Neonatal Fetal Nutrition & Metabolism
Category: Abstract Submission
Neonatal Fetal Nutrition & Metabolism IV
451 - Mid-upper arm circumference as a predictor of body composition in ELBW infants
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 451
Publication Number: 451.335
Publication Number: 451.335
Emily Niemyjski, Baylor College of Medicine, Houston, TX, United States; Laura A. Gollins, Texas Children's Hospital, Houston, TX, United States; Jana Unger, Baylor College of Medicine, Houston, TX, United States; Pamela S. Gordon, Texas Children's Hospital, Friendswoos, TX, United States; Joseph Hagan, Baylor College of Medicine, Houston, TX, United States; Roman Shypailo, Baylor College of Medicine, Houston, TX, United States; Amy B. Hair, Baylor College of Medicine, Houston, TX, United States

Emily Niemyjski, DO
Neonatal Perinatal Medicine Fellow
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Early changes in body composition have been found to be potentially predictive of metabolic and neurodevelopmental outcomes later in life. In addition, infants and children who gain more fat mass early in life and/or at a more rapid rate are at increased risk of childhood and adult obesity. Mid-upper arm circumference (MUAC) is a simple anthropometric measure found to be a predictor of body mass index (BMI), severe malnutrition, and mortality in various populations. In premature infants specifically, MUAC was found to be a reliable method for estimating adiposity at near term corrected gestational age (CGA), compared to air displacement plethysmography. However, there are no studies which have examined MUAC as an in-hospital tool for assessment of body composition when compared to dual-energy X-ray absorptiometry (DXA).
