Neonatal General
Category: Abstract Submission
Neonatology General 11: Lung
365 - Prediction of Bronchopulmonary Dysplasia (BPD) in Extremely Premature Infants on First Day of Life using the BPD Calculator
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 365
Publication Number: 365.440
Publication Number: 365.440
Sara Ali, University of Texas Medical Branch at Galveston, Galveston, TX, United States; Katelyn A. Harris Meaux, University of Texas Medical Branch School of Medicine, Galveston, TX, United States; Staley Rose, University of Texas Medical Branch School of Medicine, Galveston, TX, United States; Sunil K. Jain, University of Texas Medical Branch School of Medicine, Galveston, TX, United States

Sara Ali, MD
Resident
University of Texas Medical Branch at Galveston
Galveston, Texas, United States
Presenting Author(s)
Background:
Early risk prediction of bronchopulmonary dysplasia (BPD) in preterm infants (PI) may be helpful in implementing strategies to prevent BPD at an earlier stage. The NICHD ‘BPD Outcome Estimator’ (BPD calculator) is known to predict risk of BPD development in preterm infants using clinical and demographic data.
Objective:
To assess the accuracy of BPD calculator in predicting severity of BPD in preterm infants at day 1 of life
Design/Methods:
We defined BPD at 36 weeks post menstrual age (PMA) regardless of oxygen requirement at first 28 days. The severity was defined as: no BPD - no respiratory support; mild BPD - nasal cannula (NC) <2 L/min; moderate BPD – NC >2 L/min or noninvasive positive airway pressure and severe BPD – invasive mechanical ventilation. The NICHD BPD outcome estimator was used to retrospectively calculate BPD risk at day 1 of life by using variables like gestational age, birth weight, race and ethnicity, sex, respiratory support, and FiO2. Chi-Square test and Krus Wallis test was used for categorical and continuous variables respectively with p value < 0.05 as significant. Receiver Operating Characteristic Analysis (ROC) was used to determine sensitivity, specificity, and likelihood ratio (LR).
Results:
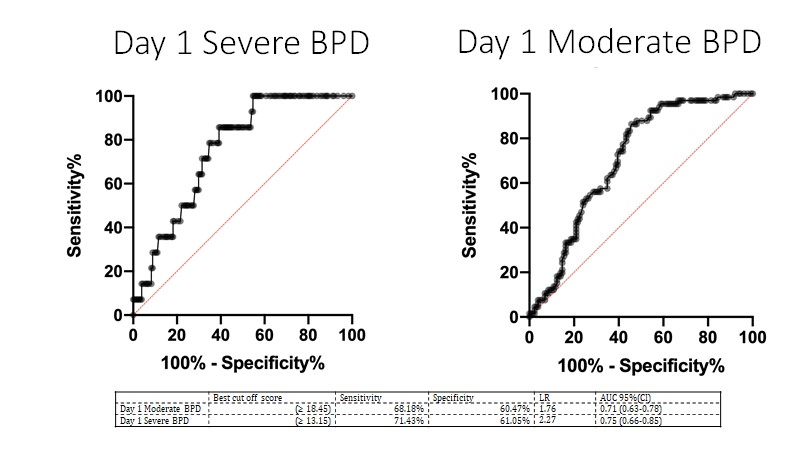
After IRB approval, in this retrospective study, we recruited 198 infants with mean birth weight 871+214 g and gestation 26.2+2 weeks (demographic details Table). 60% infants (118/198) developed BPD, out of which 18.7% had mild, 33% had moderate and 7.5% had severe BPD. Severity of BPD increased hospital stay and respiratory support. BPD calculator on day 1 had LR of 2.27, sensitivity of 71% and specificity of 61% [(AUC 0.75 (0.66 – 0.85)] for severe BPD and for moderate BPD at 36 weeks PMA LR 1.76, sensitivity 68%, and specificity 60% [AUC 0.71 (0.63 – 0.780]. BPD calculator on day 1 did not predict mild BPD at 36 weeks PMA.
