Breastfeeding/Human Milk
Category: Abstract Submission
Breastfeeding/Human Milk I
424 - States with Supportive Breastfeeding Policies Have Higher Rates of Very Preterm Infants Discharged Home on Any Human Milk
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 424
Publication Number: 424.301
Publication Number: 424.301
Erika M. Edwards, Robert Larner, M.D., College of Medicine at the University of Vermont, Burlington, VT, United States; Lucy T. Greenberg, Vermont Oxford Network, Burlington, VT, United States; Danielle Ehret, The University of Vermont Children's Hospital, Burlington, VT, United States; Margaret Parker, Boston Medical Center, Boston, MA, United States; Jeffrey D. Horbar, Larner College of Medicine University of Vermont, Burlington, VT, United States

Erika M. Edwards, PhD, MPH (she/her/hers)
Chief Scientific Officer and Director of Data Science
Vermont Oxford Network
Burlington, Vermont, United States
Presenting Author(s)
Background: Provision of human milk for very preterm infants confers short- and long-term benefits. Supportive state level breastfeeding policies modestly increase rates of breastfeeding in the healthy term population. Whether policies affect breastfeeding among very preterm infants is unclear.
Objective: To examine the rate of any human milk at discharge among very preterm infants in the US in 2019 by presence of state laws supporting breastfeeding
Design/Methods: We evaluated the rate of human milk feeding in the 24 hours before discharge, alone or in combination with fortifier or formula, among infants born from 22 to 29 completed weeks’ gestational age in 2019 and admitted to a Vermont Oxford Network member center within 28 days of birth in states with and without supportive breastfeeding laws enacted as of 2018 in five domains: (1) facilitating breastfeeding in the workplace (e.g., protected time and space for pumping, barring discrimination); (2) requiring insurance to cover breastfeeding assistance and training; (3) Medicaid coverage of donor milk; (4) hospital breastfeeding support practices (e.g., Baby-Friendly, STS care); and (5) paid or unpaid maternal leave. We also summed the number of policies by state. We calculated prevalence ratios adjusted for maternal race/ethnicity, a known driver of human milk at discharge, by the presence or absence of policies and by the number of policies.
Results: In 2019, 728 centers reported 21,018 eligible infants, of which 46.2% received any human milk at discharge. Infants who received care in states with policies supporting facilitating breastfeeding in the workplace, Medicaid coverage of donor milk, helping hospitals support breastmilk feeding, or paid or unpaid leave were more likely to be discharged on human milk than infants who received care in states without such policies (Figure). The number of policies in each state ranged from 0 to 5. In states with 3 or more policies, 56.7% of infants were discharged home on human milk compared to 40.9% in states with no policies, 41.9% in states with 1 policy, and 44.9% in states with 2 policies. As the number of policies increased, the prevalence of going home on human milk increased 7% (95% CI: 5%, 9%) after adjustment (Figure).Conclusion(s): Similar to studies examining the healthy term population, rates of any human milk at discharge among very preterm infants was greater in states with supportive breastfeeding policies. Having 3 or more policies also significantly increased any human milk at discharge rates. These findings can inform lactation advocacy efforts among the US neonatology community.
