Mental Health
Category: Abstract Submission
Mental Health II
533 - Attitudes Towards Postpartum Depression Screening in Pediatric Continuity Practices
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 533
Publication Number: 533.423
Publication Number: 533.423
Pooja Gajulapalli, Eastern Virginia Medical School, Burke, VA, United States; Natasha K. Sriraman, Children's Hospital of The King's Daughters, Norfolk, VA, United States; John W. Harrington, Children's Hospital of The King's Daughters, Norfolk, VA, United States; Hollyce Tyrrell, Academic Pediatric Association, McLean, VA, United States

Pooja Gajulapalli, B.S.
Medical Student
Eastern Virginia Medical School
Burke, Virginia, United States
Presenting Author(s)
Background: Postpartum mood disorders (PPMD) are the manifestation of depressive or anxiety symptoms within the first year of childbirth. Mothers that develop PPMD frequently have difficulty with maternal-infant bonding, leading to negative effects in both mother and baby. The American Academy of Pediatrics (AAP) recommends that pediatricians screen mothers for PPMD before or during the 1-month well-child checks (WCC), and the 2, 4, and 6-month WCC with a validated screening tool such as the Edinburgh Perinatal Depression Screening (EPDS) or the Patient Health Questionnaire (PHQ).
Objective: The purpose of this project was to identify variations in PPMD screening and intervention practices amongst academic general pediatric clinics of the Academic Pediatric Association’s (APA) Continuity Research Network (CORNET), as well as highlight barriers to screening.
Design/Methods: A recruitment email was sent to 118 pediatric residency programs enrolled in CORNET. Continuity clinics interested in joining were then sent an enrollment survey to provide demographic information and a REDCap link to complete the study survey.
Results: Preliminary data includes completed surveys from 31 clinics. The majority of responding clinics serve urban or suburban areas (97%) with majority non-white populations (87%). Many clinics see patients with Medicaid (90%) or no insurance (45%).
28 clinics report screening for PPMD. All clinics screened with the PHQ and EPDS; however, 5 clinics solely screened with shortened versions of the PHQ (PHQ-2) and the EPDS (EPDS-7). “Positive screening”, or screening results that trigger concern or action, varied for each screening tool, with wide “positive score” ranges amongst all tools. Suicidality did not trigger concern or action in 2 clinics using the EPDS. Only 55% (17/31) of clinics screen at all AAP-recommended time points.
The most common interventions amongst screening clinics were consulting in-office social work, providing pamphlets on PPMD, and referral to the mother’s OB/GYN. Reported barriers to screening include lack of embedded social work, awareness of resources, education, training of staff, as well as time constraints.Conclusion(s): These results suggest considerable variation in screening practices amongst the clinics surveyed. Over half of clinics do not follow AAP guidelines of screening at all well-child checks after the 1-month mark. This data implies that although there are clear recommendations for pediatricians to screen for PPMD, more assistance and training is required for effective PPMD screening.
APA Student Research Award CV UploadPooja's CV.pdf
Types of Interventions Utilized for Positive PPMD Screening.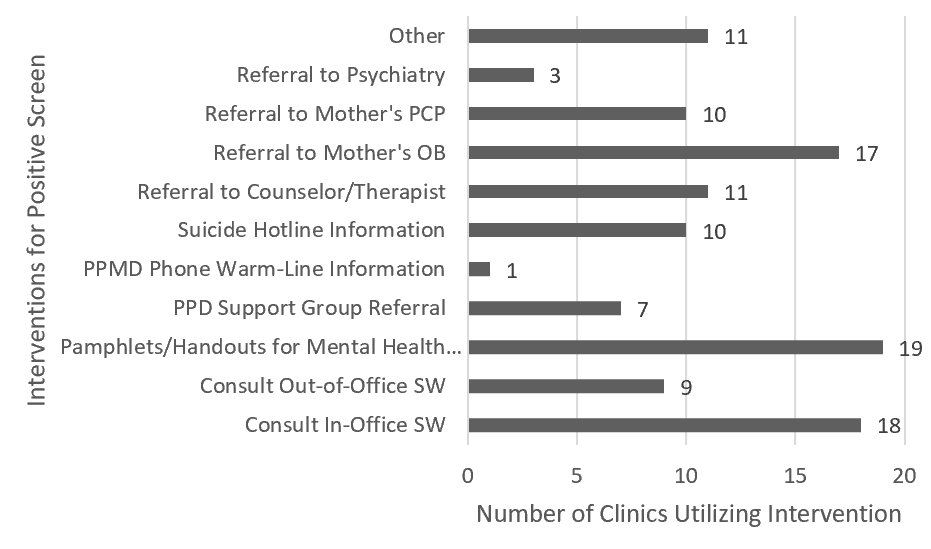 Clinics reported using a variety of methods when a mother screens positively on a PPMD screening tool.
