Breastfeeding/Human Milk
Category: Abstract Submission
Breastfeeding/Human Milk I
410 - Adressing racial disparities in maternal milk provision to infants in the NICU
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 410
Publication Number: 410.301
Publication Number: 410.301
Stacy Drury, Tulane University School of Medicine, New Orleans, LA, United States; Renee I. Tristano, Tulane University School of Medicine, New Orleans, LA, United States; Sofia Cabrera, Tulane University School of Medicine, New Orleans, LA, United States; Margaret Parker, Boston Medical Center, Boston, MA, United States

Stacy Drury, MD/PhD
Vice Chair of Research, Pediatrics
Tulane University School of Medicine
New Orleans, Louisiana, United States
Presenting Author(s)
Background: Very low birth weight (VLBW; ≤ 1,500 grams) and its associated adverse health outcomes differentially impact minoritized individuals in the US. Despite the established benefits of maternal milk (MOM) only 50-55% of mothers provide any MOM for their VLBW infants at the point of discharge from the neonatal intensive care unit (NICU). In the Gulf South, Black mothers of VLBW infants are less likely to provide MOM compared to white mothers.
Objective: To create a QI multi-hospital collaborative dedicated to increasing the provision of MOM to VLBW infants.
Design/Methods: A multi-NICU QI collaborative that included (1) regular webinars/in-person meetings focused on best practices and PDSAs in relation to key drivers of sustained MOM provision (2) development of hospital based, free loaner programs of hospital grade breast milk pumps for mothers with infants in the NICU and (3) creation of a free milk truck delivery service providing pickup and delivery of MOM to the NICU, transport of loaner breast pumps, and delivery of donor milk from a local milk bank to participating NICUs.
Results: Baseline data was collected via VON between 2016 and 2018. Data collection began July 1 of 2019 and will continue through April 2022. Data through 2021, on the percentage of infants receiving any MOM on the day of discharge from the NICU is presented in Figure 1. This percentage increased from a baseline of 37% to 57% averaged across all 8 participating level III and IV NICUs. One key barrier to maternal milk provision identified across all NICUs was breast pump accessibility. To address this, we purchased a set of hospital grade pumps that were distributed to the NICUs to develop and implement a fee-free loaner breast pump program to facilitate maternal breast milk production. Figure 2 presents the data comparing maternal milk provision at multiple time points for mothers who received loaner pump compared to mothers at the same hospital who did not receive a loaner pump. Notably while only 50% of non-loaner pump recipient infants received maternal milk at day of life 7, 100% of those infants whose mothers received a loaner pump received maternal milk on day of life 7. At discharge there remained significant improvement in the percentage of infants receiving maternal milk from mothers who received a loaner pump (68%) compared to mothers who did not (38%)Conclusion(s): Through this QI collaborative, the development of fee-free hospital grade loaner breast pump programs, and the utilization of a milk/breast pump delivery truck this collaborative has significantly increased maternal milk provision to VLBW infants, despite the last 18 months of the COVID pandemic.