Proportion of Very Preterm Infants Discharged Home on Human Milk by Presence or Absence of State Laws Supporting Breastfeeding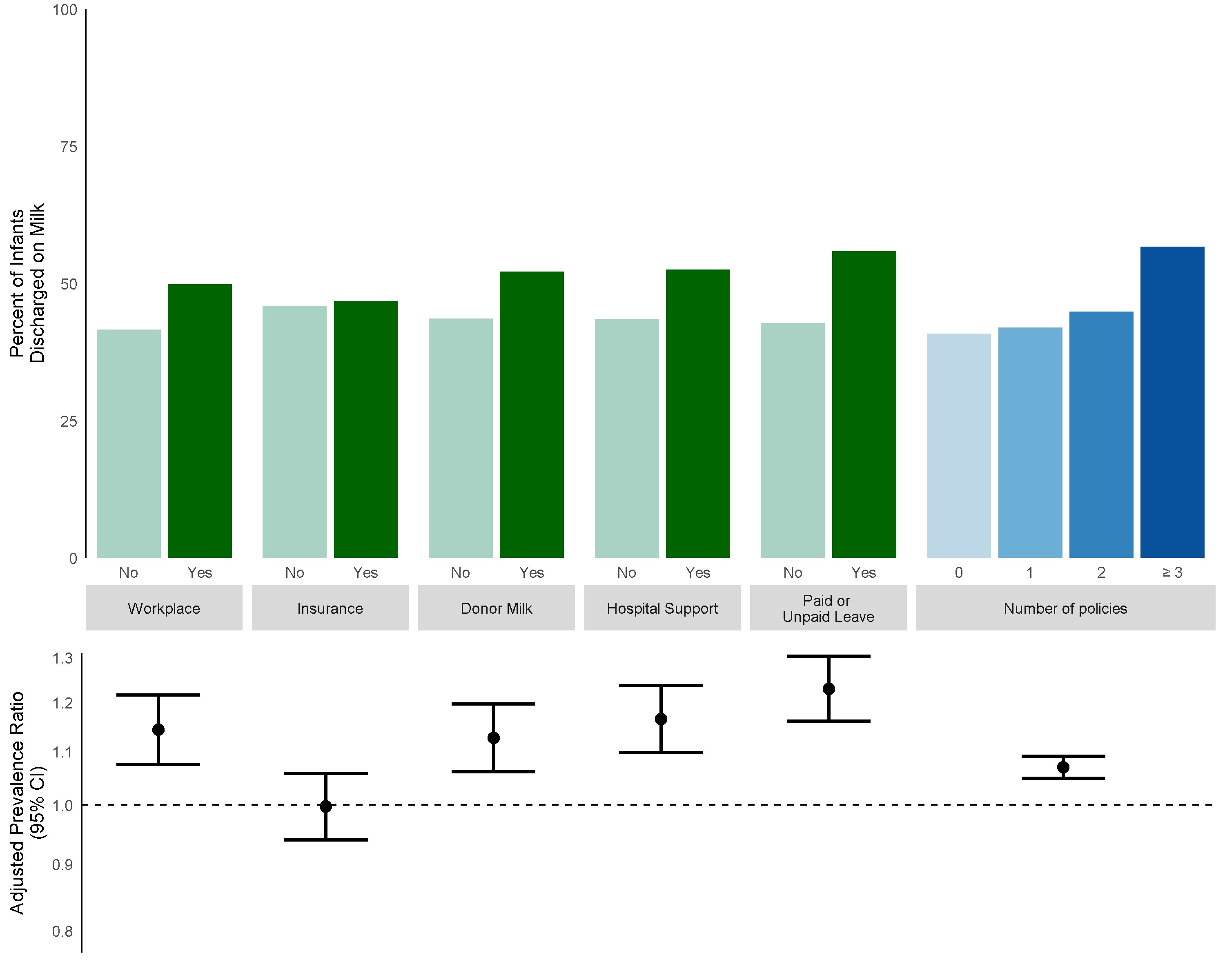 Green bars represent presence or absence of specific types of laws (facilitating breastfeeding the workplace; requiring insurance to cover breastfeeding assistance and training; Medicaid coverage of donor milk; hospital breastfeeding support policies; paid or unpaid medical leave). Blue bars represent total number of policies per state. Prevalence ratios with 95% confidence intervals are adjusted for maternal race/ethnicity.
Green bars represent presence or absence of specific types of laws (facilitating breastfeeding the workplace; requiring insurance to cover breastfeeding assistance and training; Medicaid coverage of donor milk; hospital breastfeeding support policies; paid or unpaid medical leave). Blue bars represent total number of policies per state. Prevalence ratios with 95% confidence intervals are adjusted for maternal race/ethnicity.
Objective: To examine the rate of any human milk at discharge among very preterm infants in the US in 2019 by presence of state laws supporting breastfeeding
Design/Methods: We evaluated the rate of human milk feeding in the 24 hours before discharge, alone or in combination with fortifier or formula, among infants born from 22 to 29 completed weeks’ gestational age in 2019 and admitted to a Vermont Oxford Network member center within 28 days of birth in states with and without supportive breastfeeding laws enacted as of 2018 in five domains: (1) facilitating breastfeeding in the workplace (e.g., protected time and space for pumping, barring discrimination); (2) requiring insurance to cover breastfeeding assistance and training; (3) Medicaid coverage of donor milk; (4) hospital breastfeeding support practices (e.g., Baby-Friendly, STS care); and (5) paid or unpaid maternal leave. We also summed the number of policies by state. We calculated prevalence ratios adjusted for maternal race/ethnicity, a known driver of human milk at discharge, by the presence or absence of policies and by the number of policies.
Results: In 2019, 728 centers reported 21,018 eligible infants, of which 46.2% received any human milk at discharge. Infants who received care in states with policies supporting facilitating breastfeeding in the workplace, Medicaid coverage of donor milk, helping hospitals support breastmilk feeding, or paid or unpaid leave were more likely to be discharged on human milk than infants who received care in states without such policies (Figure). The number of policies in each state ranged from 0 to 5. In states with 3 or more policies, 56.7% of infants were discharged home on human milk compared to 40.9% in states with no policies, 41.9% in states with 1 policy, and 44.9% in states with 2 policies. As the number of policies increased, the prevalence of going home on human milk increased 7% (95% CI: 5%, 9%) after adjustment (Figure).Conclusion(s): Similar to studies examining the healthy term population, rates of any human milk at discharge among very preterm infants was greater in states with supportive breastfeeding policies. Having 3 or more policies also significantly increased any human milk at discharge rates. These findings can inform lactation advocacy efforts among the US neonatology community.
