Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: Sepsis
562 - Causative Pathogens and Outcomes of Neonates with Sepsis Requiring ECMO at Quaternary NICUs
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 562
Publication Number: 562.427
Publication Number: 562.427
Zeenia Billimoria, University of Washington School of Medicine, Seattle, WA, United States; Rakesh Rao, Washington University in St. Louis School of Medicine, Saint Louis, MO, United States; Burhan Mahmood, UPMC Childrens Hospital of Pittsburgh, Pittburgh, PA, United States; Isabella Zaniletti, Children's Hospitals Association, Lenexa, KS, United States; Natalie Rintoul, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Rachel Chapman, Children's Hospital Los Angeles, Los Angeles, CA, United States; Ruth B. Seabrook, Nationwide Children'S Hospital (Columbus, OH), Columbus, OH, United States; Shannon E. Hamrick, Emory University School of Medicine, Children's Healthcare of Atlanta, Atlanta, GA, United States; Sarah D. Keene, choa/emory, DECATUR, GA, United States; Sharada H. Gowda, Baylor College of Medicine, Houston, TX, United States; Nicholas R. Carr, University of Utah School of Medicine, Sandy, UT, United States; Kevin M. Sullivan, Sidney Kimmel Medical College at Thomas Jefferson University, Wilmington, DE, United States; Robert DiGeronimo, Seattle Children's Hospital, Seattle, WA, United States
- SG
Sharada H. Gowda, MD
Assistant Professor of Pediatrics
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Sepsis remains a leading cause of neonatal morbidity and mortality. Ten percent of neonates with respiratory failure supported with extracorporeal membrane oxygenation (ECMO) had sepsis in the 2017 ELSO registry. Data is lacking on causative pathogens and outcomes in this population.
Objective: To describe the causative pathogens and outcomes of neonates with sepsis requiring ECMO.
Design/Methods: We conducted a retrospective review of the Children’s Hospital Neonatal Consortium database. All neonates supported with ECMO were identified. We created 3 groups: culture positive sepsis (CPS) (positive blood, tracheal, cerebrospinal fluid and/or urine culture), clinical sepsis (CS) (culture negative and treated with antibiotics for at least 7 days), and neonates treated with ECMO for other indications. All congenital diaphragmatic hernia patients were excluded from the cohort. Categorical variables were summarized with counts and percentages, while medians and interquartile ranges were used for continuous variables. Groups were compared using Chi-square, Fisher’s exact and Kruskal-Wallis as appropriate. All analyses were conducted in SAS Enterprise Guide v7.1 and significance was evaluated at a level of 0.05.
Results: From 2010-2016, we identified 818 neonates supported with ECMO, 108 with CPS, 176 with CS, and 534 for other non-sepsis etiologies. Most common pathogens were Escherichia coli (E. coli) (n=21; 19.4%), Group B Streptococcus (GBS) (n=20; 18.5%) and Herpes simplex virus (HSV) (n=8; 7.4%). Neonates with CPS were more likely to be supported with veno-arterial ECMO (69.4%) versus CS (44.3%). Age at ECMO cannulation was 5 versus 1 day and mean length of ECMO run was 7 versus 5 days in neonates with CPS compared to CS. Mortality in neonates supported with ECMO for CPS was 50% versus 18.8% in neonates with CS. In addition, neonates with CPS required longer ECMO runs and had a longer hospital length of stay in survivors. Neurologic injury overall was relatively low, but CPS was associated with a higher rate of intraventricular hemorrhage with acute ventriculomegaly and cerebellar hemorrhage. Forty one percent of CPS neonates that survived post ECMO were discharged home with 34% needing tube assisted feeding.
Conclusion(s): Many outcomes including survival in neonates with CPS following ECMO are worse compared with other clinical subgroups. GBS, E. coli and HSV were commonly identified pathogens. Neonates that survive to discharge home uncommonly require respiratory support other than oxygen but are at increased risk of needing gavage assisted feeding.