Conclusion(s):
BPD calculator is a useful tool for earlier prediction of moderate to severe BPD at 36 weeks PMA in extremely preterm infants. This can be used to modify management of extremely preterm infants which may help prevent and/or reduce incidence of BPD.
Receiver Operating Characteristic Curve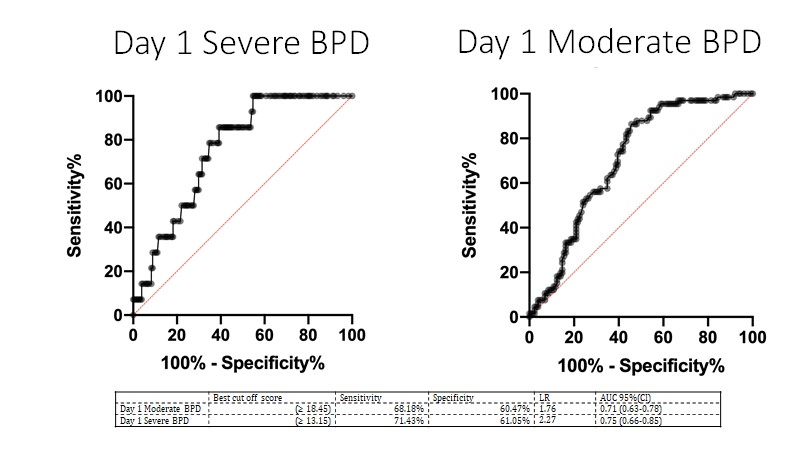
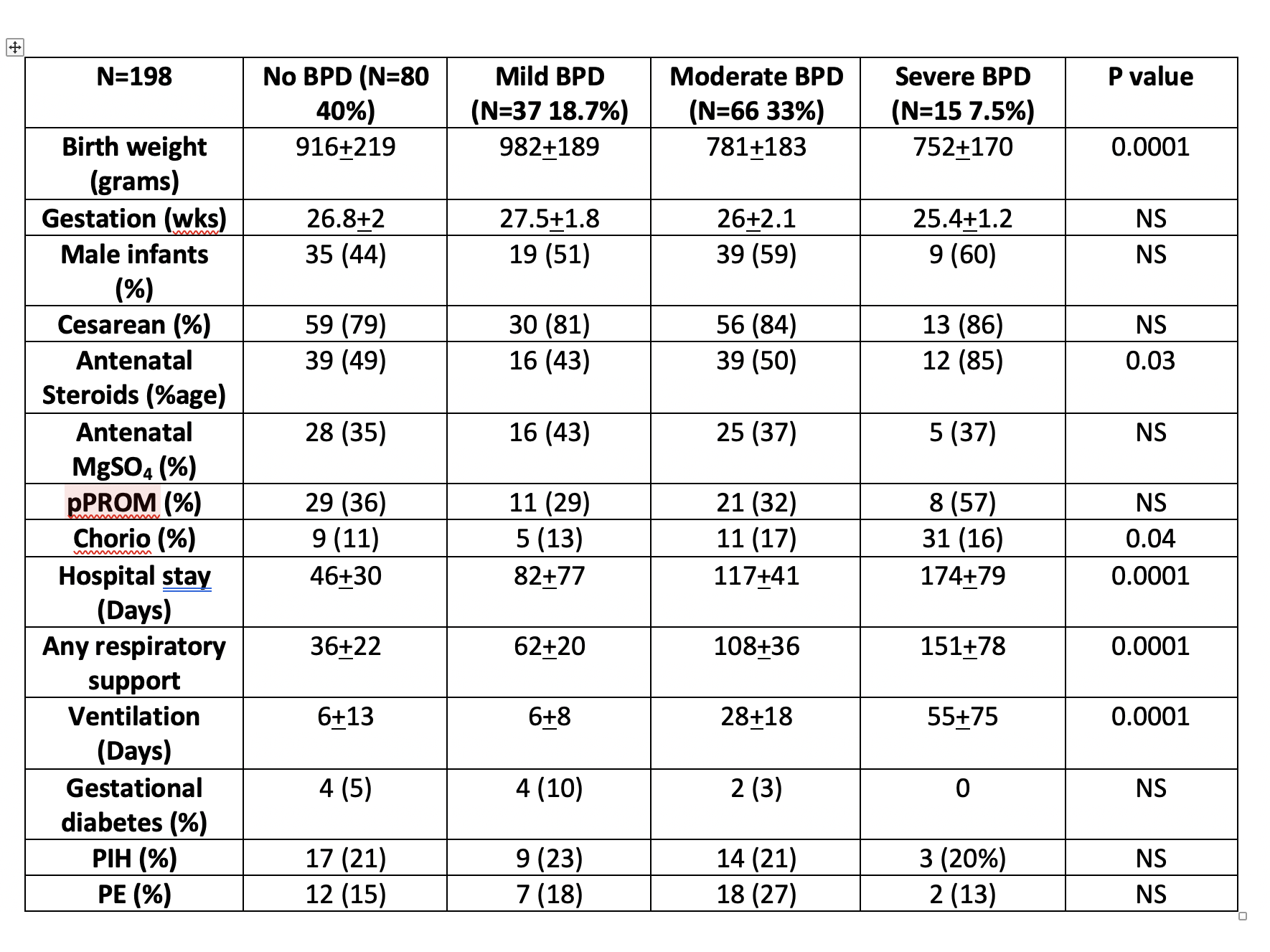
Demographic Table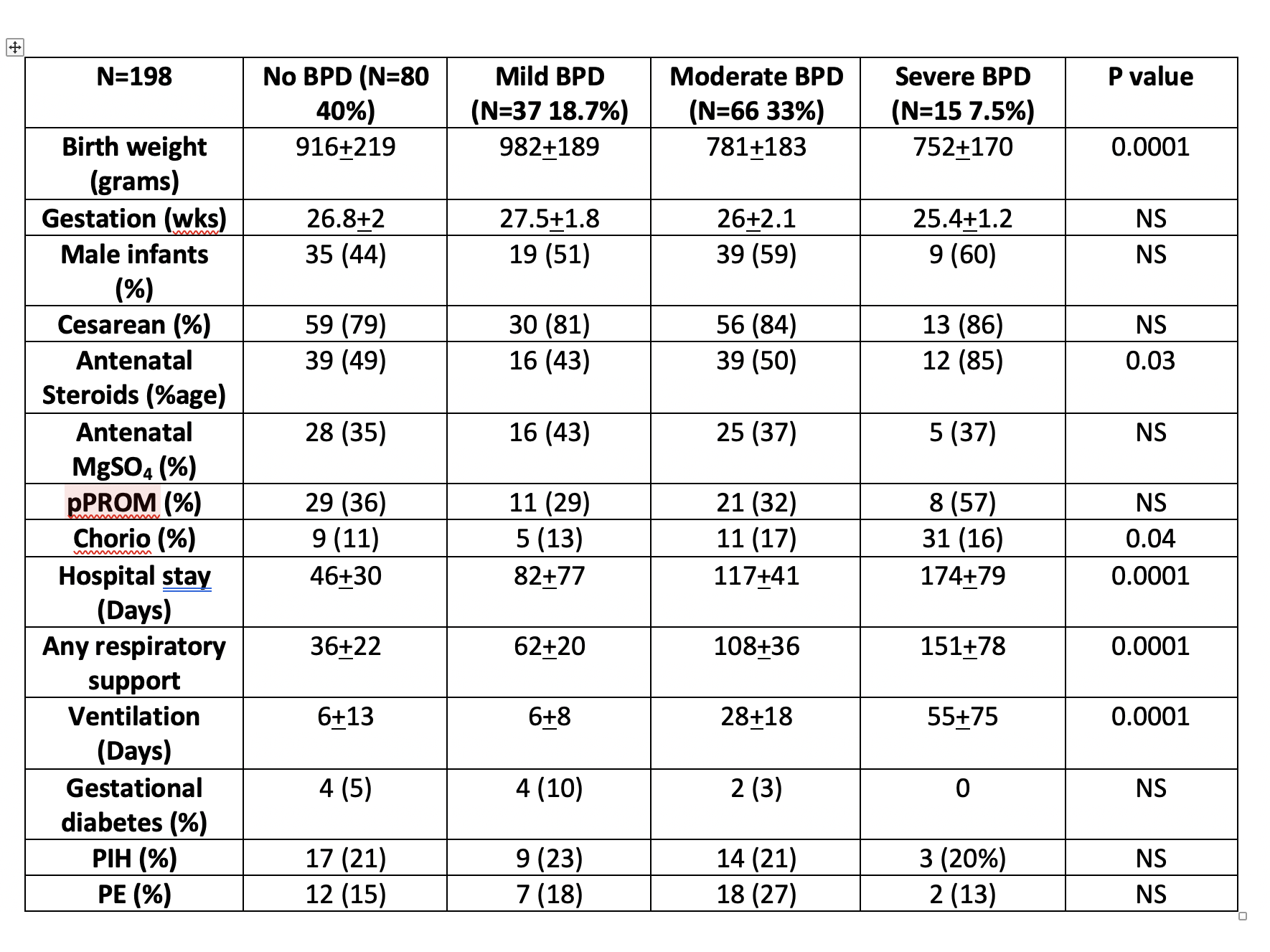
Early risk prediction of bronchopulmonary dysplasia (BPD) in preterm infants (PI) may be helpful in implementing strategies to prevent BPD at an earlier stage. The NICHD ‘BPD Outcome Estimator’ (BPD calculator) is known to predict risk of BPD development in preterm infants using clinical and demographic data.
Objective:
To assess the accuracy of BPD calculator in predicting severity of BPD in preterm infants at day 1 of life
Design/Methods:
