Cardiology
Category: Abstract Submission
Cardiology II
97 - Short and Long Term Outcomes in Infants with Supraventricular Tachycardia: Readmissions and Recurrence
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 97
Publication Number: 97.303
Publication Number: 97.303
Daniel Vari, Cincinnati Childrens Hospital, Newport, KY, United States; Nicholas Kurek, University of Cincinnati College of Medicine, Cincinnati, OH, United States; Jeff Anderson, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; David S. Spar, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Richard J. Czosek, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Daniel Vari, MD
Cardiology Fellow
Cincinnati Childrens Hospital
Newport, Kentucky, United States
Presenting Author(s)
Background: Supraventricular tachycardia (SVT) is the most common rhythm disorder in infants. At diagnosis, patients are often admitted for anti-arrhythmic therapy and discharged after a period of observation. Medications are often stopped between 6-12 months of age if no recurrence is noted. There are limited data on risk factors for readmission, readmission rates and recurrence after medication cessation.
Objective: We sought to investigate risk factors for and incidence of readmission in infants diagnosed with SVT. The secondary goal was to evaluate recurrence rates outside infancy.
Design/Methods: We performed a single-center retrospective study over a 10 year period of infants under 6 months of age with documented SVT. SVT was defined as typical atrioventricular reentrant tachycardia (AVRT), atrioventricular nodal reentrant tachycardia (AVNRT), permanent junctional reciprocating tachycardia (PJRT) and atrial tachycardia (AT). Infants with congenital heart disease requiring surgical or catheter intervention and those with gestational age less than 34 weeks were excluded. The primary outcome was readmission within 31 days of hospital discharge. Recurrence rates after medication cessation were also examined. Categorical variables were represented as frequency (percentage) and continuous variables as median (interquartile range).
Results: A total of 90 patients were included. Of these, 75 (83%) had AVRT or AVNRT, 5 (6%) had PJRT and 10 (11%) had AT. Fourteen (16%) were diagnosed prenatally, otherwise median age of diagnosis was 11 days (3.0, 30.8). Beta blockers were the initial therapy in 66 (73%) and 28 (31%) required a medication change prior to discharge. On admission, 8 patients were started on continuous intravenous anti-arrhythmic while 4 others were initiated after admission. Median length of admission was 83.4 (46.3, 161.2) hours. Nineteen (21%) were readmitted within 31 days of discharge. The only clinical factor associated with readmission was continuous anti-arrhythmic infusion initiated after admission (3/19 vs. 1/71, p = 0.037). Median length of follow up was 942 (501, 1728) days. Patients who were readmitted within 31 days had a longer length of treatment (12 [11.5, 22.0] vs. 10 [7.5, 12.0] months, p = 0.007) and were more likely to undergo ablation (4/19 vs. 2/71, p = 0.017).Conclusion(s): In this cohort of infants with SVT readmission was common and only continuous anti-arrhythmic infusion started after admission was associated with readmission. Infants who were readmitted within 31 days of discharge had longer length of anti-arrhythmic therapy and were more likely to undergo ablation.
Kaplan-Meier Curve of Freedom from Readmission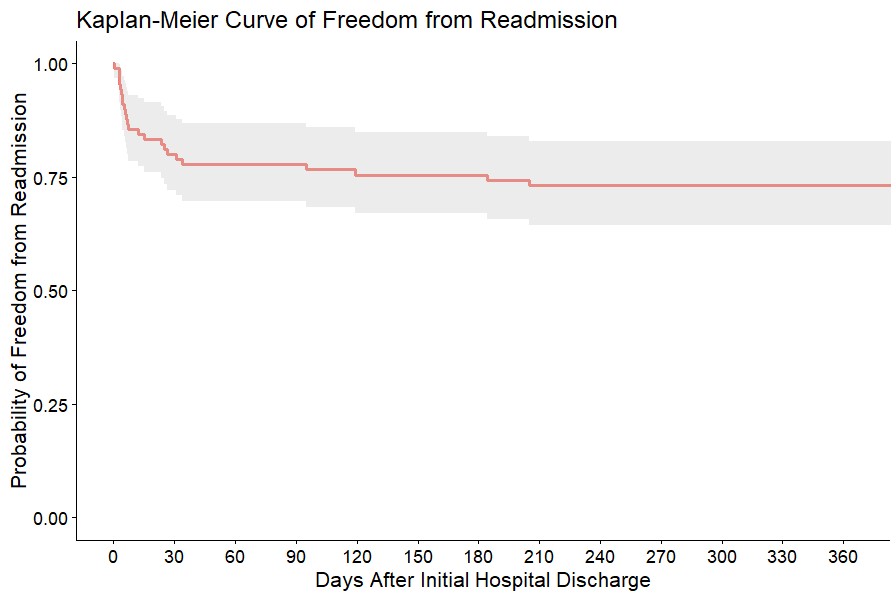
Kaplan-Meier Curve of Freedom from Ablation.png)
Objective: We sought to investigate risk factors for and incidence of readmission in infants diagnosed with SVT. The secondary goal was to evaluate recurrence rates outside infancy.
