Neonatal General
Category: Abstract Submission
Neonatology General 10: ID - Inflammation - COVID
330 - Trends in COVID-19 Diagnoses and Outcomes in Hospitalized Infants
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 330
Publication Number: 330.439
Publication Number: 330.439
Elizabeth B. Heyward, Duke University School of Medicine, North Charleston, SC, United States; Reese H. Clark, MEDNAX, Myrtle Beach, SC, United States; Brian Smith, Duke University School of Medicine, Durham, NC, United States; Daniel Benjamin, Duke University School of Medicine, Durham, NC, United States; Kaashif A. Ahmad, MEDNAX, Houston, TX, United States; Courtney K. Blackwell, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Rachel G. Greenberg, Duke Clinical Research Institute, Durham, NC, United States

Elizabeth B. Heyward, MD
Neonatology Fellow
Duke University School of Medicine
North Charleston, South Carolina, United States
Presenting Author(s)
Background: While pregnant women and infants are historically vulnerable populations during an infectious disease pandemic, the extent to which COVID-19 in the pre- and perinatal time periods changes the risk of adverse maternal and neonatal outcomes remains unclear.
Objective: To characterize the prevalence of COVID-19 diagnosis among mothers with infants hospitalized in the neonatal intensive care unit (NICU), and demographics and outcomes of these infants with SARS-CoV-2 exposure in utero.
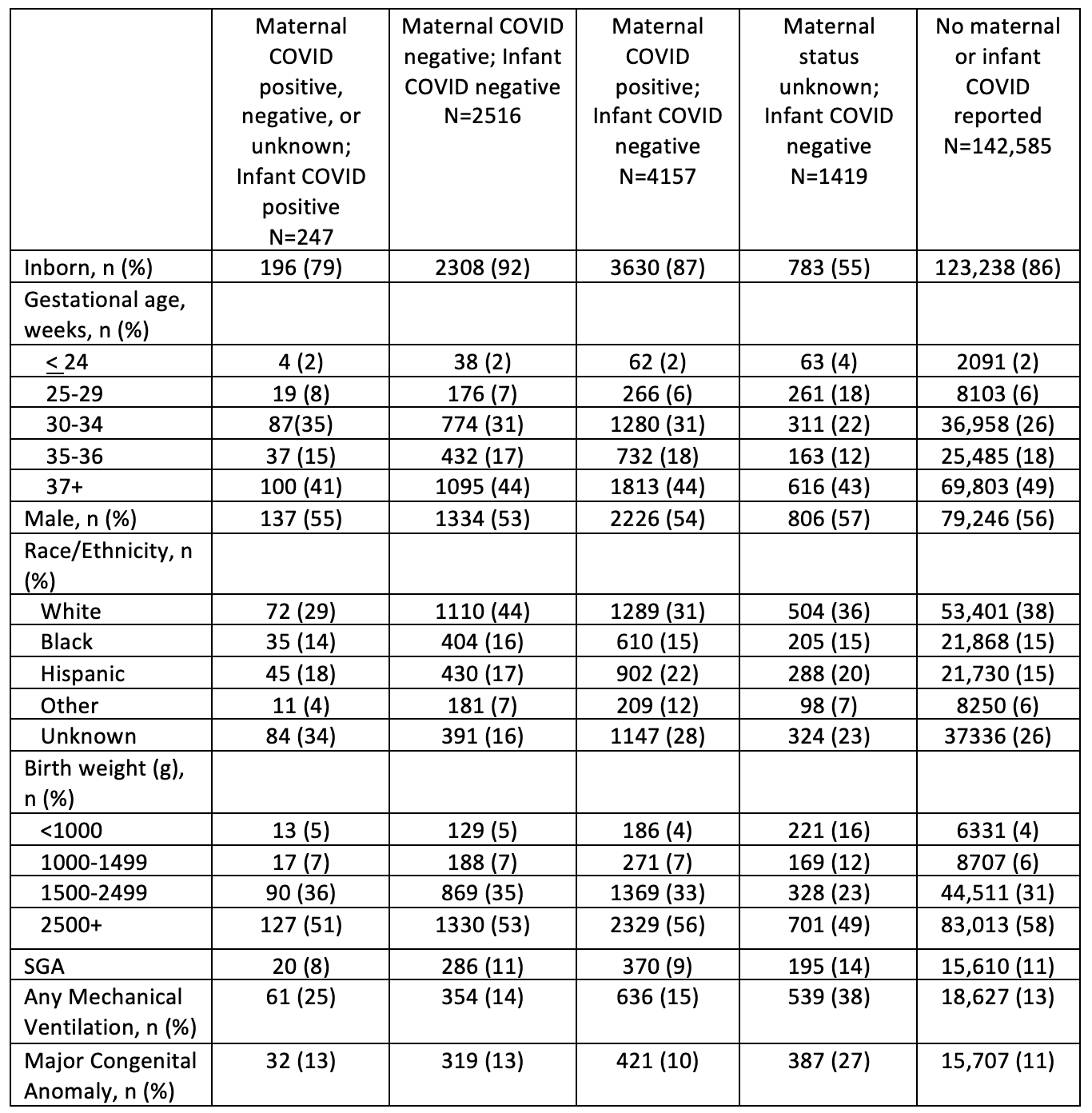
Design/Methods: Cohort study of infants discharged from Pediatrix Medical Group NICUs between January 2020 and September 2021. We defined 5 infant groups based on maternal SARS-CoV-2 infection status and infant diagnosis and testing: 1) “Maternal COVID positive, negative, or unknown; Infant COVID positive,” if the infant had a COVID-19 diagnosis or positive test for SARS-CoV-2 regardless of maternal COVID status; 2) “Maternal COVID negative; Infant COVID negative,” if the mother and infant had a negative test; 3) “Maternal COVID positive; Infant COVID negative,” if the mother had a positive test and the infant had a negative test; 