Neonatal General
Category: Abstract Submission
Neonatology General 9: Congenital Anomalies - CV
312 - Use of vasopressors for septic shock in the Neonatal Intensive Care Unit
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 312
Publication Number: 312.441
Publication Number: 312.441
Henry P. Foote, Duke University Medical Center, Durham, NC, United States; Daniel Benjamin, Clemson University, Lottsburg, VA, United States; Rachel G. Greenberg, Duke Clinical Research Institute, Durham, NC, United States; Reese H. Clark, MEDNAX, Myrtle Beach, SC, United States; Christoph Hornik, Duke University School of Medicine, Durham, NC, United States
- HF
Henry P. Foote, MD
Pediatric Cardiology Fellow
Duke University Medical Center
Durham, North Carolina, United States
Presenting Author(s)
Background: Infants in the Neonatal Intensive Care Unit (NICU) are at high risk for sepsis, which can progress to septic shock with associated cardiovascular dysfunction, severe morbidity, and mortality. Epinephrine is recommended as the first line vasopressor for septic shock in older children, but the optimal vasopressor therapy for septic shock in infants is not well defined.
Objective: To describe outcomes for infants with septic shock based on type of vasopressor administered.
Design/Methods: We performed a cohort study of inborn infants less than 120 days old with an episode of septic shock who were discharged from NICUs managed by the Pediatrix Medical group from 2010 – 2018. We defined an episode of septic shock as positive blood culture with an organism not typically considered a contaminant and concomitant new vasopressor requirement, with use starting between one day prior and two days after positive culture. Episodes started on the first day of qualifying vasopressor exposure and ended on the final day of continuous vasopressor exposure or if death occurred. Only the first episode was included for each infant. We evaluated outcomes based on combination of vasopressor therapy received during an episode using descriptive analyses and logistic regression for unadjusted odds ratios. We analyzed systemic hydrocortisone only when it was co-administered with other vasopressors.
Results: We identified 1592 infants across 175 NICUs; mortality was 50% (Table 1). The median (IQV) gestational age was 25 weeks (24, 28). Episodes began on median postnatal day 8 (1, 15) and lasted for 3 days (1, 5). Dopamine was the most used vasopressor (92% of episodes) with epinephrine (28%) and dobutamine (24%) also frequently used (Table 2). Hydrocortisone was co-administered with a vasopressor in 38% of episodes. Compared to infants who were treated with dopamine alone, unadjusted odds of mortality were significantly higher for those who received epinephrine alone (OR 4.8 [CI: 2.9 – 8.1]), or the combinations of dobutamine and dopamine (OR 2.4 [1.7 – 3.3]), epinephrine and dopamine (OR 5.3 [3.7 – 7.6]), or epinephrine, dobutamine, and dopamine together (OR 13.3 [7.7 – 23.1]) (Table 3). Mortality was numerically but not statistically higher for infants who received hydrocortisone (OR 1.2 [0.98 – 1.5] compared to those who did not).Conclusion(s): Infants with septic shock are at high risk for mortality. The use of epinephrine as either a solo agent or in combination therapy was associated with significantly worse outcomes. Further studies are needed to guide therapy for these critically ill infants.