Objective: To examine the correlation of MUAC measures with body composition parameters measured by DXA in extremely low birth weight (ELBW) infants.
Design/Methods: As part of a longitudinal cohort study, preterm infants were evaluated at near 36 weeks CGA. Weight, length, head circumference (HC), and BMI measures were obtained at birth and near 36 weeks CGA. DXA measures were obtained near 36 weeks CGA and MUAC was measured within 1 week of DXA analysis. Linear regression and correlation analysis were used to assess bivariate linear associations.
Results:
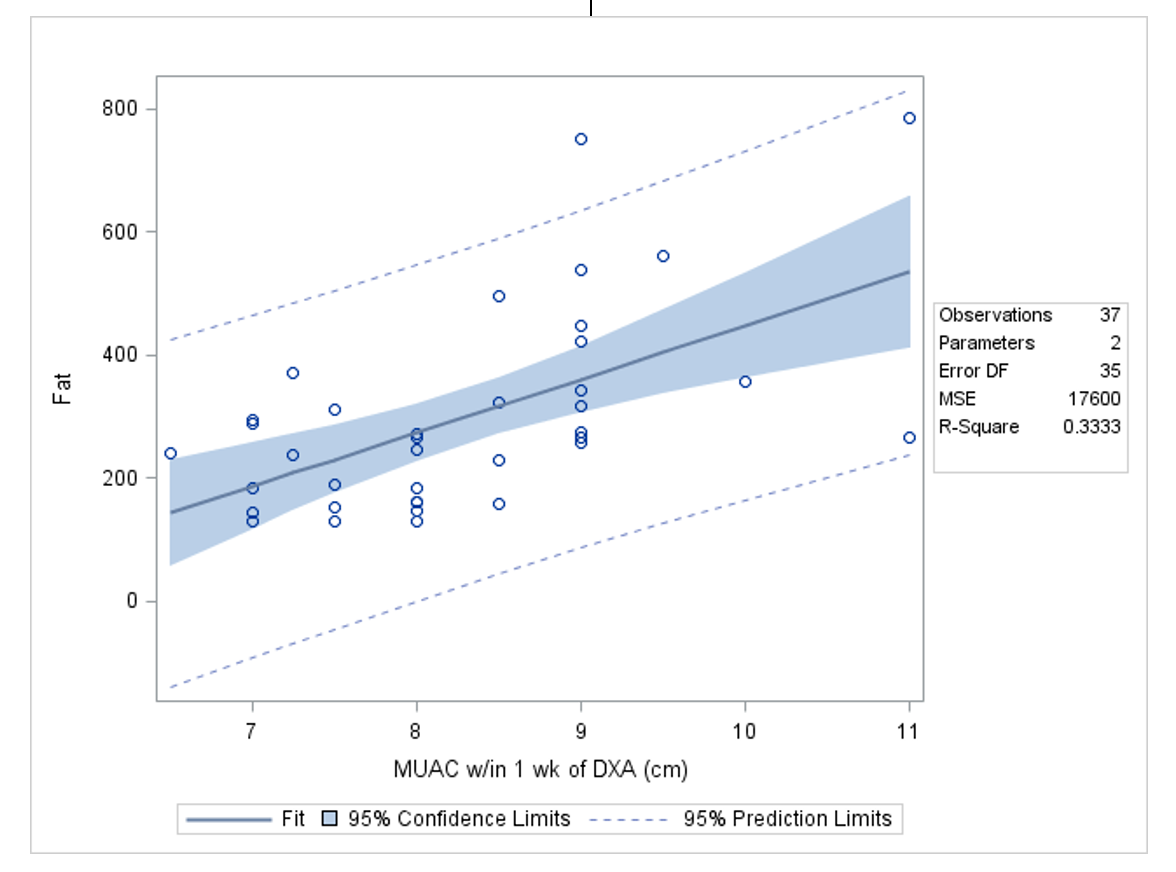
We evaluated 37 preterm infants with gestational age at birth of 26.5 ± 2.2 weeks and birth weight 831 ± 145 grams at CGA of 37.9 ± 2.5 weeks (Mean ± Standard Deviation). MUAC was significantly correlated with DXA fat mass, DXA lean mass, DXA fat free mass, DXA bone mineral density (BMD), DXA bone mineral content (BMC), and BMI at 36 weeks CGA. MUAC obtained within 1 week of DXA best predicted DXA fat mass (R2=0.333).
Conclusion(s): MUAC performed near 36 weeks CGA can be an inexpensive and informative bedside measure of body composition and nutritional status in ELBW infants. MUAC correlated with DXA fat mass (R2= 0.33), but remains an insufficient sole predictor overall because of the high variability in individual values. However, MUAC has the potential to be utilized in combination with other anthropometric measures of growth in preterm infants to direct nutrient intake and optimize body composition and growth.
Table 1: Correlations with Mid-Upper Arm Circumference.png) BMC: Bone Mineral Content, BMD: Bone Mineral Density, BMI: Body Mass Index
BMC: Bone Mineral Content, BMD: Bone Mineral Density, BMI: Body Mass Index
Figure A. Correlation between Mid-Upper Arm Circumference and DXA Fat Mass Measures.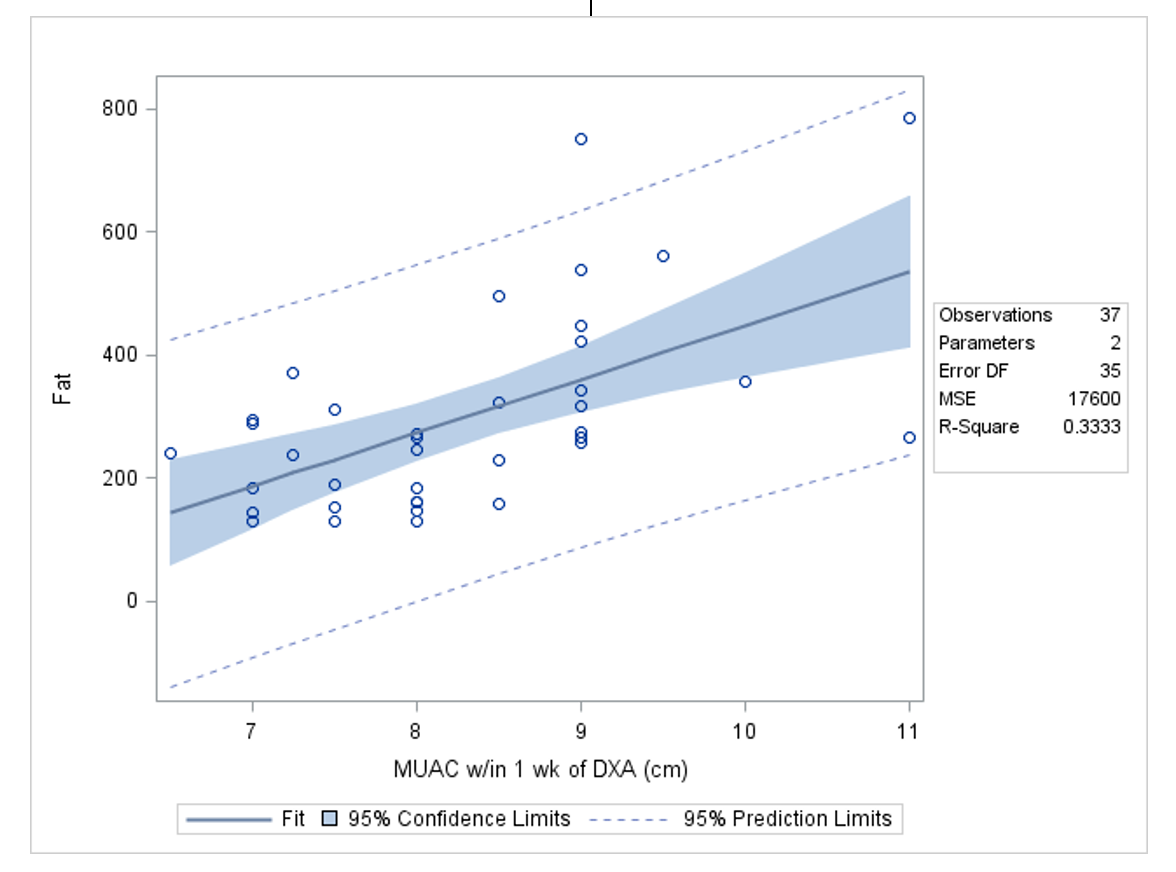
