Hematology/Oncology
Category: Abstract Submission
Hematology/Oncology II
578 - Spontaneous Calvarial Infarction with Epidural Hematoma and Subgaleal Hemorrhage in a Teenager with Sickle Cell SS Disease and Glucose-6-Phosphate Dehydrogenase Deficiency
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 578
Publication Number: 578.321
Publication Number: 578.321
Jennifer Nestor, The Children's Regional Hospital at Cooper, Philadelphia, PA, United States; Danielle Sanders, Cooper Medical School of Rowan University, Willingboro, NJ, United States; Sukrita S. Mysore, Cooper Medical School of Rowan University, Baltimore, MD, United States; Aubri M. Milano, The Children's Regional Hospital at Cooper, Cinnaminson, NJ, United States; Renata Ostrowicki, Cooper Medical School of Rowan University, Camden, NJ, United States; Thomas J. Presenza, Cooper University Hospital, Camden, NJ, United States; Emily Scattergood, Cooper university hospital, Camden, NJ, United States; Odiraa C. Nwankwor, Nemours Children's Hospital, Moorestown, NJ, United States; Rafat Ahmed, Cooper Medical School of Rowan University, Camden, NJ, United States

Jennifer Nestor, MD
Resident Physician
The Children's Regional Hospital at Cooper
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Sequelae of sickle cell disease (SCD) are often the result of vaso-occlusion (VOC) resulting from the dysmorphic shape of sickled red blood cells (RBC). Bone infarction occurs commonly in patients with sickle cell, most notably in long bones and axial skeleton. Infarct occurs much less frequently in the bones of the skull. Calvarial bone infarct results in MRI findings of T2 hyperintensity in areas of bone marrow edema with associated hemorrhage. Headaches in children with SCD are more likely to be due to severe underlying cerebral pathologies than in those children without SCD. When evaluating a child with SCD presenting with headache, consideration should be given to bony infarct.
Objective: The purpose of this case study is to discuss an uncommon sequela of SCD in a pediatric patient
Design/Methods: Single subject case study
Results: A 15 year old male with a history of sickle cell disease (type SS) and G6PD deficiency presented with chief complaints of headache and swelling over the left parietal region for two days with associated left sided visual disturbance. He denied head trauma or seizure-like activity. Upon presentation, he was febrile with tachycardia and a normal neurological exam. CT scan of his head was significant for a left subgaleal hemorrhage and bilateral epidural midline and left parietal fluid collections consistent with bone marrow infarcts and associated subacute epidural hematomas, without evidence of brain parenchymal injury, stroke or sinus venous thrombosis. A follow up MRI obtained during hospitalization indicated that the left subgaleal hematoma remained stable with breakdown of subgaleal blood products. The patient was treated primarily with supportive care including hydration, packed red blood cell transfusions and pain management. He did not require neurosurgical intervention. His hospital course was complicated by additional VOCs, sickle cell hepatopathy and acute chest syndrome. Conclusion(s): Rarely, calvarial VOC has resulted in epidural hematoma. In this case, calvarial infarct with unilateral headache, acute vision loss and acute cranial swelling resulted in subgaleal hemorrhage. This clinically significant finding results from bleeding between the periosteum and scalp galea aponeurosis, which may lead to hypovolemic shock. Calvarial infarcts should be considered on the differential in sickle cell disease patients presenting with a headache and visual deficits as prompt diagnosis can improve morbidity outcomes.
MRI Image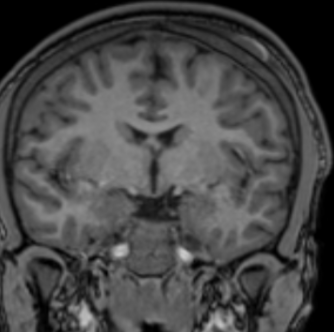 Coronal view of subgaleal hematoma.
Coronal view of subgaleal hematoma.
Objective: The purpose of this case study is to discuss an uncommon sequela of SCD in a pediatric patient
Design/Methods: Single subject case study
Results: A 15 year old male with a history of sickle cell disease (type SS) and G6PD deficiency presented with chief complaints of headache and swelling over the left parietal region for two days with associated left sided visual disturbance. He denied head trauma or seizure-like activity. Upon presentation, he was febrile with tachycardia and a normal neurological exam. CT scan of his head was significant for a left subgaleal hemorrhage and bilateral epidural midline and left parietal fluid collections consistent with bone marrow infarcts and associated subacute epidural hematomas, without evidence of brain parenchymal injury, stroke or sinus venous thrombosis. A follow up MRI obtained during hospitalization indicated that the left subgaleal hematoma remained stable with breakdown of subgaleal blood products. The patient was treated primarily with supportive care including hydration, packed red blood cell transfusions and pain management. He did not require neurosurgical intervention. His hospital course was complicated by additional VOCs, sickle cell hepatopathy and acute chest syndrome. Conclusion(s): Rarely, calvarial VOC has resulted in epidural hematoma. In this case, calvarial infarct with unilateral headache, acute vision loss and acute cranial swelling resulted in subgaleal hemorrhage. This clinically significant finding results from bleeding between the periosteum and scalp galea aponeurosis, which may lead to hypovolemic shock. Calvarial infarcts should be considered on the differential in sickle cell disease patients presenting with a headache and visual deficits as prompt diagnosis can improve morbidity outcomes.
MRI Image
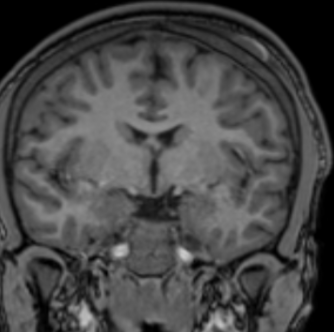 Coronal view of subgaleal hematoma.
Coronal view of subgaleal hematoma.