Table 1. Demographics and overall outcomes for infants with septic shock.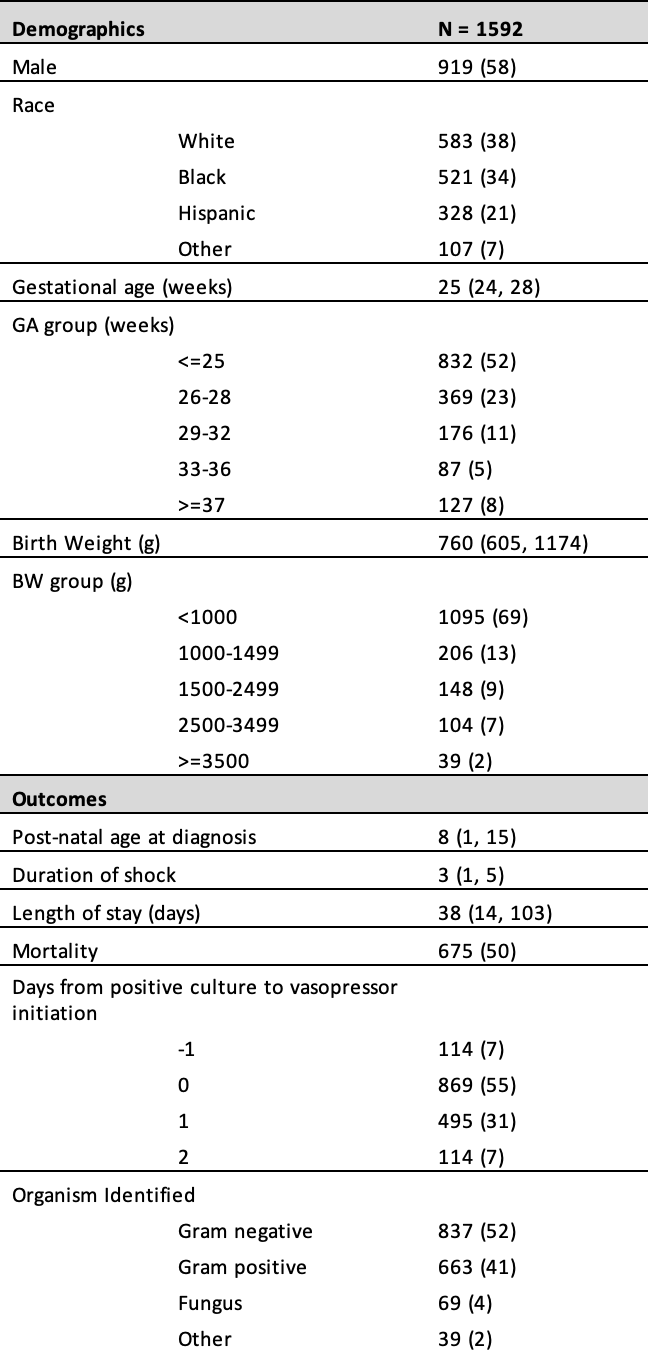 Continuous variables described using median (interquartile values) and categorical variables described as frequencies (percentage).
Continuous variables described using median (interquartile values) and categorical variables described as frequencies (percentage).
Table 2. Overall usage of vasopressors and hydrocortisone for septic shock..png) Hydrocortisone assessed only when it was co-administered with other vasopressors. Continuous variables described using median (interquartile values) and categorical variables described as frequencies (percentage).
Hydrocortisone assessed only when it was co-administered with other vasopressors. Continuous variables described using median (interquartile values) and categorical variables described as frequencies (percentage).
Objective: To describe outcomes for infants with septic shock based on type of vasopressor administered.
Design/Methods: We performed a cohort study of inborn infants less than 120 days old with an episode of septic shock who were discharged from NICUs managed by the Pediatrix Medical group from 2010 – 2018. We defined an episode of septic shock as positive blood culture with an organism not typically considered a contaminant and concomitant new vasopressor requirement, with use starting between one day prior and two days after positive culture. Episodes started on the first day of qualifying vasopressor exposure and ended on the final day of continuous vasopressor exposure or if death occurred. Only the first episode was included for each infant. We evaluated outcomes based on combination of vasopressor therapy received during an episode using descriptive analyses and logistic regression for unadjusted odds ratios. We analyzed systemic hydrocortisone only when it was co-administered with other vasopressors.
Results: We identified 1592 infants across 175 NICUs; mortality was 50% (Table 1). The median (IQV) gestational age was 25 weeks (24, 28). Episodes began on median postnatal day 8 (1, 15) and lasted for 3 days (1, 5). Dopamine was the most used vasopressor (92% of episodes) with epinephrine (28%) and dobutamine (24%) also frequently used (Table 2). Hydrocortisone was co-administered with a vasopressor in 38% of episodes. Compared to infants who were treated with dopamine alone, unadjusted odds of mortality were significantly higher for those who received epinephrine alone (OR 4.8 [CI: 2.9 – 8.1]), or the combinations of dobutamine and dopamine (OR 2.4 [1.7 – 3.3]), epinephrine and dopamine (OR 5.3 [3.7 – 7.6]), or epinephrine, dobutamine, and dopamine together (OR 13.3 [7.7 – 23.1]) (Table 3). Mortality was numerically but not statistically higher for infants who received hydrocortisone (OR 1.2 [0.98 – 1.5] compared to those who did not).Conclusion(s): Infants with septic shock are at high risk for mortality. The use of epinephrine as either a solo agent or in combination therapy was associated with significantly worse outcomes. Further studies are needed to guide therapy for these critically ill infants.
