Children with Chronic Conditions
Category: Abstract Submission
Children with Chronic Conditions IV
612 - Pediatrician perspectives on barriers and facilitators to discharge instruction comprehension and adherence for parents of children with medical complexity
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 612
Publication Number: 612.404
Publication Number: 612.404
Alexander F. Glick, NYU Grossman School of Medicine, New York, NY, United States; H. Shonna Yin, NYU Grossman School of Medicine, New York City, NY, United States; Benjamin Silva, New York University Grossman School of Medicine, New York, NY, United States; Julia S. Turock, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Jonathan S. Farkas, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Avani C. Modi, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Emily J. Goodwin, Children's Mercy Kansas City, Kansas City, MO, United States; Vincent Huynh, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Hannah S. Famiglietti, New York University Grossman School of Medicine, New York, NY, United States; Victoria V. Dickson, NYU Meyers College of Nursing, New York, NY, United States

Alexander Glick, MD, MS
Assistant Professor of Pediatrics
NYU Grossman School of Medicine
New York, New York, United States
Presenting Author(s)
Background: High rates of post-hospitalization readmissions and errors are observed in children with medical complexity (CMC); poor parent comprehension and adherence to inpatient discharge instructions likely contribute to these errors. Pediatrician views on common barriers and facilitators to parent comprehension and adherence are understudied.
Objective: To examine pediatrician perspectives on barriers and facilitators experienced by parents in comprehension of and adherence to discharge instructions for CMC after an inpatient hospitalization.