Design/Methods: We performed a single-center retrospective study over a 10 year period of infants under 6 months of age with documented SVT. SVT was defined as typical atrioventricular reentrant tachycardia (AVRT), atrioventricular nodal reentrant tachycardia (AVNRT), permanent junctional reciprocating tachycardia (PJRT) and atrial tachycardia (AT). Infants with congenital heart disease requiring surgical or catheter intervention and those with gestational age less than 34 weeks were excluded. The primary outcome was readmission within 31 days of hospital discharge. Recurrence rates after medication cessation were also examined. Categorical variables were represented as frequency (percentage) and continuous variables as median (interquartile range).
Results: A total of 90 patients were included. Of these, 75 (83%) had AVRT or AVNRT, 5 (6%) had PJRT and 10 (11%) had AT. Fourteen (16%) were diagnosed prenatally, otherwise median age of diagnosis was 11 days (3.0, 30.8). Beta blockers were the initial therapy in 66 (73%) and 28 (31%) required a medication change prior to discharge. On admission, 8 patients were started on continuous intravenous anti-arrhythmic while 4 others were initiated after admission. Median length of admission was 83.4 (46.3, 161.2) hours. Nineteen (21%) were readmitted within 31 days of discharge. The only clinical factor associated with readmission was continuous anti-arrhythmic infusion initiated after admission (3/19 vs. 1/71, p = 0.037). Median length of follow up was 942 (501, 1728) days. Patients who were readmitted within 31 days had a longer length of treatment (12 [11.5, 22.0] vs. 10 [7.5, 12.0] months, p = 0.007) and were more likely to undergo ablation (4/19 vs. 2/71, p = 0.017).Conclusion(s): In this cohort of infants with SVT readmission was common and only continuous anti-arrhythmic infusion started after admission was associated with readmission. Infants who were readmitted within 31 days of discharge had longer length of anti-arrhythmic therapy and were more likely to undergo ablation.
Kaplan-Meier Curve of Freedom from Readmission
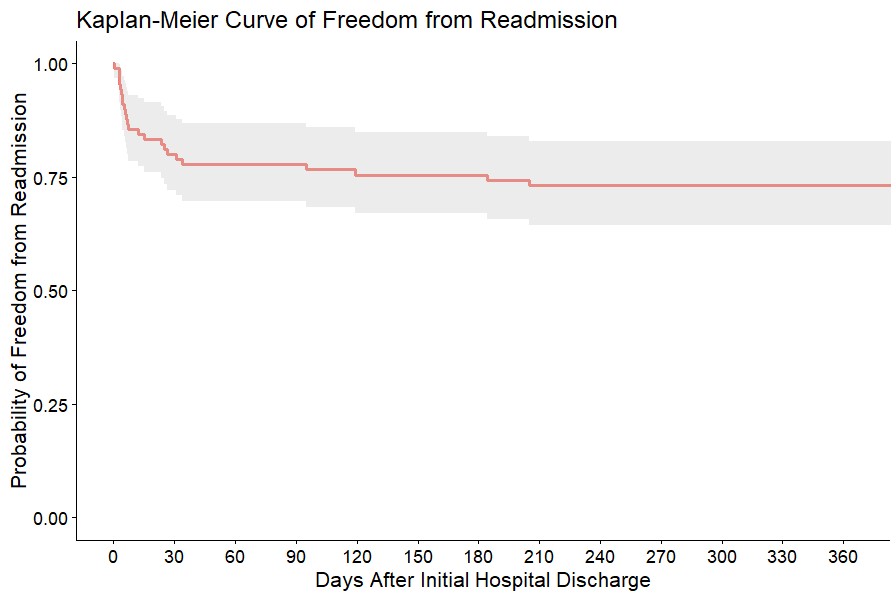
Kaplan-Meier Curve of Freedom from Ablation
.png)