Table 1. Demographics and overall outcomes for infants with septic shock.
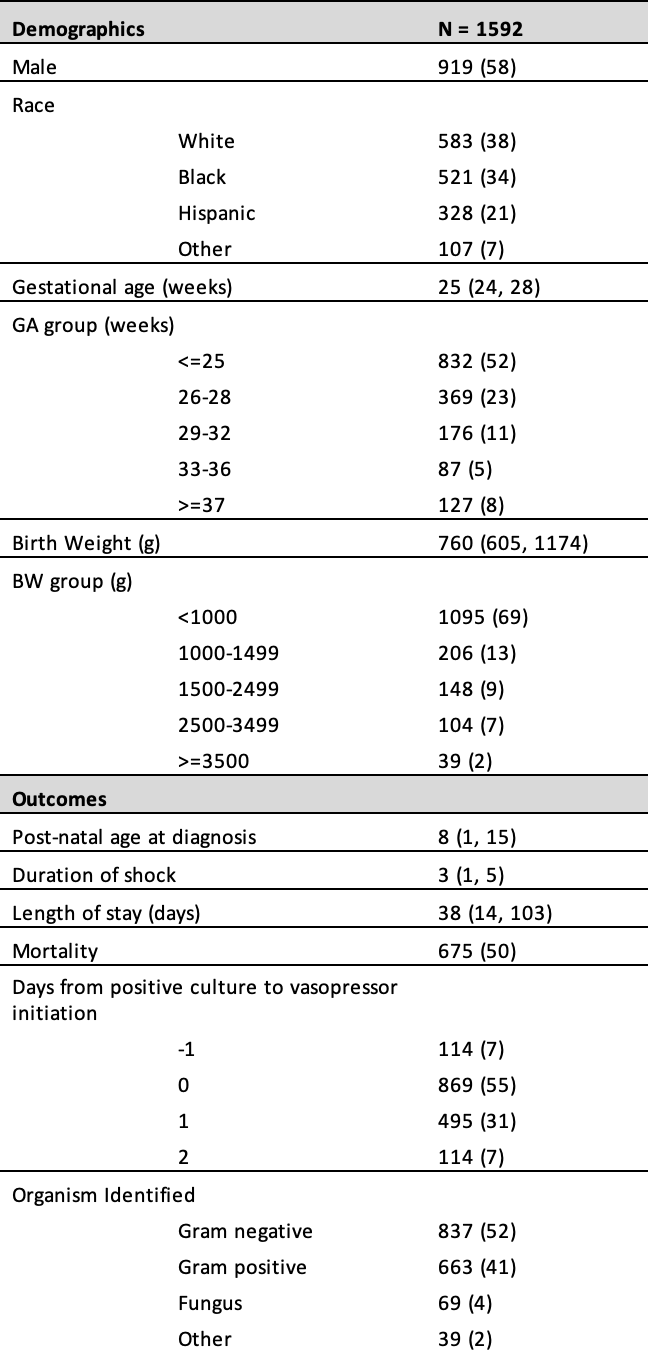 Continuous variables described using median (interquartile values) and categorical variables described as frequencies (percentage).
Continuous variables described using median (interquartile values) and categorical variables described as frequencies (percentage).Table 2. Overall usage of vasopressors and hydrocortisone for septic shock.
.png) Hydrocortisone assessed only when it was co-administered with other vasopressors. Continuous variables described using median (interquartile values) and categorical variables described as frequencies (percentage).
Hydrocortisone assessed only when it was co-administered with other vasopressors. Continuous variables described using median (interquartile values) and categorical variables described as frequencies (percentage).