We defined BPD at 36 weeks post menstrual age (PMA) regardless of oxygen requirement at first 28 days. The severity was defined as: no BPD - no respiratory support; mild BPD - nasal cannula (NC) <2 L/min; moderate BPD – NC >2 L/min or noninvasive positive airway pressure and severe BPD – invasive mechanical ventilation. The NICHD BPD outcome estimator was used to retrospectively calculate BPD risk at day 1 of life by using variables like gestational age, birth weight, race and ethnicity, sex, respiratory support, and FiO2. Chi-Square test and Krus Wallis test was used for categorical and continuous variables respectively with p value < 0.05 as significant. Receiver Operating Characteristic Analysis (ROC) was used to determine sensitivity, specificity, and likelihood ratio (LR).
Results:
After IRB approval, in this retrospective study, we recruited 198 infants with mean birth weight 871+214 g and gestation 26.2+2 weeks (demographic details Table). 60% infants (118/198) developed BPD, out of which 18.7% had mild, 33% had moderate and 7.5% had severe BPD. Severity of BPD increased hospital stay and respiratory support. BPD calculator on day 1 had LR of 2.27, sensitivity of 71% and specificity of 61% [(AUC 0.75 (0.66 – 0.85)] for severe BPD and for moderate BPD at 36 weeks PMA LR 1.76, sensitivity 68%, and specificity 60% [AUC 0.71 (0.63 – 0.780]. BPD calculator on day 1 did not predict mild BPD at 36 weeks PMA.
Conclusion(s):
BPD calculator is a useful tool for earlier prediction of moderate to severe BPD at 36 weeks PMA in extremely preterm infants. This can be used to modify management of extremely preterm infants which may help prevent and/or reduce incidence of BPD.
Receiver Operating Characteristic Curve
Demographic Table