Objective: To examine the correlation of MUAC measures with body composition parameters measured by DXA in extremely low birth weight (ELBW) infants.
Design/Methods: As part of a longitudinal cohort study, preterm infants were evaluated at near 36 weeks CGA. Weight, length, head circumference (HC), and BMI measures were obtained at birth and near 36 weeks CGA. DXA measures were obtained near 36 weeks CGA and MUAC was measured within 1 week of DXA analysis. Linear regression and correlation analysis were used to assess bivariate linear associations.
Results:
We evaluated 37 preterm infants with gestational age at birth of 26.5 ± 2.2 weeks and birth weight 831 ± 145 grams at CGA of 37.9 ± 2.5 weeks (Mean ± Standard Deviation). MUAC was significantly correlated with DXA fat mass, DXA lean mass, DXA fat free mass, DXA bone mineral density (BMD), DXA bone mineral content (BMC), and BMI at 36 weeks CGA. MUAC obtained within 1 week of DXA best predicted DXA fat mass (R2=0.333).
Conclusion(s): MUAC performed near 36 weeks CGA can be an inexpensive and informative bedside measure of body composition and nutritional status in ELBW infants. MUAC correlated with DXA fat mass (R2= 0.33), but remains an insufficient sole predictor overall because of the high variability in individual values. However, MUAC has the potential to be utilized in combination with other anthropometric measures of growth in preterm infants to direct nutrient intake and optimize body composition and growth.
Table 1: Correlations with Mid-Upper Arm Circumference
.png) BMC: Bone Mineral Content, BMD: Bone Mineral Density, BMI: Body Mass Index
BMC: Bone Mineral Content, BMD: Bone Mineral Density, BMI: Body Mass IndexFigure A. Correlation between Mid-Upper Arm Circumference and DXA Fat Mass Measures.