Neonatal Neurology: Clinical
Category: Abstract Submission
Neurology 4: Neonatal Neurology Preterm Clinical
470 - Single-room vs. Open-Bay NICU Design, Cerebral Maturation and Sleep-wake Cycling in Preterm Infants
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 470
Publication Number: 470.342
Publication Number: 470.342
Debashish Chowdhury, Mount Sinai Hospital, Scarborough, ON, Canada; Amish Jain, University of Toronto/ Mount Sinai Hospital, Toronto, ON, Canada; Adel Mohamed, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Prakesh Shah, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Poorva Deshpande, Mount Sinai Hospital, Mississauga, ON, Canada

Poorva Deshpande, MBBS, MRCPCP, MSc (she/her/hers)
Neonatologist
Mount Sinai Hospital
Toronto, Ontario, Canada
Presenting Author(s)
Background: Increasingly, neonatal intensive care units (NICU) are changing from a traditional open-bay (OB) to single-room (SR) design layout; however, its impact on the neurobehavioral development of preterm neonates is unclear. Amplitude-integrated electroencephalography (aEEG) is a simple bedside tool that may be used to study functional cerebral maturation and sleep-wake cycling (SWC).
Objective: To compare cerebral maturation and SWC on aEEG in extremely preterm neonates cared for in a tertiary NICU before and after layout change from OB to SR design.
Design/Methods: Mount Sinai Hospital in Toronto moved from an OB to SR NICU design in February 2015. Neonates born between gestational age (GA) 24+0 – 28+6 weeks and admitted to our NICU before (OB period) and after (SR period) design change were prospectively recruited and had single-channel aEEG recording between corrected GA 30+0 - 30+6 weeks, continuously for a period of 24 hours. Infants with intraventricular hemorrhage Grade 3, those receiving mechanical ventilation or treatment for sepsis at corrected GA 30 weeks were excluded. Recorded aEEG traces were divided into 6-hour segments and analyzed offline using visual inspection in random order. Lower (LMV) and upper (UMV) margin voltages were identified and background pattern was classified as continuous (C, LMV >5mV), discontinuous (DC, LMV 2-5mV and variable) or burst suppression (BS, LMV 0-3mV and non-variable). Uninterrupted SWCs were identified as periods of gradual fall and rise of LMV lasting ≥20 minutes (Figure 1). The primary outcome was aEEG maturation assessed using the Burdjalov score, which incorporates sub-scores for continuity, SWC, LMV, and bandwidth. Sub-score components, SWC number, and characteristics were secondary outcomes.
Results: Eighteen and 19 infants were included during OB and SR periods, respectively, with similar demographics (Table 1); C-sections were more frequent in the OB group. aEEG pattern was C or DC for all segments, except 2 infants who demonstrated a short segment ( < 1 hour) of BS pattern (1 each during OB and SR period). No differences were observed in any maturation-related aEEG variables, except the SR group showing higher total and uninterrupted SWCs per hour of recording (Table 2). Conclusion(s): SR NICU design may be associated with a higher number of total and uninterrupted SWCs in extremely preterm neonates. Further studies should focus on the relationship between higher sleep during the NICU period and neurodevelopmental outcomes.