Figure 1.png) The change over time of the provision of maternal milk (MOM) to VLBW infants in the NICUs
The change over time of the provision of maternal milk (MOM) to VLBW infants in the NICUs
Figure 2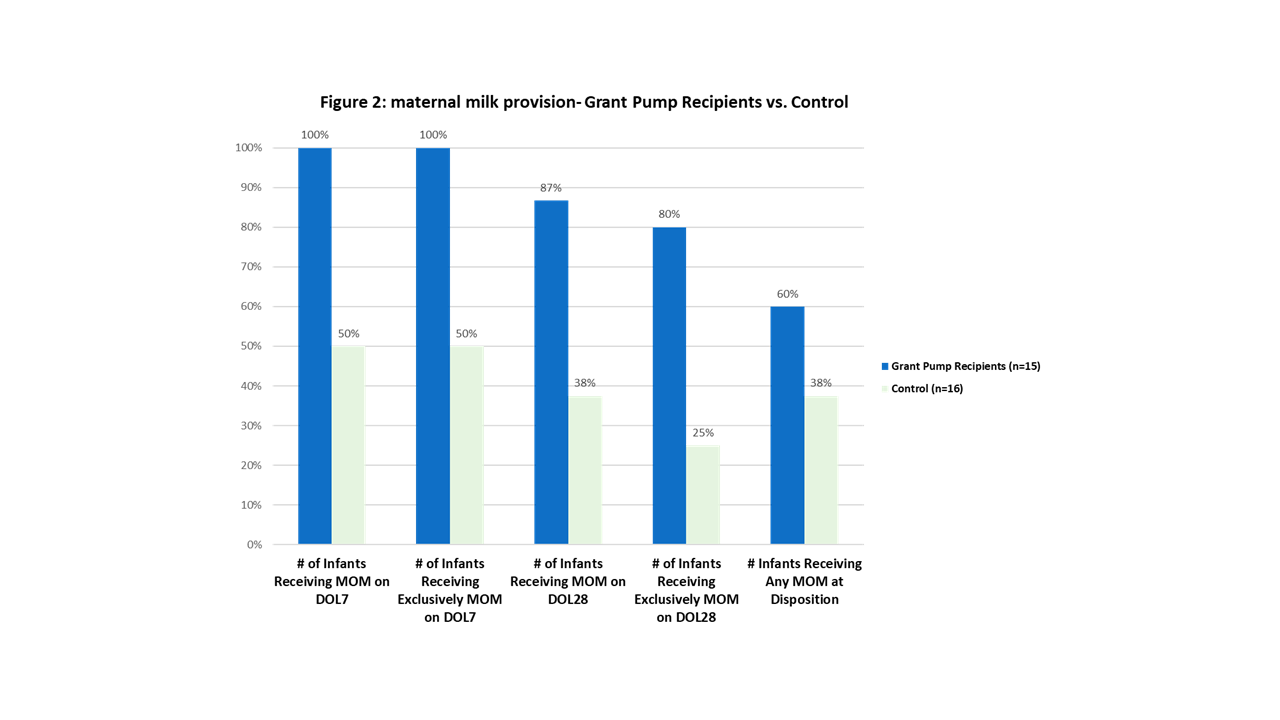 The effect of the implementatino of a fee-free hospital grade breast pump loaner program on the provision of maternal milk (MOM) to VLBW infants in the NICU over the course of the infant's NICU stay
The effect of the implementatino of a fee-free hospital grade breast pump loaner program on the provision of maternal milk (MOM) to VLBW infants in the NICU over the course of the infant's NICU stay
Objective: To create a QI multi-hospital collaborative dedicated to increasing the provision of MOM to VLBW infants.
Design/Methods: A multi-NICU QI collaborative that included (1) regular webinars/in-person meetings focused on best practices and PDSAs in relation to key drivers of sustained MOM provision (2) development of hospital based, free loaner programs of hospital grade breast milk pumps for mothers with infants in the NICU and (3) creation of a free milk truck delivery service providing pickup and delivery of MOM to the NICU, transport of loaner breast pumps, and delivery of donor milk from a local milk bank to participating NICUs.
Results: Baseline data was collected via VON between 2016 and 2018. Data collection began July 1 of 2019 and will continue through April 2022. Data through 2021, on the percentage of infants receiving any MOM on the day of discharge from the NICU is presented in Figure 1. This percentage increased from a baseline of 37% to 57% averaged across all 8 participating level III and IV NICUs. One key barrier to maternal milk provision identified across all NICUs was breast pump accessibility. To address this, we purchased a set of hospital grade pumps that were distributed to the NICUs to develop and implement a fee-free loaner breast pump program to facilitate maternal breast milk production. Figure 2 presents the data comparing maternal milk provision at multiple time points for mothers who received loaner pump compared to mothers at the same hospital who did not receive a loaner pump. Notably while only 50% of non-loaner pump recipient infants received maternal milk at day of life 7, 100% of those infants whose mothers received a loaner pump received maternal milk on day of life 7. At discharge there remained significant improvement in the percentage of infants receiving maternal milk from mothers who received a loaner pump (68%) compared to mothers who did not (38%)Conclusion(s): Through this QI collaborative, the development of fee-free hospital grade loaner breast pump programs, and the utilization of a milk/breast pump delivery truck this collaborative has significantly increased maternal milk provision to VLBW infants, despite the last 18 months of the COVID pandemic.
