment and their roles before and after simulation.
Participants' comfort levels with educational content, commonly used equipment and their roles before and after simulation.
Objective: We used low fidelity simulation of 8 commonly occurring pediatric scenarios to prepare our trainees to triage children in need of acute care, escalate care and/or begin the treatment needed.
Design/Methods: Using pre- and post-simulation surveys, we measured comfort level with management of the 8 scenarios and the use of equipment common in a primary office setting. Comfort in participation, leadership and the feedback aspects were also measured. Simulated cases are presented 1-2 times monthly to residents and students during the acute care rotation in our general pediatrics office. Junior residents and medical students participated in the scenarios and senior residents on the 'teach' rotation provided the debrief and teaching related to content.
Results: Prior to their participation in our project, almost half (45%) of the trainees had no exposure to emergency scenarios in the outpatient setting. Of the scenarios and associated skills, management of upper and lower airway distress was where the trainees felt most comfortable ( >50% answering somewhat or very comfortable). Comfort with participation in simulation increased between the pre- and post-surveys from 40% to 71%; similarly, comfort in receiving feedback rose from 85% to 100%. Most trainees did not feel comfortable leading the scenarios (86 and 95% respectively), but they had similar comfort with asking for help (75 and 71% respectively). Following simulation, 87.5% of trainees said they felt somewhat or very comfortable with the content of the scenario they had participated in.Conclusion(s): There are many areas where trainees do not have comfort with acute scenarios and the use of equipment in the primary care office. We anticipate increasing confidence as this training continues. Simulation resulted in increased comfort in participation and receiving feedback after the simulation. Trainees reported comfort in management of the scenario they had just participated in.
Summary of Simulation Participants' Experiences
.png) Description of participants, their experience prior to and after simulation.
Description of participants, their experience prior to and after simulation.Comfort with Scenarios, Equipment and Roles Pre- and Post-simulation
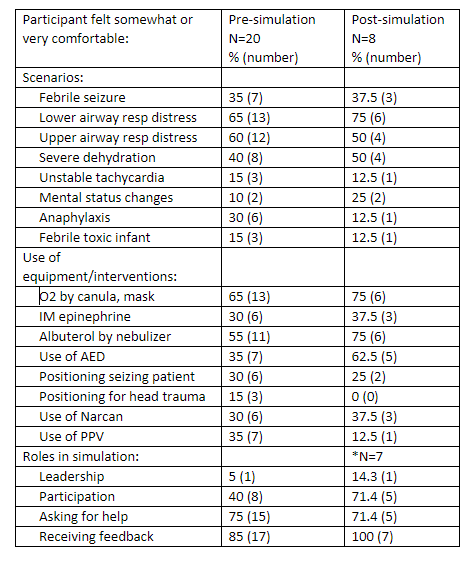 Participants' comfort levels with educational content, commonly used equipment and their roles before and after simulation.
Participants' comfort levels with educational content, commonly used equipment and their roles before and after simulation.