Neonatal Nephrology/AKI
Category: Abstract Submission
Neonatal Nephrology/AKI I
116 - Renal Saturations and Detection of Acute Kidney Injury in the Preterm Infant with a Patent Ductus Arteriosus
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 116
Publication Number: 116.125
Publication Number: 116.125
Laura A. Rose, Stanford University School of Medicine, Palo Alto, CA, United States; Valerie Y. Chock, Stanford University School of Medicine, Sunnyvale, CA, United States; Adam Frymoyer, Stanford University School of Medicine, San Carlos, CA, United States; Shazia Bhombal, Stanford university, Palo Alto, CA, United States

Laura A. Rose, MD
Resident
Stanford Children's Health
Palo Alto, California, United States
Presenting Author(s)
Background: Preterm infants with a hemodynamically significant patent ductus arteriosus (hsPDA) are at risk of developing acute kidney injury (AKI). Near-infrared spectroscopy (NIRS) measurement of renal saturation has been used to characterize hsPDA and may further delineate those infants at highest risk for AKI.
Objective: To investigate renal saturation (RSat) as measured by NIRS for detection of AKI in neonates with a PDA.
Design/Methods: This single-center retrospective study investigated clinical, ECHO, and NIRS characteristics of 50 preterm infants ≤29 weeks gestation who underwent routine NIRS monitoring and ECHO due to concern for PDA. A PDA was classified as hemodynamically significant if two of the following were found on ECHO: moderate to large size, left-to-right shunting, descending aorta flow reversal, or left atrial enlargement. AKI was defined by neonatal Kidney Disease: Improving Global Outcomes [KDIGO] criteria. Only AKI occurring three days before until ten days after ECHO qualified in this study. Cerebral and renal saturations were evaluated for the 24 hour period prior to ECHO. Student t-test or Fisher’s exact test compared characteristics between groups. Logistic regression assessed the association between NIRS and AKI.
Results: Among 50 infants, hsPDA was found on ECHO in 35 infants (70%). Of infants with hsPDA, 15 (43%) developed AKI compared to 3 (20%) without hsPDA. No significant differences in demographics or PDA management were found in those with AKI versus no AKI (Table 1), however infants with AKI were less likely to be on dopamine on day of ECHO (p=0.04). RSat was not significantly associated with AKI (p=0.4) or hsPDA (p=0.2) (Table 3). Although dopamine use was not associated with SCr or RSat levels, infants on dopamine had significantly less variability in RSat (p=0.002). Infants with hsPDA had lower cerebral saturations than those without hsPDA (68% versus 74%, p=0.02) (Table 3).Conclusion(s): Renal NIRS measurements did not discriminate AKI in the preterm hsPDA population, however our data may not capture the optimal timing of measurement prior to AKI occurrence. Future research into the utility of NIRS monitoring and effect of dopamine on renal oxygenation is needed to better characterize the infant at high risk of AKI.