Proportion of Very Preterm Infants Discharged Home on Human Milk by Presence or Absence of State Laws Supporting Breastfeeding
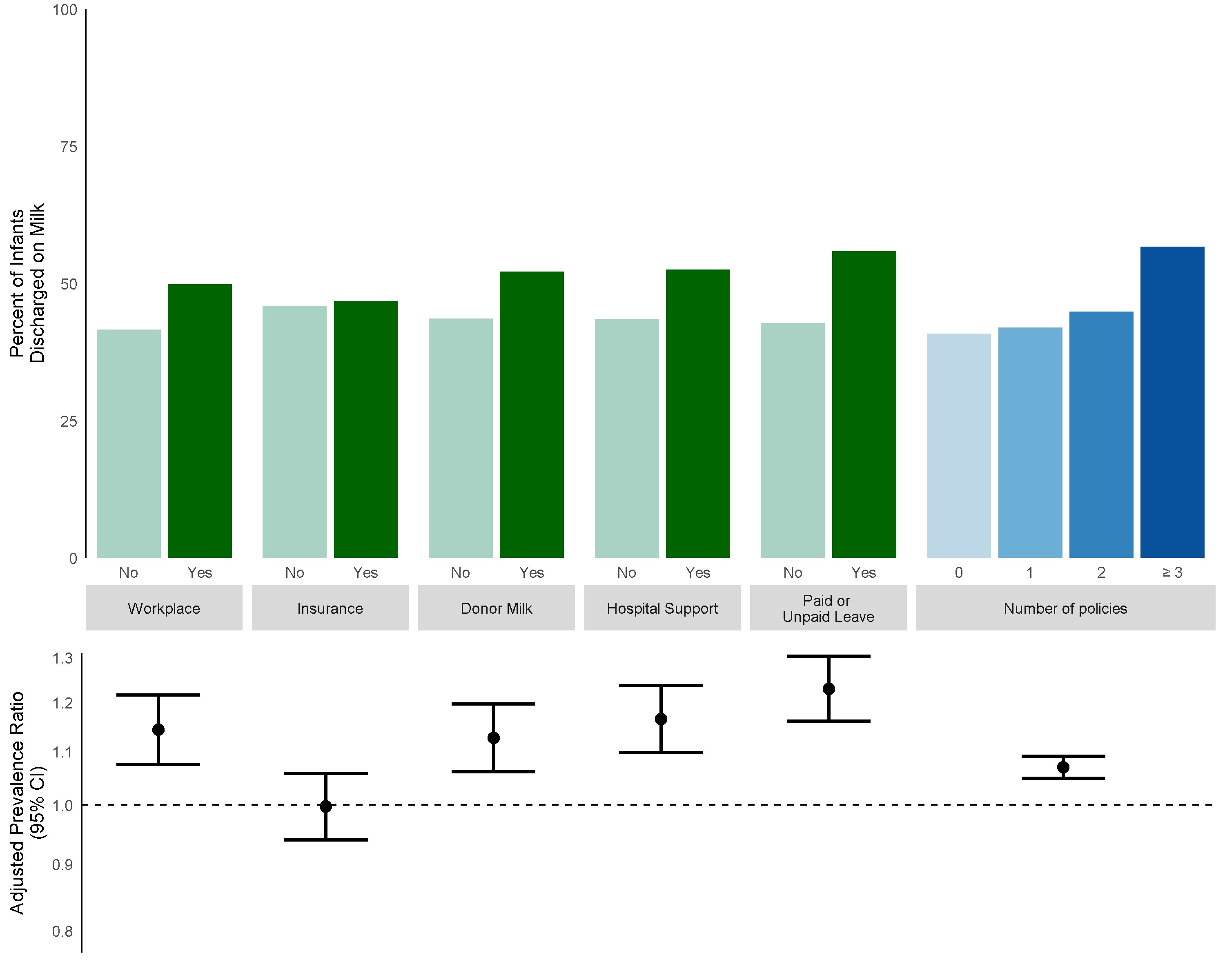 Green bars represent presence or absence of specific types of laws (facilitating breastfeeding the workplace; requiring insurance to cover breastfeeding assistance and training; Medicaid coverage of donor milk; hospital breastfeeding support policies; paid or unpaid medical leave). Blue bars represent total number of policies per state. Prevalence ratios with 95% confidence intervals are adjusted for maternal race/ethnicity.
Green bars represent presence or absence of specific types of laws (facilitating breastfeeding the workplace; requiring insurance to cover breastfeeding assistance and training; Medicaid coverage of donor milk; hospital breastfeeding support policies; paid or unpaid medical leave). Blue bars represent total number of policies per state. Prevalence ratios with 95% confidence intervals are adjusted for maternal race/ethnicity.