Design/Methods: We conducted a qualitative, descriptive study of a purposeful sample of attending pediatricians (n=20) caring for CMC in inpatient settings (US and Canada) and belonging to listservs for pediatric hospitalists/complex care providers. We used maximum variation sampling to ensure heterogeneity (e.g., hospital, region). A multidisciplinary team designed and piloted a semi-structured interview guide with members of the target population. Trained team members conducted semi-structured interviews via phone or video call. Interviews were audiorecorded and transcribed. We analyzed transcripts using content analysis (Dedoose Version 9.0.17). We derived codes a priori from a conceptual framework (based on the Pediatric Self-Management Model and existing literature) and a preliminary analysis of transcripts. We applied codes and subsequently identified emerging themes from transcripts. Methodologic rigor was supported via member checking, peer debriefing, and 2 coders for a subset of transcripts.
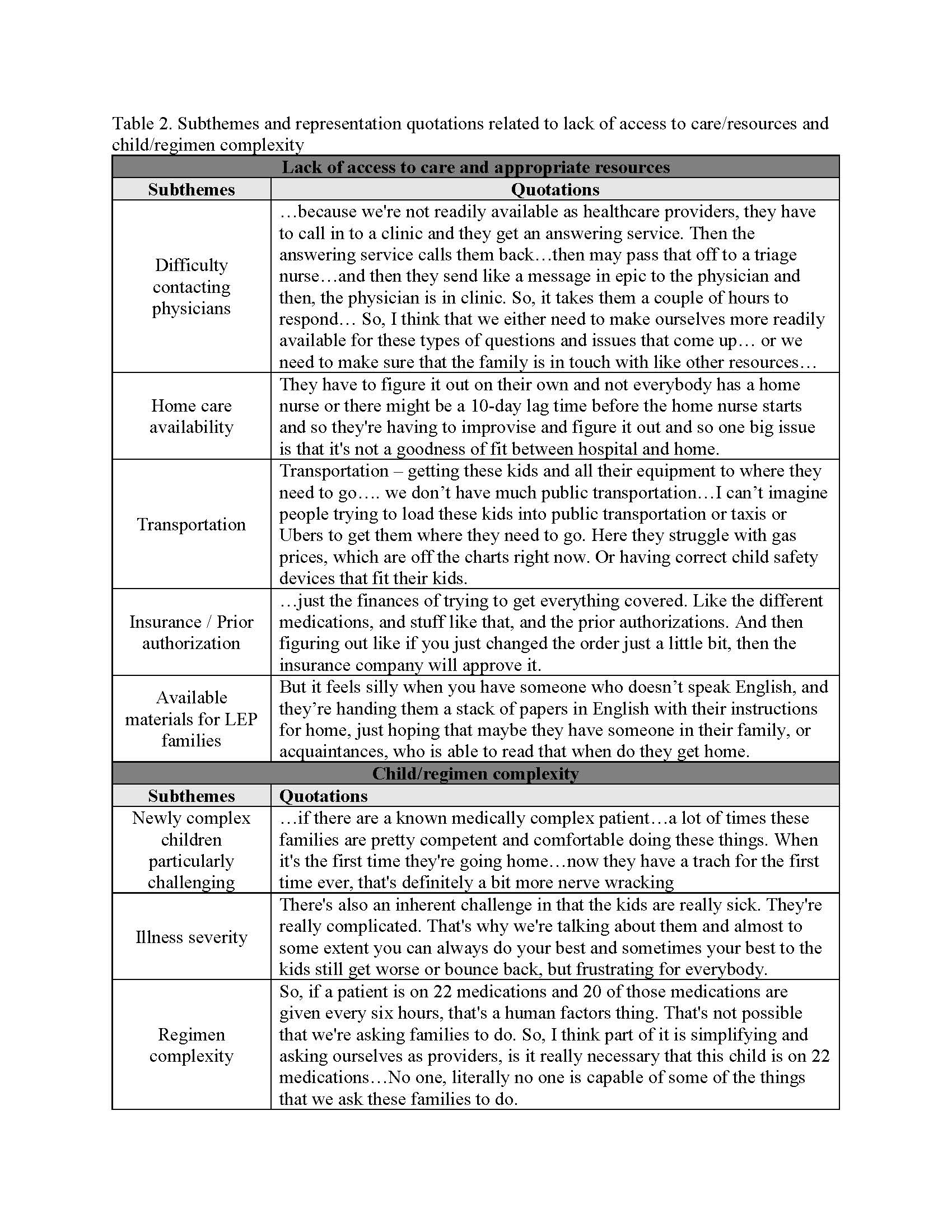
Results: We identified 4 themes among participants (Table 1): 1) Lack of access to care and appropriate resources, including physician access, home care, transportation, insurance, and available materials for families with limited English proficiency (Table 2); 2) Challenges associated with child and regimen complexity (especially for children who are newly medically complex) (Table 2); 3) Importance of teamwork and relationship building (Table 3); and 4) Need for a patient- and family-centered and structured approach to discharge planning, including accommodating schedules/competing priorities, understanding support systems, ensuring enough time for discharge counseling and comfort with post-discharge care, and tailoring education (Table 3).Conclusion(s): Pediatricians identified several barriers and facilitators to discharge instruction comprehension and adherence for parents of CMC. Next steps include assessment of parent perspectives and development of intervention strategies.
