Neonatal General
Category: Abstract Submission
Neonatology General 11: Lung
370 - Towards optimal high CPAP pressures as post-extubation support in preterm neonates: A retrospective cohort study
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 370
Publication Number: 370.440
Publication Number: 370.440
Lana Khalid, 1Department of Pediatrics, McMaster University, Hamilton, ON, Canada, Hamilton, ON, Canada; Said Salim Nasser S. Al Balushi, Mcmaster University, Hamilton, ON, Canada; Nandita Manoj, McMaster University Michael G. DeGroote School of Medicine, Markham, ON, Canada; Sufyan Rather, McMaster University Michael G. DeGroote School of Medicine, Brampton, ON, Canada; Heather Johnson, McMaster University Michael G. DeGroote School of Medicine, dundas, ON, Canada; Laura Strauss, Hamilton Health Sciences, Hamilton, ON, Canada; Sourabh Dutta, PGIMER, Chandigarh, Chandigarh, India; Amit Mukerji, McMaster University, Hamilton, ON, Canada

Amit Mukerji, MD, MSc
Associate Professor
McMaster University
Hamilton, Ontario, Canada
Presenting Author(s)
Background: High CPAP (≥9 cmH2O) is increasingly utilized to facilitate earlier extubation from invasive mechanical ventilation in preterm neonates. However, the optimal distending pressure level when extubating from high pressures on invasive ventilation remains unknown.
Objective: To identify whether the initial choice of distending pressure during High CPAP, in relation to pre-extubation mean airway pressure (Paw), is associated with clinical outcomes.
Design/Methods: Preterm neonates of GA < 29 weeks free of any congenital/genetic abnormalities admitted to a single tertiary centre between Jan 1, 2011-Dec 31, 2020 were included if they were extubated from high Paw ≥9 cmH2O on invasive ventilation. The cohort was classified into Higher CPAP (initial distending pressure between +2 and +3 cmH2O in relation to pre-extubation Paw) and Equivalent CPAP (-1 to +1 cmH2O in relation to pre-extubation Paw). Primary outcome was failure of CPAP within 7 days (a composite of need for intubation, escalation to alternate non-invasive mode, or use of CPAP > +3 cmH2O in relation to pre-extubation Paw). Categorical variables were reported as percentages while continuous variables are reported as median (IQR), with appropriate corresponding univariate analyses. A logistic regression model was only performed for the primary outcome.
Results: Out of 874 infants screened, 168 were eligible for analysis – of whom 31 were in the Higher CPAP group while 137 comprised the Equivalent CPAP group. With the exception of pre-extubation invasive mode, there were no differences in baseline variables (Table 1). The median (IQR) distending pressure levels were 13 (12-14) and 10 (10-12) cmH2O in the two groups, respectively. There was no difference in the primary outcome, both unadjusted (Table 2) and after adjustment for potential confounders (aOR 0.76 [95% CI 0.30 – 1.91; P = 0.56]). Interestingly, the intubation rate was significantly lower with use of Higher CPAP levels, while 37% of patients extubated to Higher CPAP levels were de-escalated to Equivalent CPAP levels within 7 days (Table 2). There were no differences in safety outcomes (Table 2), nor was the primary outcome different in subgroup analyses (Table 3).Conclusion(s): These data suggest that when extubating from Paw≥9 cmH2O, use of initial distending pressures 2-3 cmH2O higher that pre-extubation Paw does not alter CPAP failure but may reduce re-intubation rates.
