General Pediatrics: All Areas
Category: Abstract Submission
General Pediatrics II
603 - Approach to Isolated Prelabor Rupture of Membranes (PROM) risk factor and well Appearing Newborns in the Nursery
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 603
Publication Number: 603.209
Publication Number: 603.209
Pinchi Srinivasan, Mount Sinai South Nassau, Oceanside, NY, United States
- PS
Pinchi Srinivasan, MD, MBA
Clinical Associate Professor, Pediatrics
Icahn School of Medicine at Mount Sinai
NEW HYDE PARK, New York, United States
Presenting Author(s)
Background: Clinical risk factors for neonatal Early Onset Sepsis (EOS) are based on results of studies performed prior to widespread use of GBS- IAP. Widely adopted EOS score calculator uses multiple specified maternal risk factors available. Approach to asymptomatic well appearing neonates born to mothers with just isolated PROM in absence of other maternal risk factors has been variable especially sepsis screen evaluations. Reported frequency of PROM among term pregnancies is 8%. Most nurseries perform a partial sepsis screen (CBC Diff and Blood CS) on these babies
Objective: To describe the outcomes in well appearing neonates exposed to only PROM as a risk factor who underwent only vital sign (VS) observation q 4 hrs for 24 hours with no sepsis evaluation
Design/Methods: Retrospective review on mothers and newborns admitted to nursery between 2019-2020 from a regional hospital with ~2,200 deliveries/year (our baseline rate of EOS < 0.5/1000 births). All babies were examined and assessed with q 4 hr VS monitoring X 24 hours, followed by q 6 hr until discharge. Mothers with PROM (19hr-94 hrs) Mean 29.4 hrs, Total =309 (7% of all delivering mothers), only mothers with GA >35 Wks with PROM between 19hr-30hrs and their well appearing newborns admitted to WBN were reviewed, n=178. Mothers with intrapartum fever = 0
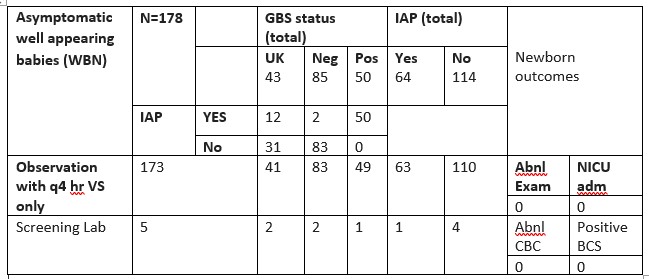
Results: None of the babies developed any symptoms or transferred to NICU. No rehospitalization noted in the first 30 days post discharge. 100% of mothers with positive GBS and only 28% of mothers with unknown GBS in the setting of PROM received IAP. Five babies had partial sepsis screen (CBC Diff/Blood CS) with normal results, (done as the new policy of utilizing EOS score evaluation was being implemented). Mothers with PROM comparison against antepartum GBS status and IAP use shown in table 1Conclusion(s): Despite a known monotonic relationship of increasing time of ROM with increased EOS risk, no convincing evidence of benefit is shown for mothers or neonates from the routine use of antibiotics for PROM at or near term as per Cochrane review, our approach to do exclusive clinical assessment with q 4 h VS monitoring in babies born to mothers with isolated PROM (19 hr- 30 hrs) as a risk factor was acceptable with none of these babies developing symptoms or requiring NICU admissions during their nursery stay. Frequent VS monitoring and structured clinical observation alone in the setting of a single isolated risk factor of PROM (19hrs-30hrs) can potentially eliminate unnecessary sepsis screen evaluations. Use of EOS score in with single risk factor in the absence of Chorioamnionitis needs to be explored.
Table 1.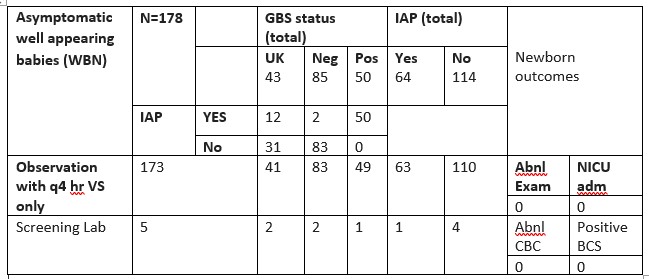
Objective: To describe the outcomes in well appearing neonates exposed to only PROM as a risk factor who underwent only vital sign (VS) observation q 4 hrs for 24 hours with no sepsis evaluation
Design/Methods: Retrospective review on mothers and newborns admitted to nursery between 2019-2020 from a regional hospital with ~2,200 deliveries/year (our baseline rate of EOS < 0.5/1000 births). All babies were examined and assessed with q 4 hr VS monitoring X 24 hours, followed by q 6 hr until discharge. Mothers with PROM (19hr-94 hrs) Mean 29.4 hrs, Total =309 (7% of all delivering mothers), only mothers with GA >35 Wks with PROM between 19hr-30hrs and their well appearing newborns admitted to WBN were reviewed, n=178. Mothers with intrapartum fever = 0
Results: None of the babies developed any symptoms or transferred to NICU. No rehospitalization noted in the first 30 days post discharge. 100% of mothers with positive GBS and only 28% of mothers with unknown GBS in the setting of PROM received IAP. Five babies had partial sepsis screen (CBC Diff/Blood CS) with normal results, (done as the new policy of utilizing EOS score evaluation was being implemented). Mothers with PROM comparison against antepartum GBS status and IAP use shown in table 1Conclusion(s): Despite a known monotonic relationship of increasing time of ROM with increased EOS risk, no convincing evidence of benefit is shown for mothers or neonates from the routine use of antibiotics for PROM at or near term as per Cochrane review, our approach to do exclusive clinical assessment with q 4 h VS monitoring in babies born to mothers with isolated PROM (19 hr- 30 hrs) as a risk factor was acceptable with none of these babies developing symptoms or requiring NICU admissions during their nursery stay. Frequent VS monitoring and structured clinical observation alone in the setting of a single isolated risk factor of PROM (19hrs-30hrs) can potentially eliminate unnecessary sepsis screen evaluations. Use of EOS score in with single risk factor in the absence of Chorioamnionitis needs to be explored.
Table 1.