Table 1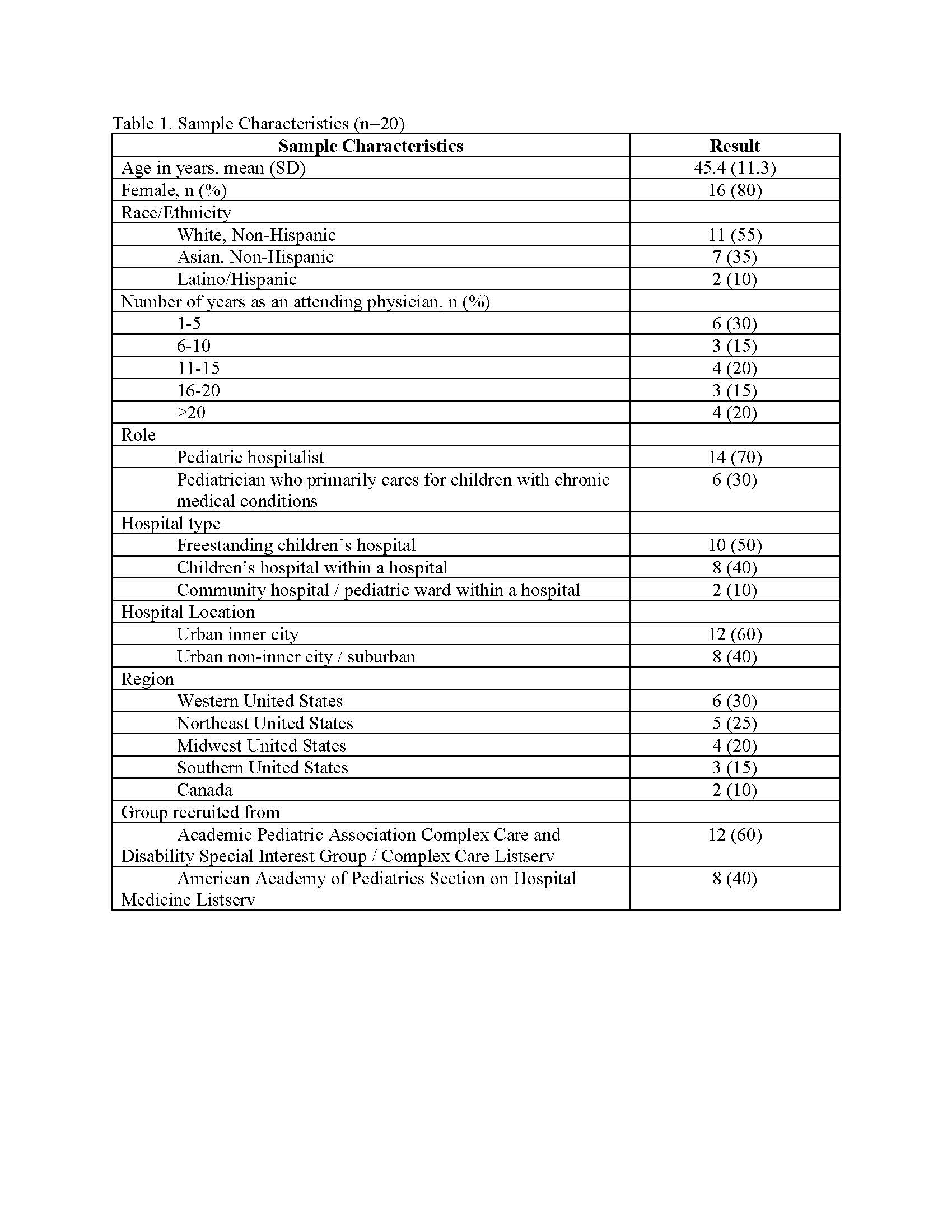
Table 2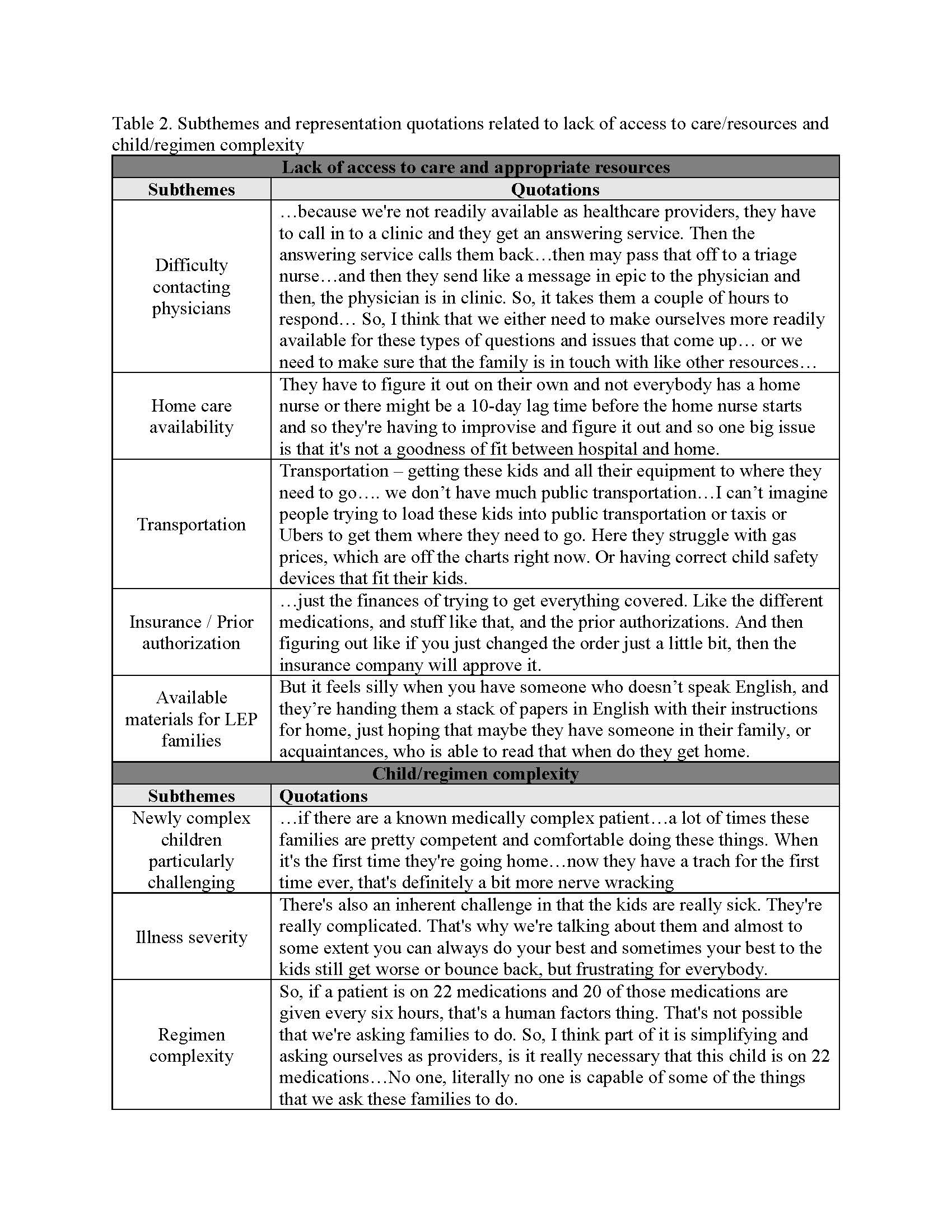
Objective: To examine pediatrician perspectives on barriers and facilitators experienced by parents in comprehension of and adherence to discharge instructions for CMC after an inpatient hospitalization.
Design/Methods: We conducted a qualitative, descriptive study of a purposeful sample of attending pediatricians (n=20) caring for CMC in inpatient settings (US and Canada) and belonging to listservs for pediatric hospitalists/complex care providers. We used maximum variation sampling to ensure heterogeneity (e.g., hospital, region). A multidisciplinary team designed and piloted a semi-structured interview guide with members of the target population. Trained team members conducted semi-structured interviews via phone or video call. Interviews were audiorecorded and transcribed. We analyzed transcripts using content analysis (Dedoose Version 9.0.17). We derived codes a priori from a conceptual framework (based on the Pediatric Self-Management Model and existing literature) and a preliminary analysis of transcripts. We applied codes and subsequently identified emerging themes from transcripts. Methodologic rigor was supported via member checking, peer debriefing, and 2 coders for a subset of transcripts.
Results: We identified 4 themes among participants (Table 1): 1) Lack of access to care and appropriate resources, including physician access, home care, transportation, insurance, and available materials for families with limited English proficiency (Table 2); 2) Challenges associated with child and regimen complexity (especially for children who are newly medically complex) (Table 2); 3) Importance of teamwork and relationship building (Table 3); and 4) Need for a patient- and family-centered and structured approach to discharge planning, including accommodating schedules/competing priorities, understanding support systems, ensuring enough time for discharge counseling and comfort with post-discharge care, and tailoring education (Table 3).Conclusion(s): Pediatricians identified several barriers and facilitators to discharge instruction comprehension and adherence for parents of CMC. Next steps include assessment of parent perspectives and development of intervention strategies.