Table 1. Baseline Characteristics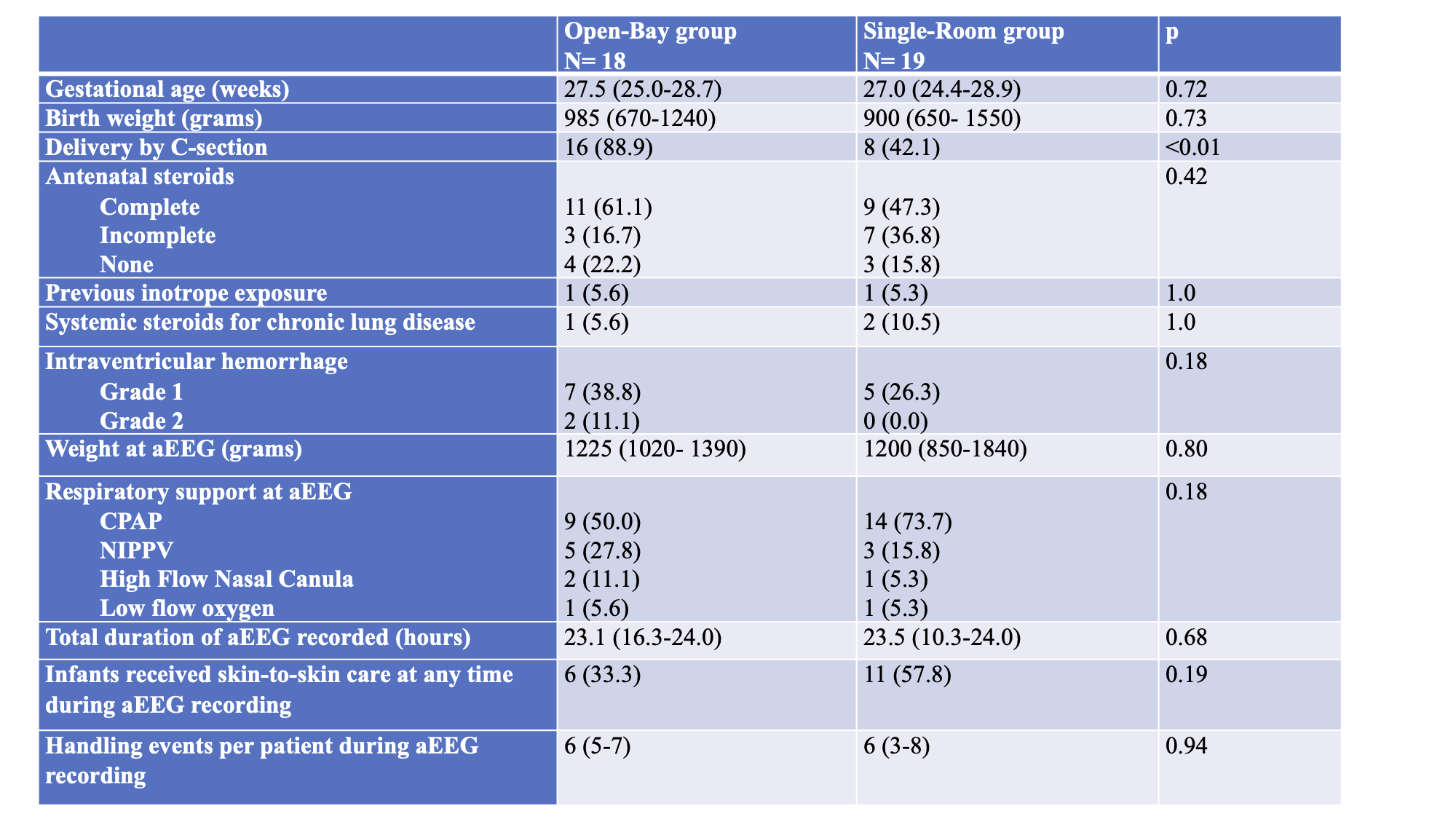 Data are presented as N (proportion) or median (range) as appropriate.
Data are presented as N (proportion) or median (range) as appropriate.
CPAP: Continuous Positive Airway Pressure, NIPPV: Non-invasive Positive Pressure Ventilation
Table 2: Differences in aEEG characteristics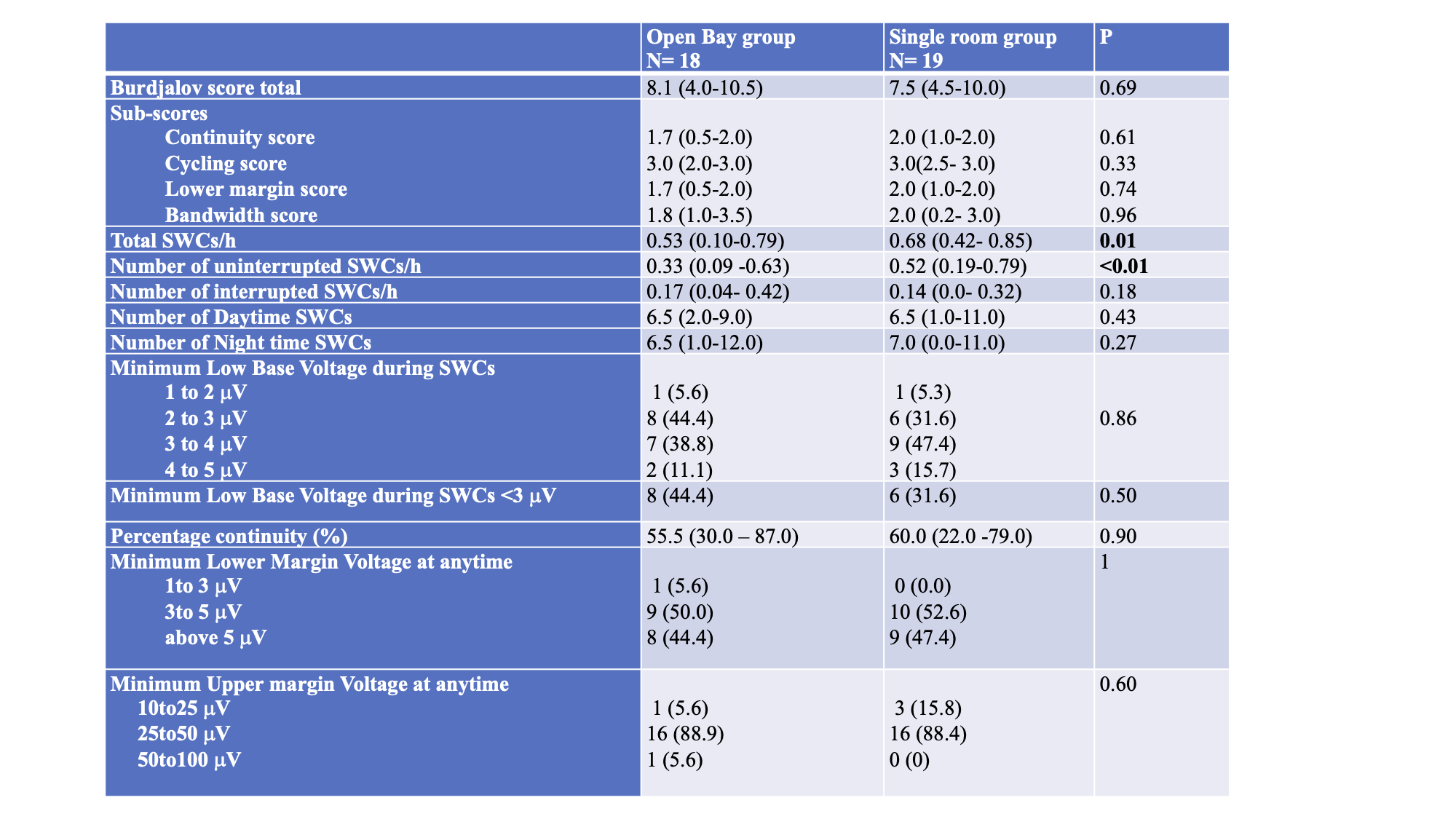 Data are presented as N (proportion) or median (range) as appropriate.
Data are presented as N (proportion) or median (range) as appropriate.
SWC: Sleep-wake cycle
Objective: To compare cerebral maturation and SWC on aEEG in extremely preterm neonates cared for in a tertiary NICU before and after layout change from OB to SR design.
Design/Methods: Mount Sinai Hospital in Toronto moved from an OB to SR NICU design in February 2015. Neonates born between gestational age (GA) 24+0 – 28+6 weeks and admitted to our NICU before (OB period) and after (SR period) design change were prospectively recruited and had single-channel aEEG recording between corrected GA 30+0 - 30+6 weeks, continuously for a period of 24 hours. Infants with intraventricular hemorrhage Grade 3, those receiving mechanical ventilation or treatment for sepsis at corrected GA 30 weeks were excluded. Recorded aEEG traces were divided into 6-hour segments and analyzed offline using visual inspection in random order. Lower (LMV) and upper (UMV) margin voltages were identified and background pattern was classified as continuous (C, LMV >5mV), discontinuous (DC, LMV 2-5mV and variable) or burst suppression (BS, LMV 0-3mV and non-variable). Uninterrupted SWCs were identified as periods of gradual fall and rise of LMV lasting ≥20 minutes (Figure 1). The primary outcome was aEEG maturation assessed using the Burdjalov score, which incorporates sub-scores for continuity, SWC, LMV, and bandwidth. Sub-score components, SWC number, and characteristics were secondary outcomes.