Table 1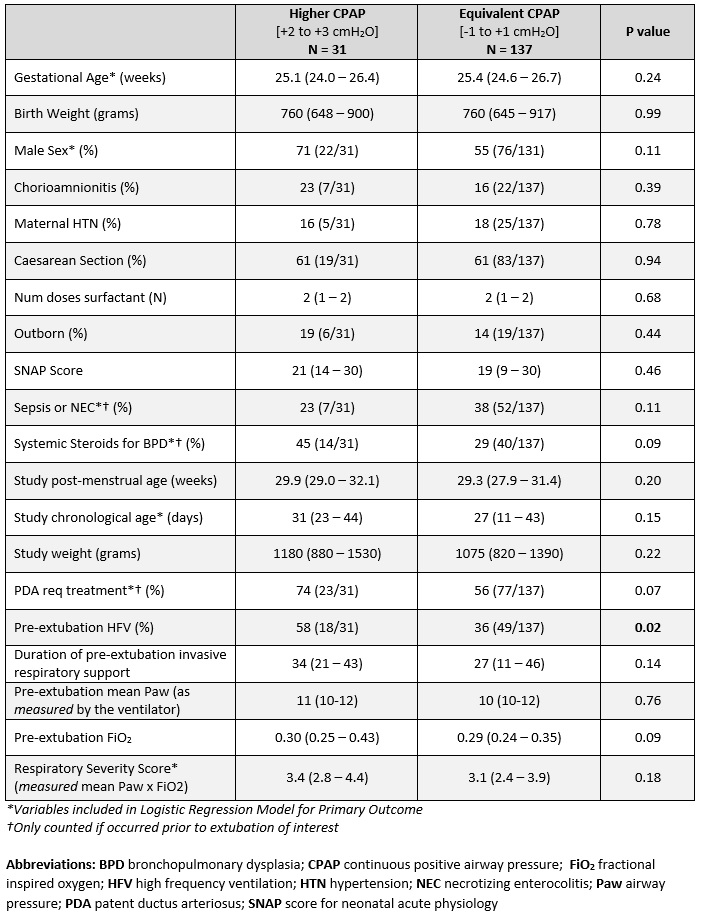 Baseline variables
Baseline variables
Table 2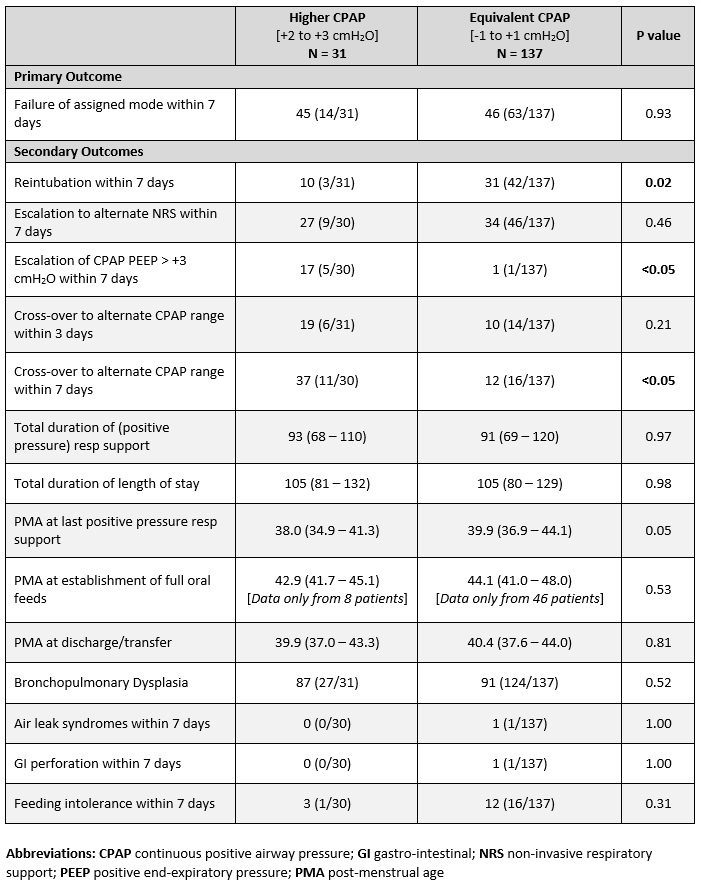 Clinical outcomes [Unadjusted]
Clinical outcomes [Unadjusted]
Objective: To identify whether the initial choice of distending pressure during High CPAP, in relation to pre-extubation mean airway pressure (Paw), is associated with clinical outcomes.
Design/Methods: Preterm neonates of GA < 29 weeks free of any congenital/genetic abnormalities admitted to a single tertiary centre between Jan 1, 2011-Dec 31, 2020 were included if they were extubated from high Paw ≥9 cmH2O on invasive ventilation. The cohort was classified into Higher CPAP (initial distending pressure between +2 and +3 cmH2O in relation to pre-extubation Paw) and Equivalent CPAP (-1 to +1 cmH2O in relation to pre-extubation Paw). Primary outcome was failure of CPAP within 7 days (a composite of need for intubation, escalation to alternate non-invasive mode, or use of CPAP > +3 cmH2O in relation to pre-extubation Paw). Categorical variables were reported as percentages while continuous variables are reported as median (IQR), with appropriate corresponding univariate analyses. A logistic regression model was only performed for the primary outcome.
Results: Out of 874 infants screened, 168 were eligible for analysis – of whom 31 were in the Higher CPAP group while 137 comprised the Equivalent CPAP group. With the exception of pre-extubation invasive mode, there were no differences in baseline variables (Table 1). The median (IQR) distending pressure levels were 13 (12-14) and 10 (10-12) cmH2O in the two groups, respectively. There was no difference in the primary outcome, both unadjusted (Table 2) and after adjustment for potential confounders (aOR 0.76 [95% CI 0.30 – 1.91; P = 0.56]). Interestingly, the intubation rate was significantly lower with use of Higher CPAP levels, while 37% of patients extubated to Higher CPAP levels were de-escalated to Equivalent CPAP levels within 7 days (Table 2). There were no differences in safety outcomes (Table 2), nor was the primary outcome different in subgroup analyses (Table 3).Conclusion(s): These data suggest that when extubating from Paw≥9 cmH2O, use of initial distending pressures 2-3 cmH2O higher that pre-extubation Paw does not alter CPAP failure but may reduce re-intubation rates.