Neonatal Characteristics.jpg) Value are mean +/- SD or n (%); *on date of ECHO; +on date of NIRS
Value are mean +/- SD or n (%); *on date of ECHO; +on date of NIRS
Creatinine trends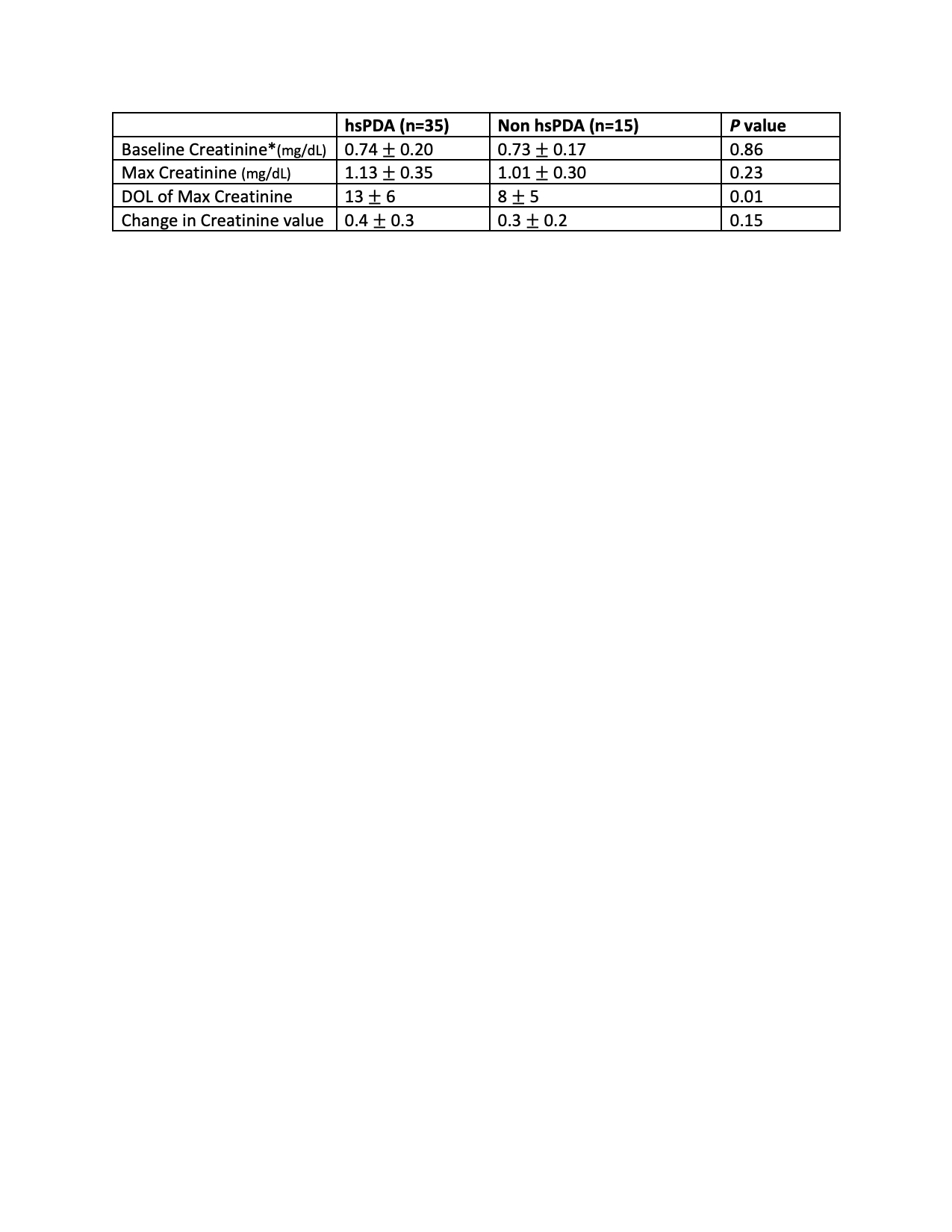 *Baseline Creatinine defined by lowest SCr after DOL1, prior to any subsequent increase in SCr
*Baseline Creatinine defined by lowest SCr after DOL1, prior to any subsequent increase in SCr
Objective: To investigate renal saturation (RSat) as measured by NIRS for detection of AKI in neonates with a PDA.
Design/Methods: This single-center retrospective study investigated clinical, ECHO, and NIRS characteristics of 50 preterm infants ≤29 weeks gestation who underwent routine NIRS monitoring and ECHO due to concern for PDA. A PDA was classified as hemodynamically significant if two of the following were found on ECHO: moderate to large size, left-to-right shunting, descending aorta flow reversal, or left atrial enlargement. AKI was defined by neonatal Kidney Disease: Improving Global Outcomes [KDIGO] criteria. Only AKI occurring three days before until ten days after ECHO qualified in this study. Cerebral and renal saturations were evaluated for the 24 hour period prior to ECHO. Student t-test or Fisher’s exact test compared characteristics between groups. Logistic regression assessed the association between NIRS and AKI.
Results: Among 50 infants, hsPDA was found on ECHO in 35 infants (70%). Of infants with hsPDA, 15 (43%) developed AKI compared to 3 (20%) without hsPDA. No significant differences in demographics or PDA management were found in those with AKI versus no AKI (Table 1), however infants with AKI were less likely to be on dopamine on day of ECHO (p=0.04). RSat was not significantly associated with AKI (p=0.4) or hsPDA (p=0.2) (Table 3). Although dopamine use was not associated with SCr or RSat levels, infants on dopamine had significantly less variability in RSat (p=0.002). Infants with hsPDA had lower cerebral saturations than those without hsPDA (68% versus 74%, p=0.02) (Table 3).Conclusion(s): Renal NIRS measurements did not discriminate AKI in the preterm hsPDA population, however our data may not capture the optimal timing of measurement prior to AKI occurrence. Future research into the utility of NIRS monitoring and effect of dopamine on renal oxygenation is needed to better characterize the infant at high risk of AKI.