Results: Eighteen and 19 infants were included during OB and SR periods, respectively, with similar demographics (Table 1); C-sections were more frequent in the OB group. aEEG pattern was C or DC for all segments, except 2 infants who demonstrated a short segment ( < 1 hour) of BS pattern (1 each during OB and SR period). No differences were observed in any maturation-related aEEG variables, except the SR group showing higher total and uninterrupted SWCs per hour of recording (Table 2). Conclusion(s): SR NICU design may be associated with a higher number of total and uninterrupted SWCs in extremely preterm neonates. Further studies should focus on the relationship between higher sleep during the NICU period and neurodevelopmental outcomes.
Table 1. Baseline Characteristics
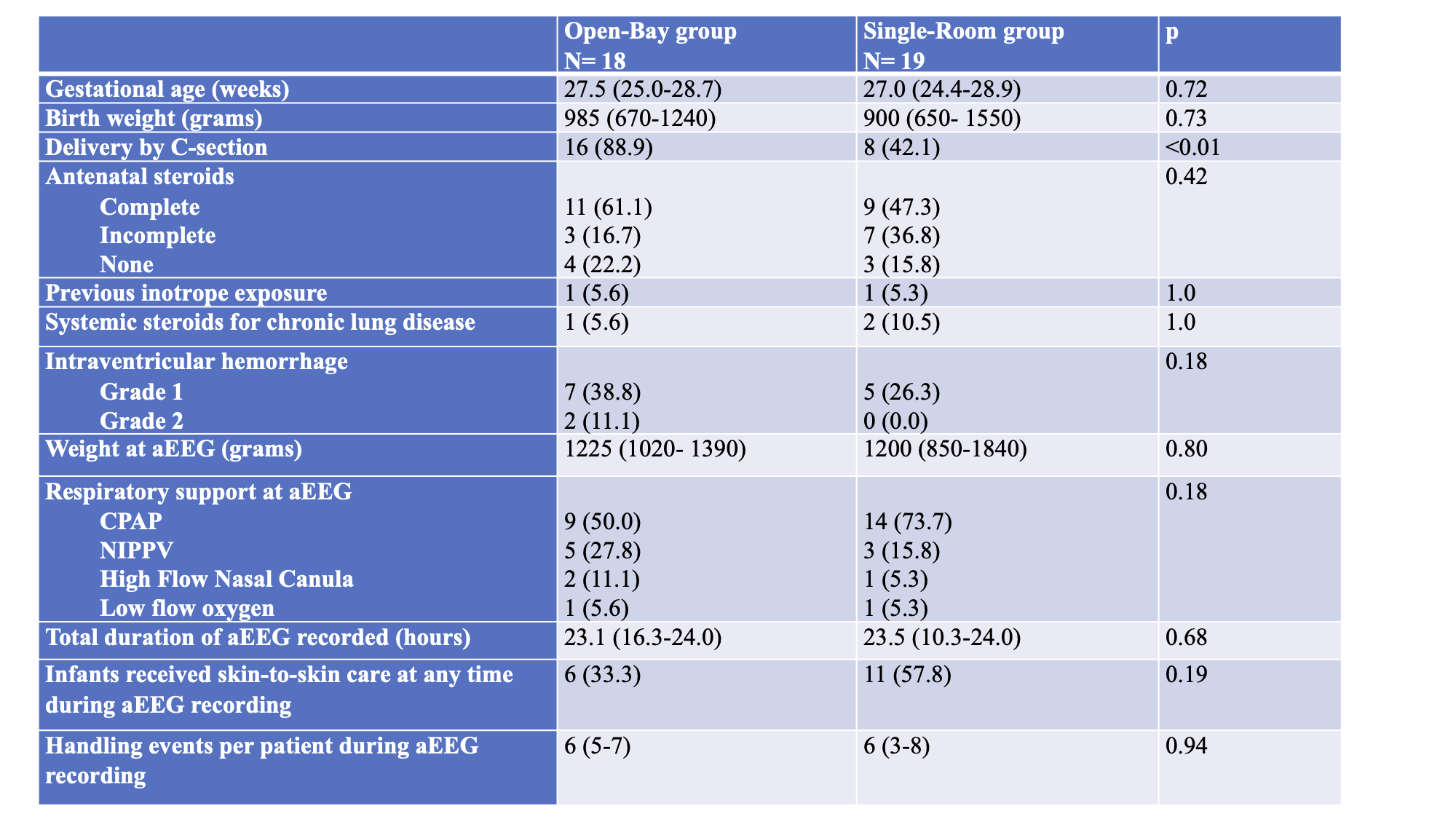 Data are presented as N (proportion) or median (range) as appropriate.