Figure 1
.png) The change over time of the provision of maternal milk (MOM) to VLBW infants in the NICUs
The change over time of the provision of maternal milk (MOM) to VLBW infants in the NICUsFigure 2
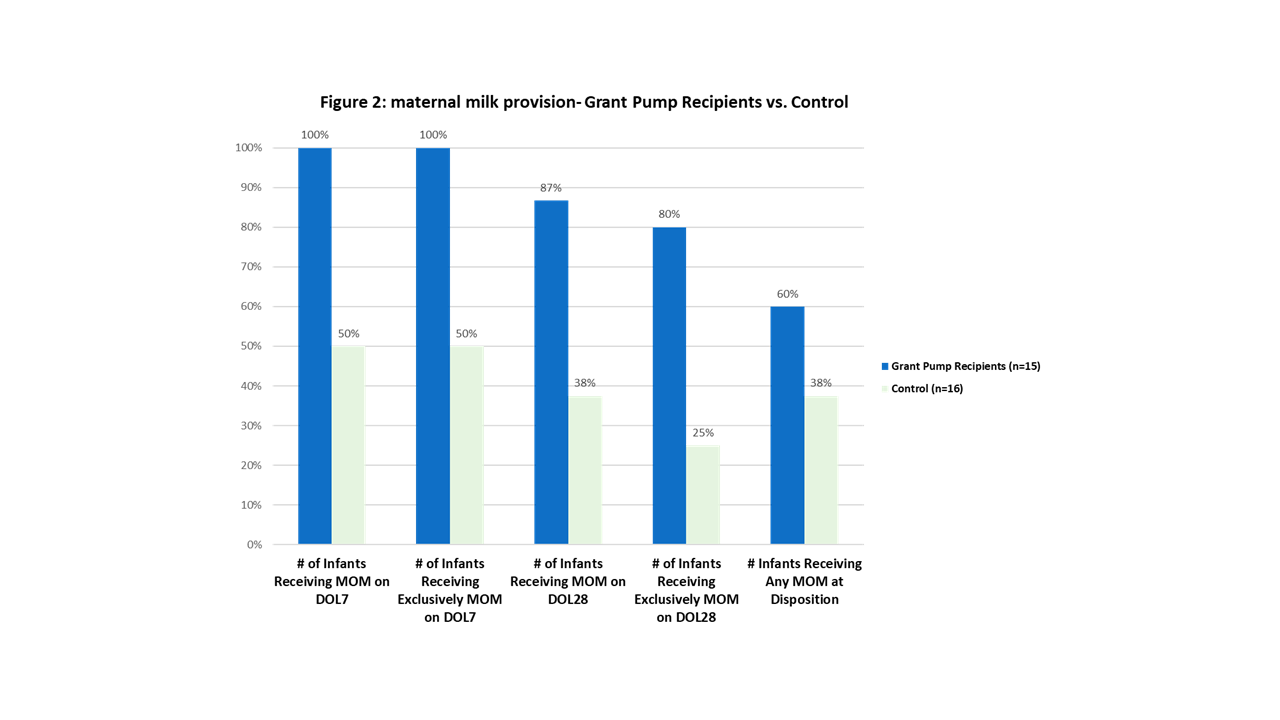 The effect of the implementatino of a fee-free hospital grade breast pump loaner program on the provision of maternal milk (MOM) to VLBW infants in the NICU over the course of the infant's NICU stay
The effect of the implementatino of a fee-free hospital grade breast pump loaner program on the provision of maternal milk (MOM) to VLBW infants in the NICU over the course of the infant's NICU stay