4) “Maternal status unknown; Infant COVID negative,” if the mother had unknown COVID-19 status and the infant had a negative test; and 5) "No maternal or infant COVID reported,” if mother and infant had no reported COVID-related diagnosis or test. We compared demographics, clinical characteristics, and outcomes, including postnatal day of discharge, death, severe intraventricular hemorrhage (IVH), severe retinopathy of prematurity (ROP), and necrotizing enterocolitis (NEC).
Results:
In the study period, 150,924 infants were discharged from 294 NICUs. Most (95%) of these infants had no reported COVID-related diagnosis or test. Only 247 ( < 1%) of infants tested positive for COVID-19. The trends in testing of mothers of infants in our cohort reflected temporal surges reported in the general population (Figure 1). Infants positive for COVID-19 had similar demographic and clinical characteristics to other groups (Table 2); infants with unknown maternal status and negative testing were more premature, more likely outborn, and had longer hospital stays, likely reflecting testing on transfer or pre-procedure. Adverse outcomes were rare, and mortality was similar across groups (Table 3).
Conclusion(s): In this large cohort of hospitalized newborn infants, most had no known exposure to COVID-19. The demographics between the infant groups were similar, and mortality was rare. Further studies are needed to evaluate the long-term effects of COVID-19 in this population.
Figure 1: Maternal and Infant COVID-19 Trends from January 2020 to September 2021.png)
Table 2: Demographics and clinical characteristics of infants hospitalized in NICU with COVID-19 Exposure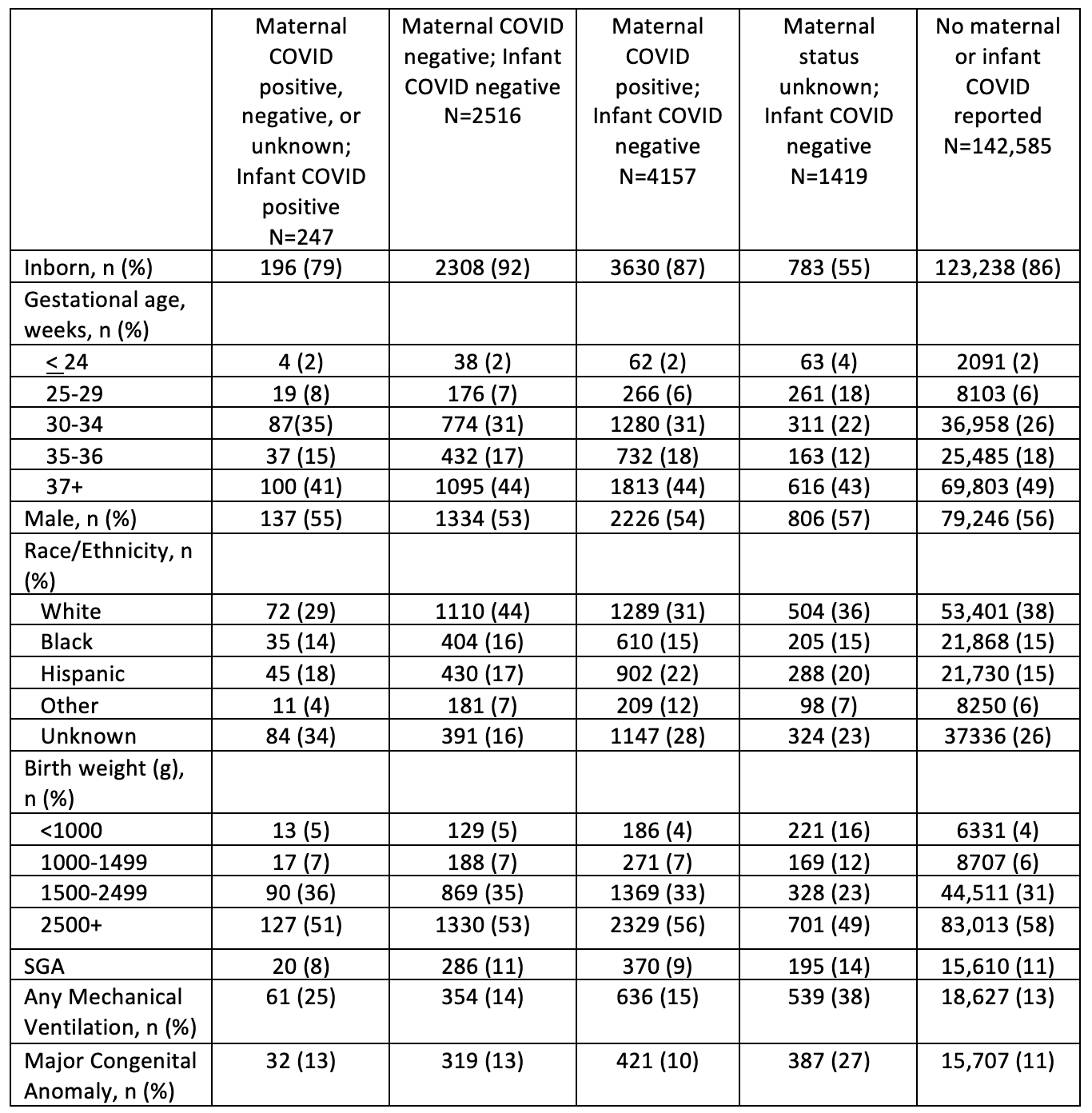
Objective: To characterize the prevalence of COVID-19 diagnosis among mothers with infants hospitalized in the neonatal intensive care unit (NICU), and demographics and outcomes of these infants with SARS-CoV-2 exposure in utero.