Table 1
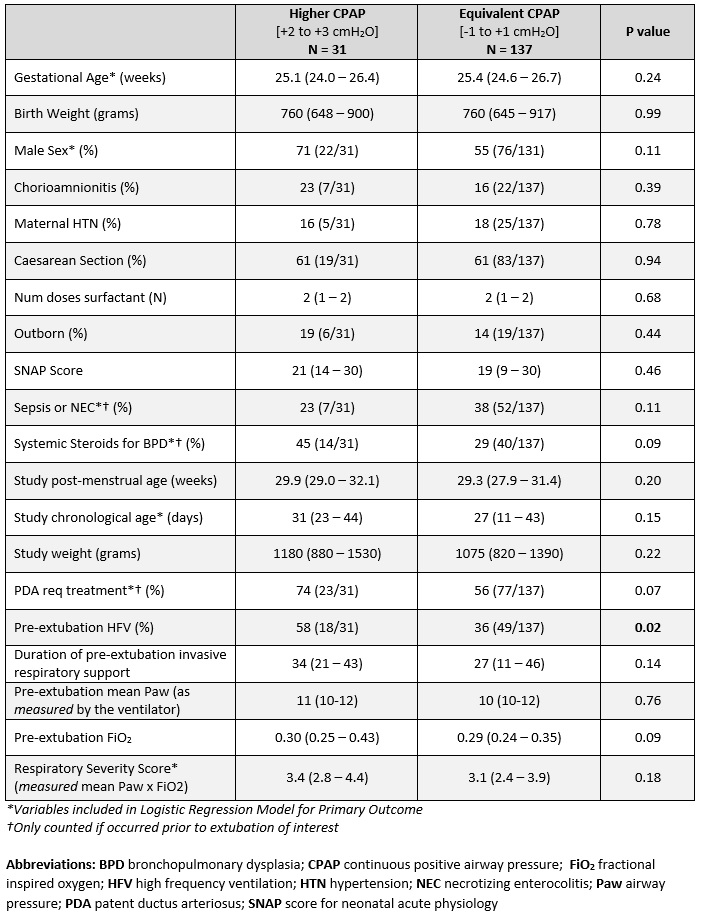 Baseline variables
Baseline variablesTable 2
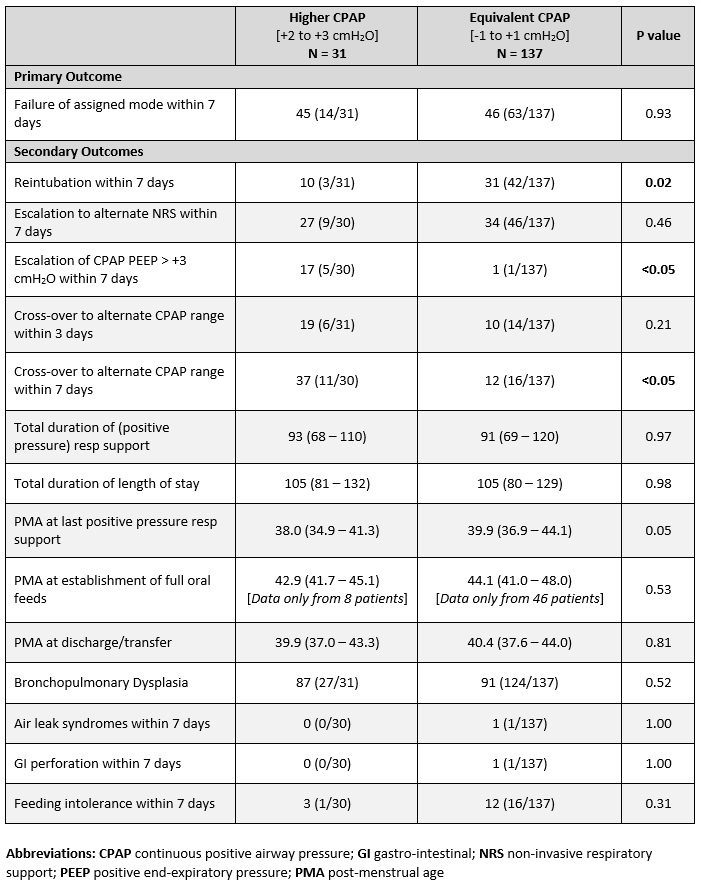 Clinical outcomes [Unadjusted]
Clinical outcomes [Unadjusted]