General Pediatrics: Primary Care/Prevention
Category: Abstract Submission
General Pediatrics VI
119 - Preparing to launch iPOP-UP (Improving Pediatric Obesity Practice Using Prompts): a mixed methods formative evaluation
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 119
Publication Number: 119.410
Publication Number: 119.410
Mona Sharifi, Yale School of Medicine, New Haven, CT, United States; Jessica M. Ray, Yale School of Medicine, Gainesville, FL, United States; Emily B. Finn, Yale School of Medicine, New Haven, CT, United States; Hollyce Tyrrell, Academic Pediatric Association, McLean, VA, United States; Carlin Aloe, Yale University School of Medicine, New Haven, CT, United States; Kaitlin R. Maciejewski, Yale Center for Analytical Sciences, New Haven, CT, United States; Jeremy Michel, Childrens Hospital of Philadelphia, Bryn Mawr, PA, United States; Randall Grout, Indiana University School of Medicine, Indianapolis, IN, United States; Charles Wood, Duke University School of Medicine, Durham, NC, United States; Dean S. Miner, Duke University School of Medicine, Durham, NC, United States; Rixin Wang, Yale School of Medicine, New Haven, CT, United States; Denise Esserman, Yale School of Public Health, New Haven, CT, United States; Eliana M. Perrin, Johns Hopkins School of Medicine, Baltimore, MD, United States; Laura J. Damschroder, Implementation Pathways, LLC and Veterans Affairs (VA) Ann Arbor Center for ClinicaL Management Research (CCMR), Ann Arbor, MI, United States

Mona Sharifi, MD, MPH (she/her/hers)
Associate Professor of Pediatrics
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Overweight/obesity (OW/OB) prevalence is rising, and disparities are widening. Primary care clinicians (PCCs) play a key role in OW/OB care, yet evidence-based practice is inconsistent. Electronic health record (EHR)-based clinical decision support (CDS) for PCCs improved OW/OB practice and outcomes in prior trials, but implementation of CDS in new contexts can be challenging.
Objective: To assess factors that influence the implementation and effectiveness of EHR-based CDS for OW/OB across diverse primary care settings
Design/Methods: We used mixed methods to assess OW/OB management and past experiences with CDS at 84 primary care practices in 3 US health systems in the Northeast, Midwest, and South. For all 2-to-12-year-olds with BMI≥85th percentile seen in primary care 2019-2020, we queried structured EHR data to analyze patient characteristics and evidence of OW/OB-related diagnosis and counseling. We conducted semi-structured interviews with PCCs and other stakeholders (e.g., quality leaders, EHR analysts, OW/OB specialists) purposively sampled from diverse settings. We coded PCC transcripts to identify barriers and facilitators to OW/OB CDS use. For other stakeholders, we used a Strengths, Weaknesses, Opportunities, and Threats analysis. We triangulated findings and used a novel visual mapping approach to create a unified diagram of workflows.
Results: EHR data revealed variation in patient demographics and diagnosis coding of high BMI, but all PCCs in all 3 health systems coded < 1% for nutrition/activity counseling (Table 1). The 21 PCCs and 20 non-PCCs interviewed described multi-level factors influencing OW/OB management: 1) patient/family: cultural norms, family engagement; 2) clinician: self-efficacy, expectations, weight bias/stigma; 3) health system: access to specialty care/resources; 4) community: barriers to healthy living; and challenges of COVID-19 pandemic, which span these 4 levels. Some discussed negative experiences with past implementations of CDS, but reported that in-person trainings and local champions enhanced PCC buy-in. Many noted usability within workflows drives uptake of EHR tools (e.g., using growth charts to engage patients). Figure 1 displays commonalities and points of wide variation in PCC workflows. Conclusion(s): Health systems shared common barriers to OW/OB management but also described unique local challenges related to workflows, resources, and PCC attitudes, as well as opportunities for EHR support. This information will inform user-centered design for OW/OB EHR-based CDS and guide the development of tailored implementation strategies for broad adoption.