Design/Methods: Cohort study of infants discharged from Pediatrix Medical Group NICUs between January 2020 and September 2021. We defined 5 infant groups based on maternal SARS-CoV-2 infection status and infant diagnosis and testing: 1) “Maternal COVID positive, negative, or unknown; Infant COVID positive,” if the infant had a COVID-19 diagnosis or positive test for SARS-CoV-2 regardless of maternal COVID status; 2) “Maternal COVID negative; Infant COVID negative,” if the mother and infant had a negative test; 3) “Maternal COVID positive; Infant COVID negative,” if the mother had a positive test and the infant had a negative test; 4) “Maternal status unknown; Infant COVID negative,” if the mother had unknown COVID-19 status and the infant had a negative test; and 5) "No maternal or infant COVID reported,” if mother and infant had no reported COVID-related diagnosis or test. We compared demographics, clinical characteristics, and outcomes, including postnatal day of discharge, death, severe intraventricular hemorrhage (IVH), severe retinopathy of prematurity (ROP), and necrotizing enterocolitis (NEC).
Results:
In the study period, 150,924 infants were discharged from 294 NICUs. Most (95%) of these infants had no reported COVID-related diagnosis or test. Only 247 ( < 1%) of infants tested positive for COVID-19. The trends in testing of mothers of infants in our cohort reflected temporal surges reported in the general population (Figure 1). Infants positive for COVID-19 had similar demographic and clinical characteristics to other groups (Table 2); infants with unknown maternal status and negative testing were more premature, more likely outborn, and had longer hospital stays, likely reflecting testing on transfer or pre-procedure. Adverse outcomes were rare, and mortality was similar across groups (Table 3).
Conclusion(s): In this large cohort of hospitalized newborn infants, most had no known exposure to COVID-19. The demographics between the infant groups were similar, and mortality was rare. Further studies are needed to evaluate the long-term effects of COVID-19 in this population.
Figure 1: Maternal and Infant COVID-19 Trends from January 2020 to September 2021
.png)
Table 2: Demographics and clinical characteristics of infants hospitalized in NICU with COVID-19 Exposure