Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine X
381 - Airway Alignment: Consensus-based Development of a Pre-intubation Checklist for the Pediatric Emergency Department
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 381
Publication Number: 381.314
Publication Number: 381.314
Kelsey A. Miller, Boston Children's Hospital, Brookline, MA, United States; Monica M. Prieto, Childrens Hospital of Philadelphia, Swarthmore, PA, United States; Robyn Wing, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Michael P. Goldman, Yale School of Medicine, New Haven, CT, United States; Lee Polikoff, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Akira Nishisaki, The Children's Hospital of Philadelphia, Philadelphia, PA, United States; Joshua Nagler, Boston Children's Hospital Division of Emergency Medicine, Brookline, MA, United States
- KM
Kelsey A. Miller, MD, EdM (she/her/hers)
Attending Physician in Pediatric Emergency Medicine
Harvard Medical School
Brookline, Massachusetts, United States
Presenting Author(s)
Background: Intubation in the pediatric emergency department (PED) is a high-risk, low frequency event. Airway checklists have proven to be effective tools for safe intubations in pediatric intensive care units (PICUs), resulting in decreased tracheal intubation-associated adverse events. PED airway management differs from PICU management and critical items to include in a PED airway checklist are not yet defined.
Objective: To achieve expert multi-disciplinary consensus on a pre-intubation checklist for use in the PED.
Design/Methods: Thirty candidate items for the checklist were identified by review of the existing pre-intubation checklists created by the National Emergency Airway Registry for Kids. A modified Delphi was performed with experts consisting of National Emergency Airway Registry for Pediatric Emergency Medicine (NEAR4PEM) physician site directors, general emergency medicine physicians, neonatologists, and pediatric intensivists, anesthesiologists, and otorhinolaryngologists. All experts received an electronic questionnaire asking them to rank each item on a nine-point appropriateness scale. Median score and interquartile range were calculated for each item. Consensus was defined a priori as 75% of experts ranking an item 7 or higher on the scale. Experts could suggest new items for inclusion and changes to the wording of candidate items for subsequent rounds. The maximum number of rounds was capped at three.
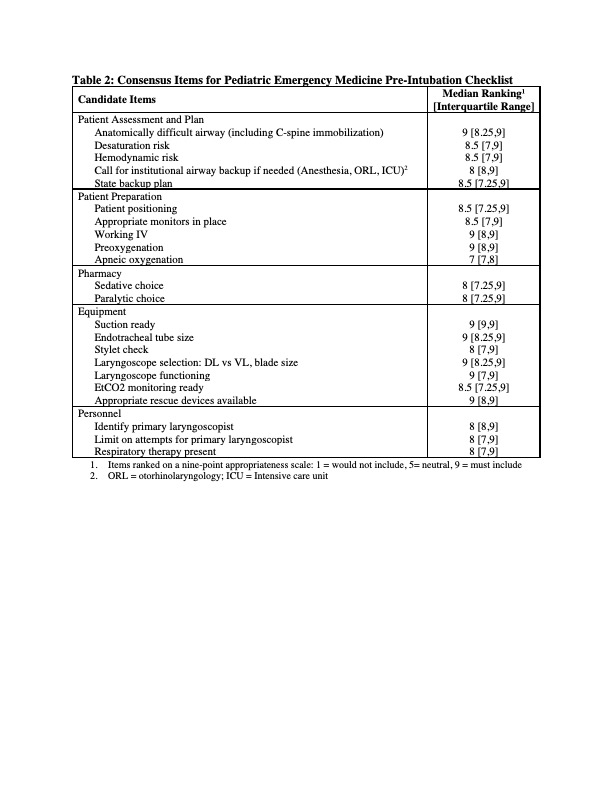
Results: Fourteen experts participated in the modified Delphi (Table 1). Consensus was achieved on 22 items after two rounds of the modified Delphi, and all experts completed both rounds of questionaries. Twelve of these items were original candidate items and 10 were newly suggested or modified items. Consensus items included the following categories: Patient Assessment and Plan (5 items), Patient Preparation (5 items), Pharmacy (2 items), Equipment (7 items), and Personnel (3 items). The final checklist items are presented in Table 2. Experts welcomed institutional-specific customization.Conclusion(s): Using the modified Delphi method, consensus was established among airway management experts within and outside of pediatric emergency medicine around a 22-item pre-intubation checklist for use in the PED. Next steps include engagement of human factors engineers to maximize formatting and generalizability of this checklist for all NEAR4PEM sites, and analysis of subsequent impact on intubation outcomes.