Table 1. Baseline patient and ECMO characteristics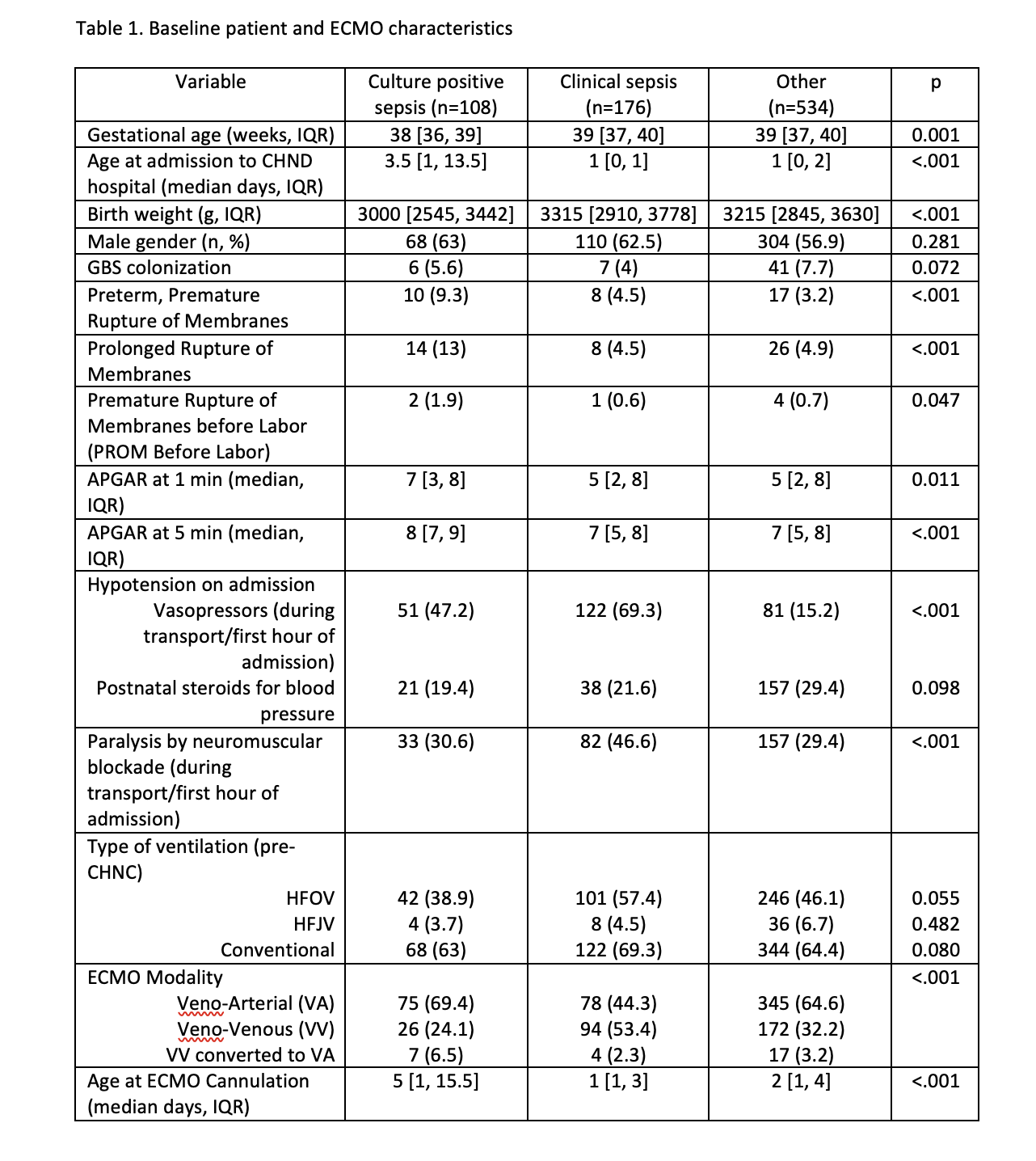
Table 2. Patient Outcomes.png)
Objective: To describe the causative pathogens and outcomes of neonates with sepsis requiring ECMO.
Design/Methods: We conducted a retrospective review of the Children’s Hospital Neonatal Consortium database. All neonates supported with ECMO were identified. We created 3 groups: culture positive sepsis (CPS) (positive blood, tracheal, cerebrospinal fluid and/or urine culture), clinical sepsis (CS) (culture negative and treated with antibiotics for at least 7 days), and neonates treated with ECMO for other indications. All congenital diaphragmatic hernia patients were excluded from the cohort. Categorical variables were summarized with counts and percentages, while medians and interquartile ranges were used for continuous variables. Groups were compared using Chi-square, Fisher’s exact and Kruskal-Wallis as appropriate. All analyses were conducted in SAS Enterprise Guide v7.1 and significance was evaluated at a level of 0.05.
Results: From 2010-2016, we identified 818 neonates supported with ECMO, 108 with CPS, 176 with CS, and 534 for other non-sepsis etiologies. Most common pathogens were Escherichia coli (E. coli) (n=21; 19.4%), Group B Streptococcus (GBS) (n=20; 18.5%) and Herpes simplex virus (HSV) (n=8; 7.4%). Neonates with CPS were more likely to be supported with veno-arterial ECMO (69.4%) versus CS (44.3%). Age at ECMO cannulation was 5 versus 1 day and mean length of ECMO run was 7 versus 5 days in neonates with CPS compared to CS. Mortality in neonates supported with ECMO for CPS was 50% versus 18.8% in neonates with CS. In addition, neonates with CPS required longer ECMO runs and had a longer hospital length of stay in survivors. Neurologic injury overall was relatively low, but CPS was associated with a higher rate of intraventricular hemorrhage with acute ventriculomegaly and cerebellar hemorrhage. Forty one percent of CPS neonates that survived post ECMO were discharged home with 34% needing tube assisted feeding.
Conclusion(s): Many outcomes including survival in neonates with CPS following ECMO are worse compared with other clinical subgroups. GBS, E. coli and HSV were commonly identified pathogens. Neonates that survive to discharge home uncommonly require respiratory support other than oxygen but are at increased risk of needing gavage assisted feeding.
Table 1. Baseline patient and ECMO characteristics
Table 2. Patient Outcomes
.png)