Data are presented as N (proportion) or median (range) as appropriate.CPAP: Continuous Positive Airway Pressure, NIPPV: Non-invasive Positive Pressure Ventilation
Table 2: Differences in aEEG characteristics
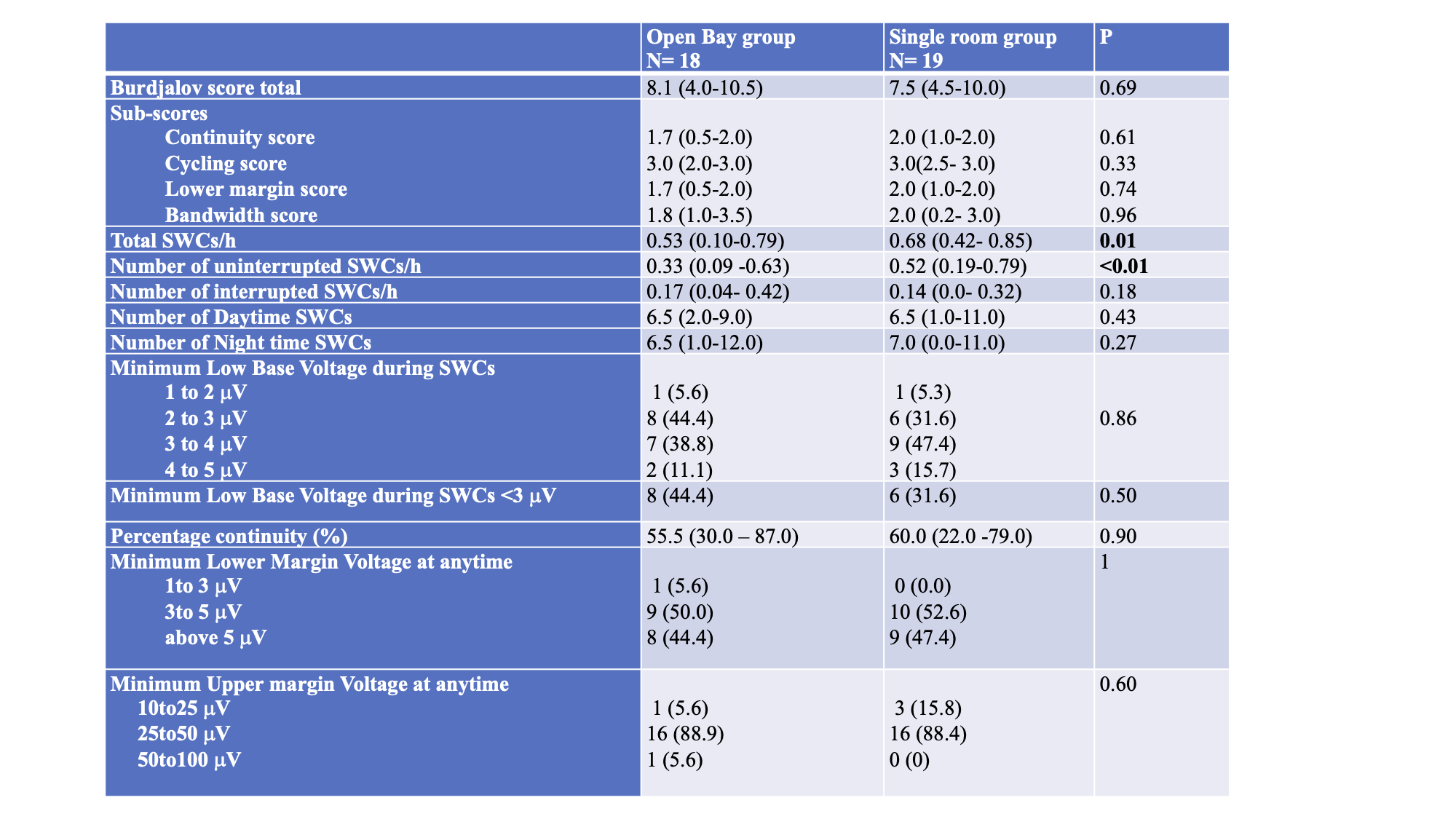 Data are presented as N (proportion) or median (range) as appropriate.
Data are presented as N (proportion) or median (range) as appropriate.SWC: Sleep-wake cycle