Table 1
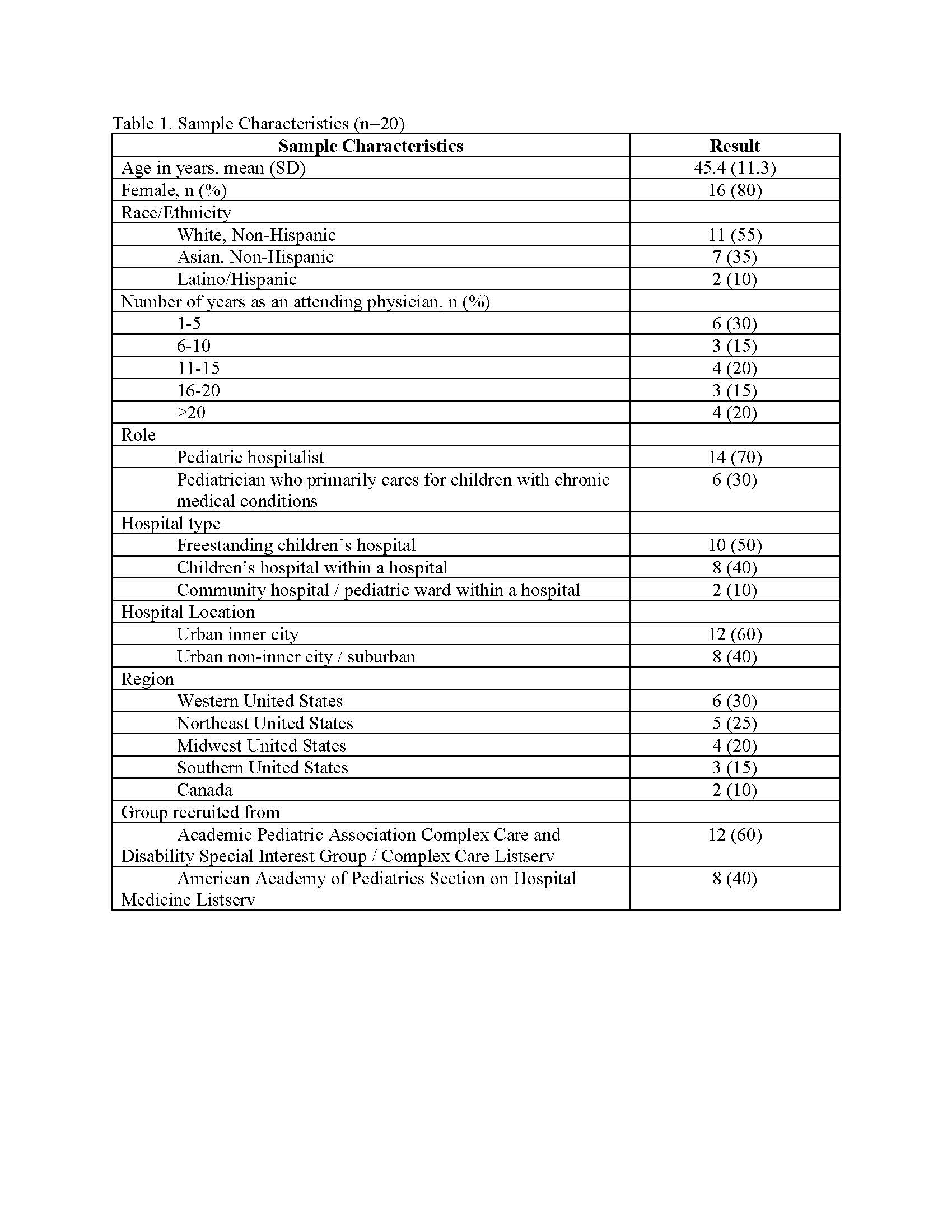
Table 2