Table 1: Characteristics of Experts Participating in Modified Delphi (N = 14)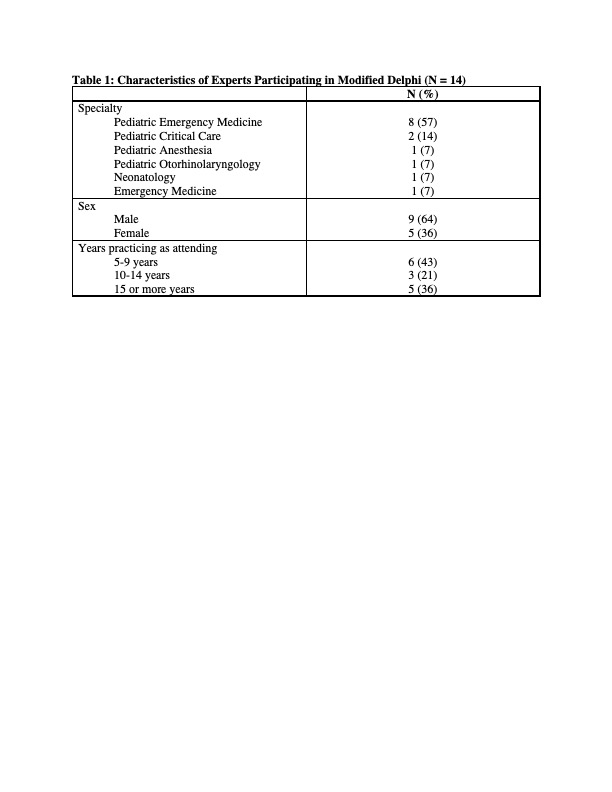
Table 2: Consensus Items for Pediatric Emergency Medicine Pre-Intubation Checklist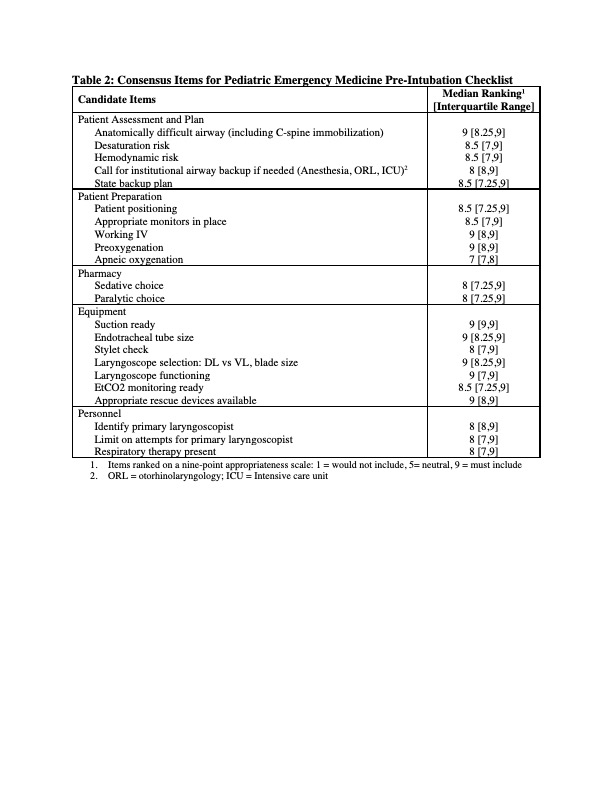
Objective: To achieve expert multi-disciplinary consensus on a pre-intubation checklist for use in the PED.
Design/Methods: Thirty candidate items for the checklist were identified by review of the existing pre-intubation checklists created by the National Emergency Airway Registry for Kids. A modified Delphi was performed with experts consisting of National Emergency Airway Registry for Pediatric Emergency Medicine (NEAR4PEM) physician site directors, general emergency medicine physicians, neonatologists, and pediatric intensivists, anesthesiologists, and otorhinolaryngologists. All experts received an electronic questionnaire asking them to rank each item on a nine-point appropriateness scale. Median score and interquartile range were calculated for each item. Consensus was defined a priori as 75% of experts ranking an item 7 or higher on the scale. Experts could suggest new items for inclusion and changes to the wording of candidate items for subsequent rounds. The maximum number of rounds was capped at three.
Results: Fourteen experts participated in the modified Delphi (Table 1). Consensus was achieved on 22 items after two rounds of the modified Delphi, and all experts completed both rounds of questionaries. Twelve of these items were original candidate items and 10 were newly suggested or modified items. Consensus items included the following categories: Patient Assessment and Plan (5 items), Patient Preparation (5 items), Pharmacy (2 items), Equipment (7 items), and Personnel (3 items). The final checklist items are presented in Table 2. Experts welcomed institutional-specific customization.Conclusion(s): Using the modified Delphi method, consensus was established among airway management experts within and outside of pediatric emergency medicine around a 22-item pre-intubation checklist for use in the PED. Next steps include engagement of human factors engineers to maximize formatting and generalizability of this checklist for all NEAR4PEM sites, and analysis of subsequent impact on intubation outcomes.
Table 1: Characteristics of Experts Participating in Modified Delphi (N = 14)
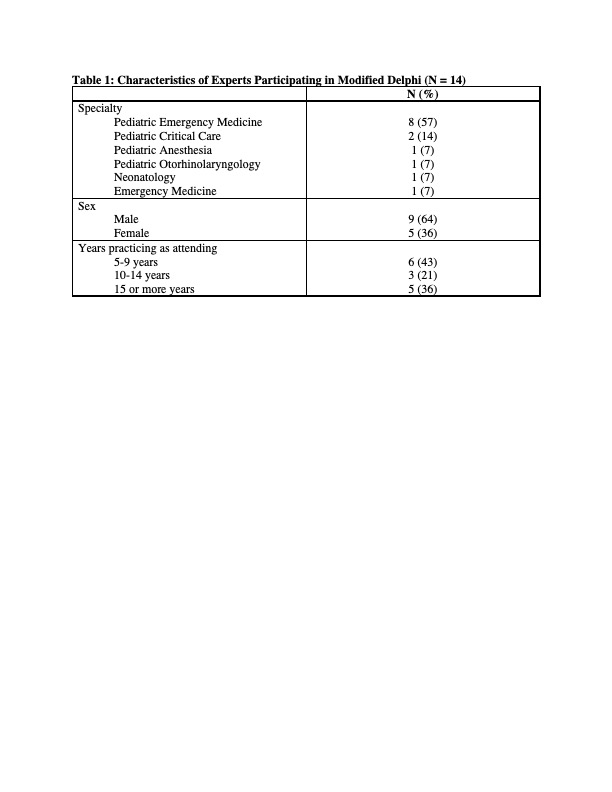
Table 2: Consensus Items for Pediatric Emergency Medicine Pre-Intubation Checklist