Neonatal Neurology: Clinical
Category: Abstract Submission
Neurology 7: Neonatal Neurology Term Imaging
353 - Risk stratification of infants with hypoxic- ischemic encephalopathy for adverse outcome based on MRI scoring
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 353
Publication Number: 353.443
Publication Number: 353.443
Enikő Szakmár, Semmelweis University, Budapest, Budapest, Hungary; Csilla Andorka, Semmelweis University, Budapest, Budapest, Hungary; Tímea Seszták, Semmelweis University, Budapest, Budapest, Hungary; Edit Varga, Semmelweis University, Budapest, Pest, Hungary; Miklós Szabó, Division of Neonatology Ist Dept. of Pediatrics Semmelweis University, Budapest, Budapest, Hungary; Agnes Jermendy, Semmelweis University, Budapest, Budapest, Hungary

Eniko Szakmar, MD, PhD
Pediatric Resident
Semmelweis University
Budapest, Hungary
Presenting Author(s)
Background: Magnetic resonance imaging (MRI) has a key role in predicting neurological outcomes in infants with hypoxic- ischemic encephalopathy (HIE). Weeke et al. developed a detailed MRI scoring system assessing brain injury in the grey matter, white matter, cortex and cerebellum resulting in a total score of 55. A cutoff value for the grey matter subscore was described to predict neurodevelopmental outcome at 2 years of age and at school age. Categorization of the total score into disease severity categories predicting neurodevelopmental outcome is still awaited.
Objective: Our aim was to stratify infants with HIE into low, moderate and high risk categories for adverse outcome (death or severe disabilities) based on the total injury score on MRI.
Design/Methods: In this single center retrospective cohort study, infants receiving hypothermia (TH) for HIE between 2013 and 2019 were enrolled. Post-rewarming brain MRI were assessed according to the Weeke scoring system. Adverse outcome was defined as death or severe disabilities if Bayley-II Scales of Infant Developmental score was < 70 in any domain at 18-24 months of age. A logistic regression model was used for the selection of optimal cut points for adverse outcome in terms of maximizing the area under the receiver operating characteristics curves (AUC). Bootstrap bias correction was carried out to calculate the corrected AUC to avoid the overestimation of obtained AUC in the logistic model.
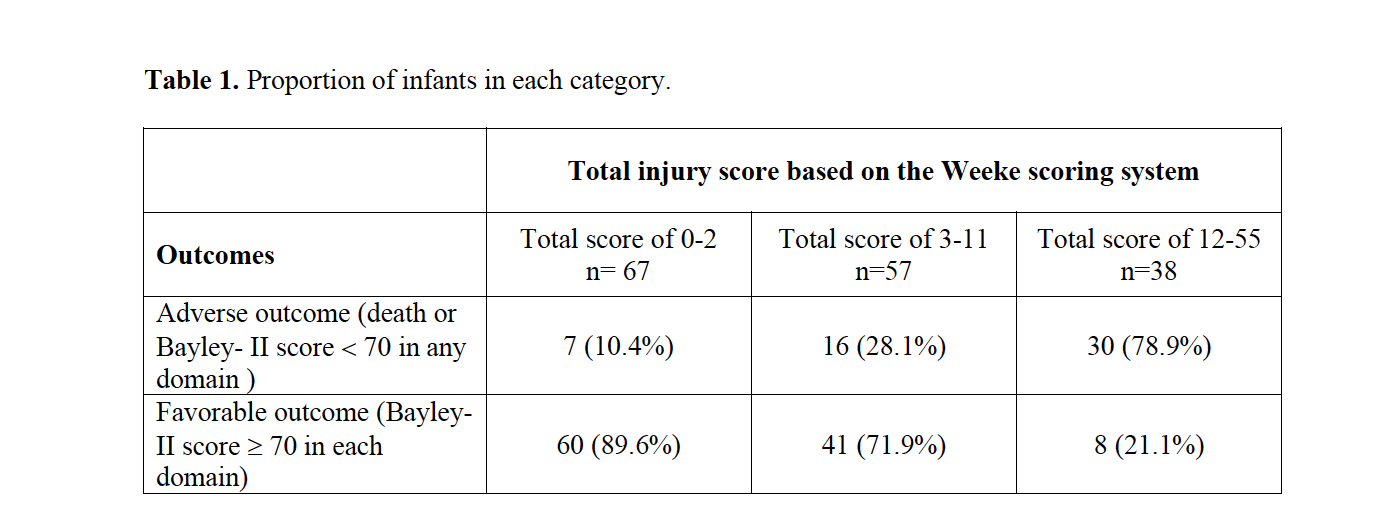
Results: A total of 162 infants who underwent TH for moderate or severe HIE were included in the present analysis. MRI studies were carried out at a median 4.7 days of life [IQR 3.5; 6.2]. The rate of death was 5.6% and severe disabilities occurred in 27.3% (44/162) of the cases. Based on the logistic regression model the optimal cut points were 0-2; 3-11 and 12-55 with a corrected AUC of 0.77. Infants who had a total score between 3 and 11 on MRI had 3- fold (95% CI 1.3- 9.4) increase in the odds of death or severe disabilities compared to the group with total score of 0-2. The infants with a total score of 12 or above had an odds ratio of 32 (95% CI 11.3-105.0) for adverse outcome. Table 1. presents the proportion of infants in each category.Conclusion(s): The presented cut points can be useful in daily clinical practice for risk stratifying patients with HIE and allow parents and caregivers to optimize care beyond the neonatal period. Since MRI scores are often used as a surrogate markers of neurodevelopmental outcome, established risk categories may also aid future clinical research efforts.