Table 1. Characteristics of children 2 to 12 years old with OW/OB seen by PCCs in 2019-2020 (inclusive) at 84 primary care practices affiliated with 3 US health systems and EHR evidence of obesity-related clinical care.jpg)
Figure 1. Diagram displaying common elements and variation in PCC workflow during well-child visits with children with OW/OB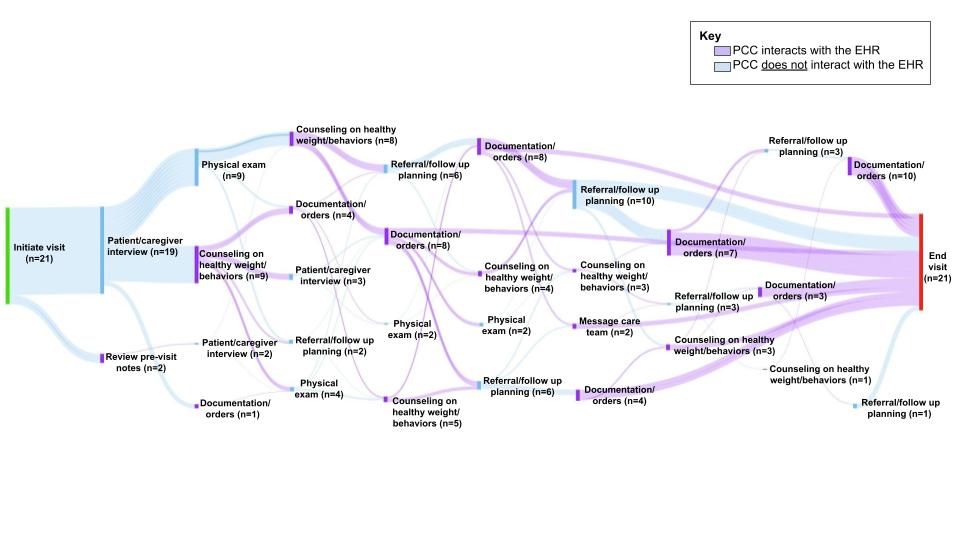 EHR: electronic health record; OW/OB: overweight/obesity; PCC: primary care clinician
EHR: electronic health record; OW/OB: overweight/obesity; PCC: primary care clinician
Objective: To assess factors that influence the implementation and effectiveness of EHR-based CDS for OW/OB across diverse primary care settings
Design/Methods: We used mixed methods to assess OW/OB management and past experiences with CDS at 84 primary care practices in 3 US health systems in the Northeast, Midwest, and South. For all 2-to-12-year-olds with BMI≥85th percentile seen in primary care 2019-2020, we queried structured EHR data to analyze patient characteristics and evidence of OW/OB-related diagnosis and counseling. We conducted semi-structured interviews with PCCs and other stakeholders (e.g., quality leaders, EHR analysts, OW/OB specialists) purposively sampled from diverse settings. We coded PCC transcripts to identify barriers and facilitators to OW/OB CDS use. For other stakeholders, we used a Strengths, Weaknesses, Opportunities, and Threats analysis. We triangulated findings and used a novel visual mapping approach to create a unified diagram of workflows.
Results: EHR data revealed variation in patient demographics and diagnosis coding of high BMI, but all PCCs in all 3 health systems coded < 1% for nutrition/activity counseling (Table 1). The 21 PCCs and 20 non-PCCs interviewed described multi-level factors influencing OW/OB management: 1) patient/family: cultural norms, family engagement; 2) clinician: self-efficacy, expectations, weight bias/stigma; 3) health system: access to specialty care/resources; 4) community: barriers to healthy living; and challenges of COVID-19 pandemic, which span these 4 levels. Some discussed negative experiences with past implementations of CDS, but reported that in-person trainings and local champions enhanced PCC buy-in. Many noted usability within workflows drives uptake of EHR tools (e.g., using growth charts to engage patients). Figure 1 displays commonalities and points of wide variation in PCC workflows. Conclusion(s): Health systems shared common barriers to OW/OB management but also described unique local challenges related to workflows, resources, and PCC attitudes, as well as opportunities for EHR support. This information will inform user-centered design for OW/OB EHR-based CDS and guide the development of tailored implementation strategies for broad adoption.
Table 1. Characteristics of children 2 to 12 years old with OW/OB seen by PCCs in 2019-2020 (inclusive) at 84 primary care practices affiliated with 3 US health systems and EHR evidence of obesity-related clinical care
.jpg)
Figure 1. Diagram displaying common elements and variation in PCC workflow during well-child visits with children with OW/OB
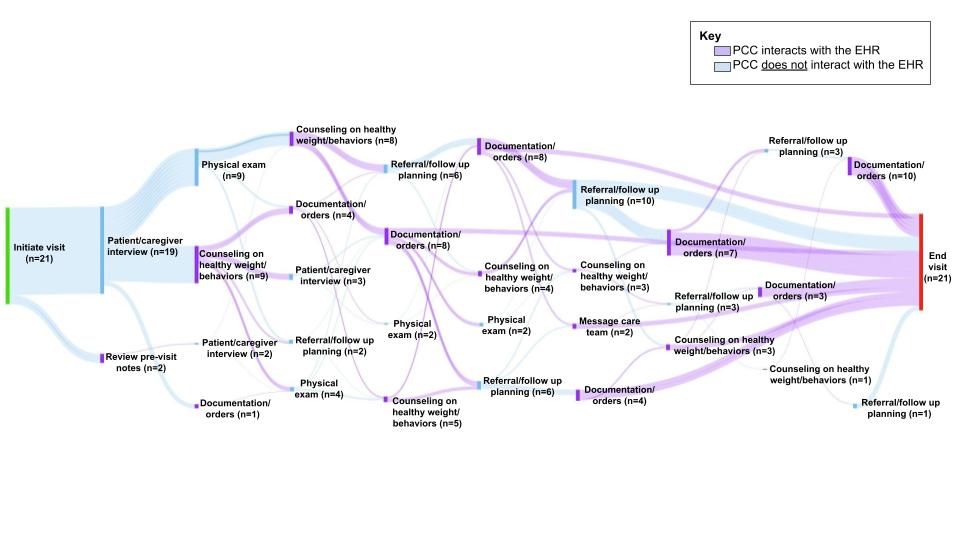 EHR: electronic health record; OW/OB: overweight/obesity; PCC: primary care clinician
EHR: electronic health record; OW/OB: overweight/obesity; PCC: primary care clinician