Clinics reported using a variety of methods when a mother screens positively on a PPMD screening tool.
Objective: The purpose of this project was to identify variations in PPMD screening and intervention practices amongst academic general pediatric clinics of the Academic Pediatric Association’s (APA) Continuity Research Network (CORNET), as well as highlight barriers to screening.
Design/Methods: A recruitment email was sent to 118 pediatric residency programs enrolled in CORNET. Continuity clinics interested in joining were then sent an enrollment survey to provide demographic information and a REDCap link to complete the study survey.
Results: Preliminary data includes completed surveys from 31 clinics. The majority of responding clinics serve urban or suburban areas (97%) with majority non-white populations (87%). Many clinics see patients with Medicaid (90%) or no insurance (45%).
28 clinics report screening for PPMD. All clinics screened with the PHQ and EPDS; however, 5 clinics solely screened with shortened versions of the PHQ (PHQ-2) and the EPDS (EPDS-7). “Positive screening”, or screening results that trigger concern or action, varied for each screening tool, with wide “positive score” ranges amongst all tools. Suicidality did not trigger concern or action in 2 clinics using the EPDS. Only 55% (17/31) of clinics screen at all AAP-recommended time points.
The most common interventions amongst screening clinics were consulting in-office social work, providing pamphlets on PPMD, and referral to the mother’s OB/GYN. Reported barriers to screening include lack of embedded social work, awareness of resources, education, training of staff, as well as time constraints.Conclusion(s): These results suggest considerable variation in screening practices amongst the clinics surveyed. Over half of clinics do not follow AAP guidelines of screening at all well-child checks after the 1-month mark. This data implies that although there are clear recommendations for pediatricians to screen for PPMD, more assistance and training is required for effective PPMD screening.
APA Student Research Award CV UploadPooja's CV.pdf
Types of Interventions Utilized for Positive PPMD Screening.
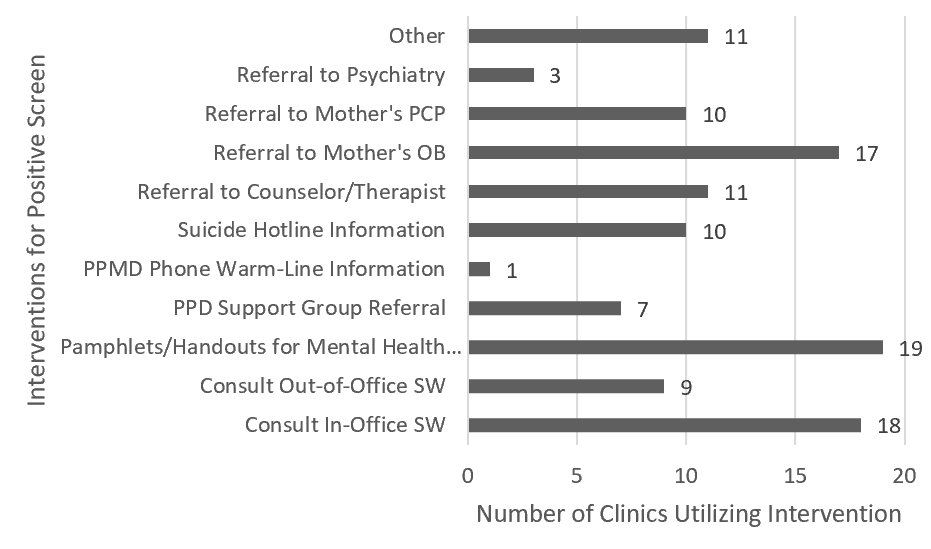 Clinics reported using a variety of methods when a mother screens positively on a PPMD screening tool.
Clinics reported using a variety of methods when a mother screens positively on a PPMD screening tool.