Table 1. Proportion of infants in each category.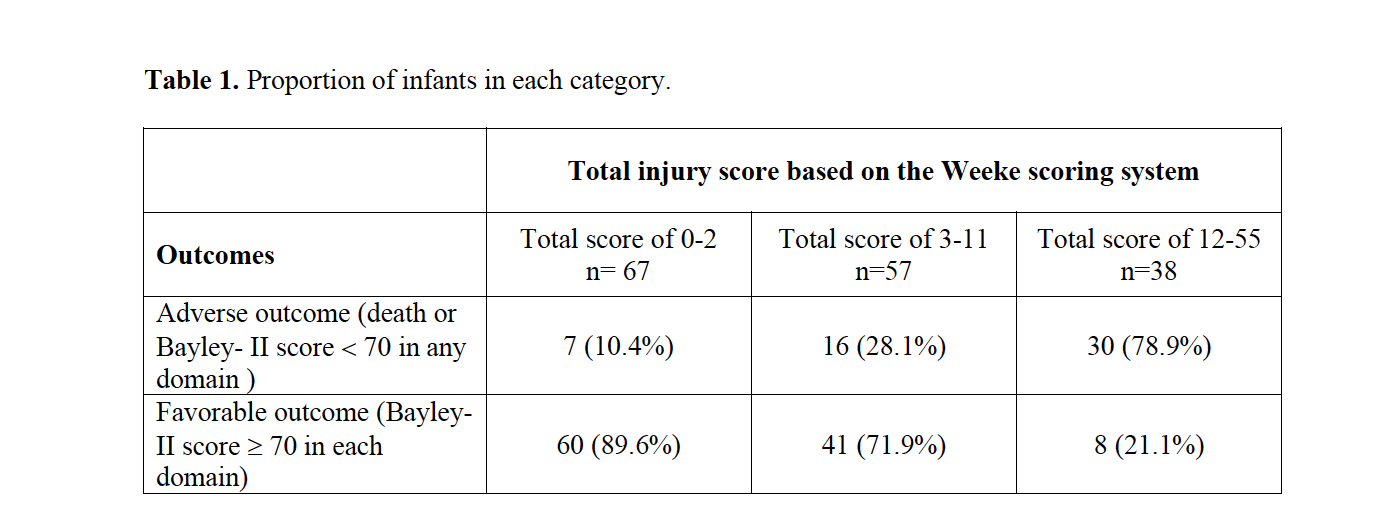
Objective: Our aim was to stratify infants with HIE into low, moderate and high risk categories for adverse outcome (death or severe disabilities) based on the total injury score on MRI.
Design/Methods: In this single center retrospective cohort study, infants receiving hypothermia (TH) for HIE between 2013 and 2019 were enrolled. Post-rewarming brain MRI were assessed according to the Weeke scoring system. Adverse outcome was defined as death or severe disabilities if Bayley-II Scales of Infant Developmental score was < 70 in any domain at 18-24 months of age. A logistic regression model was used for the selection of optimal cut points for adverse outcome in terms of maximizing the area under the receiver operating characteristics curves (AUC). Bootstrap bias correction was carried out to calculate the corrected AUC to avoid the overestimation of obtained AUC in the logistic model.
Results: A total of 162 infants who underwent TH for moderate or severe HIE were included in the present analysis. MRI studies were carried out at a median 4.7 days of life [IQR 3.5; 6.2]. The rate of death was 5.6% and severe disabilities occurred in 27.3% (44/162) of the cases. Based on the logistic regression model the optimal cut points were 0-2; 3-11 and 12-55 with a corrected AUC of 0.77. Infants who had a total score between 3 and 11 on MRI had 3- fold (95% CI 1.3- 9.4) increase in the odds of death or severe disabilities compared to the group with total score of 0-2. The infants with a total score of 12 or above had an odds ratio of 32 (95% CI 11.3-105.0) for adverse outcome. Table 1. presents the proportion of infants in each category.Conclusion(s): The presented cut points can be useful in daily clinical practice for risk stratifying patients with HIE and allow parents and caregivers to optimize care beyond the neonatal period. Since MRI scores are often used as a surrogate markers of neurodevelopmental outcome, established risk categories may also aid future clinical research efforts.
Table 1. Proportion of infants in each category.