Neonatal Characteristics
.jpg) Value are mean +/- SD or n (%); *on date of ECHO; +on date of NIRS
Value are mean +/- SD or n (%); *on date of ECHO; +on date of NIRSCreatinine trends
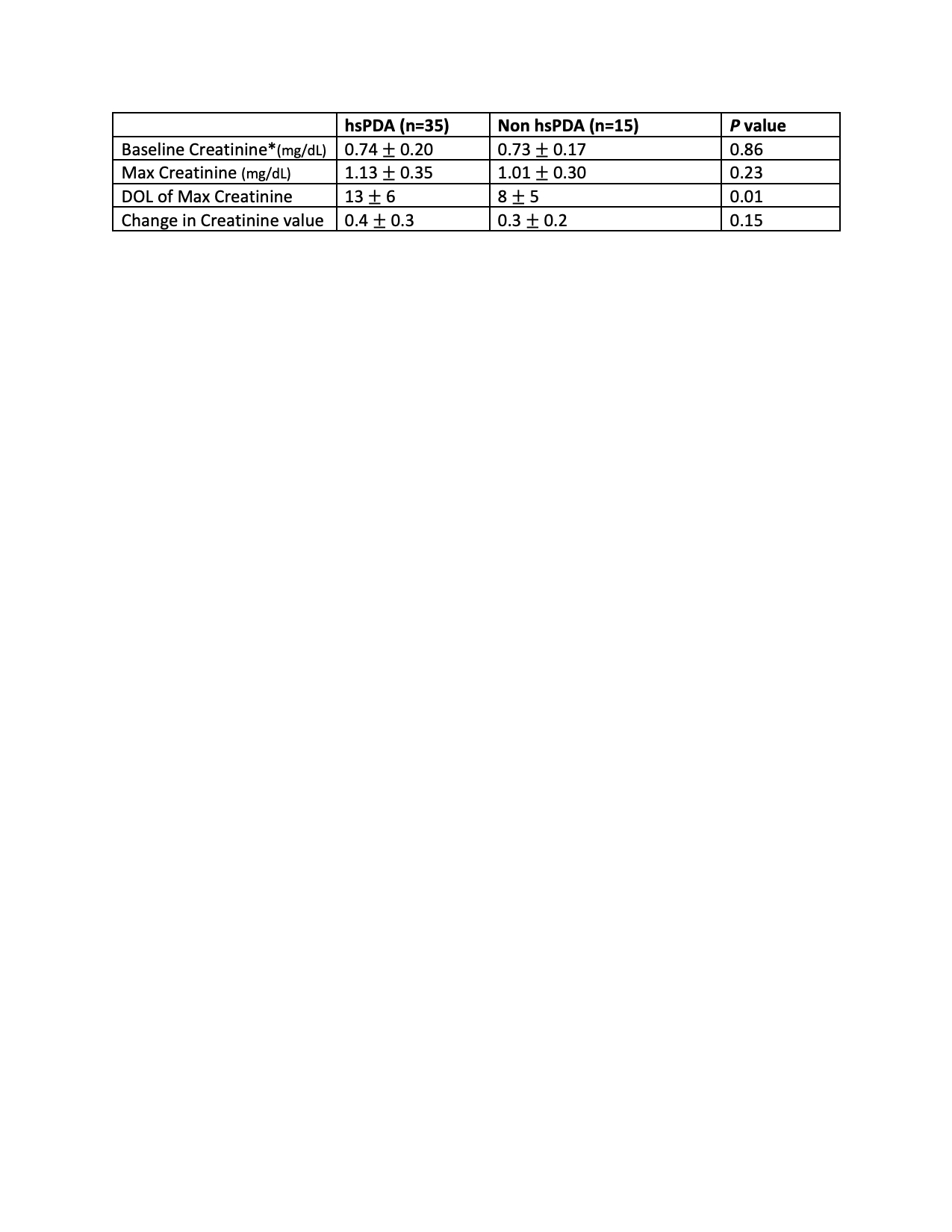 *Baseline Creatinine defined by lowest SCr after DOL1, prior to any subsequent increase in SCr
*Baseline Creatinine defined by lowest SCr after DOL1, prior to any subsequent increase in SCr