Neonatal Hematology & Bilirubin Metabolism
Category: Abstract Submission
Neonatal Hematology & Bilirubin Metabolism I
342 - Reticulocyte Hemoglobin as an Early Predictor of Impending Anemia in a Nonhuman Primate Model of Infantile Iron Deficiency Anemia
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 342
Publication Number: 342.122
Publication Number: 342.122
Kathleen Ennis-Czerniak, University of Minnesota, Minneapolis, MN, United States; gabriele Lubach, University of Wisconsin, Madison, WI, United States; Eric Lock, University of Minnesota, Minneapolis, MN, United States; Pamela J. Kling, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Michael K. Georgieff, University of Minnesota, Minneapolis, MN, United States; Christopher L. Coe, University of Wisconsin, Madison, WI, United States; Raghavendra Rao, University of Minnesota Medical School, Minneapolis, MN, United States
- KE
Kathleen M. Ennis-Czerniak, BA
Researcher
University of Minnesota
Woodbury, Minnesota, United States
Presenting Author(s)
Background: Iron deficiency (ID) in infancy is a risk for long-term neurobehavioral deficits. Currently, infantile ID is screened for by low hemoglobin (Hgb) at 9-12 months. But, due to prioritization of iron to RBCs, anemia is the end stage of ID. Brain ID precedes the onset of anemia. Treatment once becoming anemic fails to reverse all ID-induced neurological deficits. Reticulocyte Hgb content (Ret-He) reflects iron availability for RBC production and predates anemia. Lower Ret-He is a biomarker of ID and correlates with the onset of brain ID in a rat model of early postnatal ID.
Objective: Determine whether Ret-He is a biomarker of impending anemia in a nonhuman primate model of human infantile ID.
Design/Methods: Iron indices (serum iron, transferrin saturation [TSAT], total and unsaturated iron-binding capacity), RBC indices (Hgb, Ret-He, mean corpuscular volume, mean corpuscular Hgb, mean corpuscular Hgb concentration and RBC distribution width) and growth parameters (weight, length, head circumference and rate of weight gain) were serially determined at 2 weeks, 2, 4, and 6 months in rhesus monkey infants and their mothers (n=54). The relationships between iron, RBC and growth parameters and risk of ID (TSAT < 20%) and anemia (Hgb < 10 g/dL) were determined.
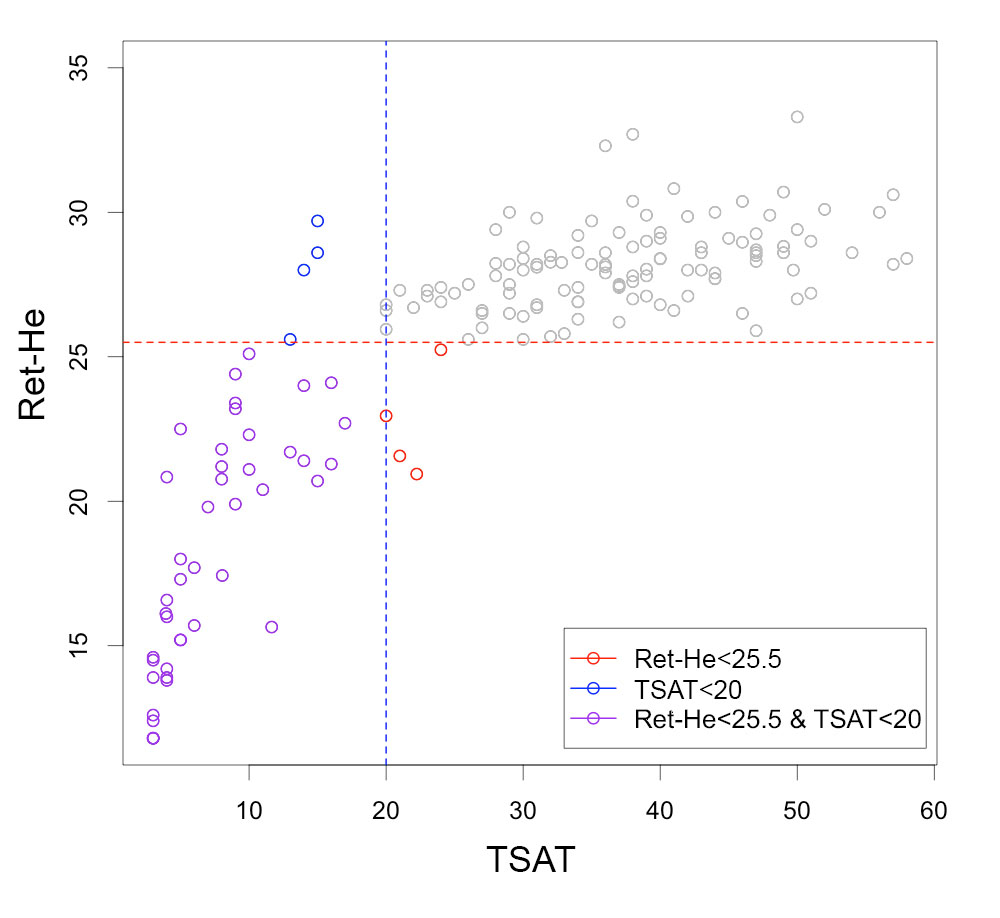
Results: Thirty infants (56%) became ID and 16 infants (30%) developed anemia. ID and anemic infants gained weight faster than unaffected infants until 2 months of age (Fig. 1). Ret-He correlated with TSAT. A Ret-He < 25.5 correctly predicted impending anemia in 12/16 (75%) infants and falsely predicted anemia in 4/38 (10%) unaffected infants (Fig. 2). Ret-He and TSAT differed earlier than the other iron indices in infants developing anemia. Lower Ret-He was the only RBC index that predicted impending anemia (Fig. 3). There was no association between maternal and infant RBC and iron indices.Conclusion(s): In this naturalistic model of infantile ID, rapid postnatal weight gain predisposed to ID and anemia. Ret-He was a more sensitive early biomarker of anemia than other RBC indices and had a similar predictive specificity as TSAT. Ret-He is a component of the CBC panel in commonly used hematology analyzers and provides a hematology-based diagnostic approach that is cost effective and appealing to detect early ID.
Fig 1. Body weight of infants developing iron deficiency anemia and those that remained unaffected. Values are mean +/- SEM (n=16 anemic and n=38 non-anemic); *p < 0.05 vs. age-matched IS.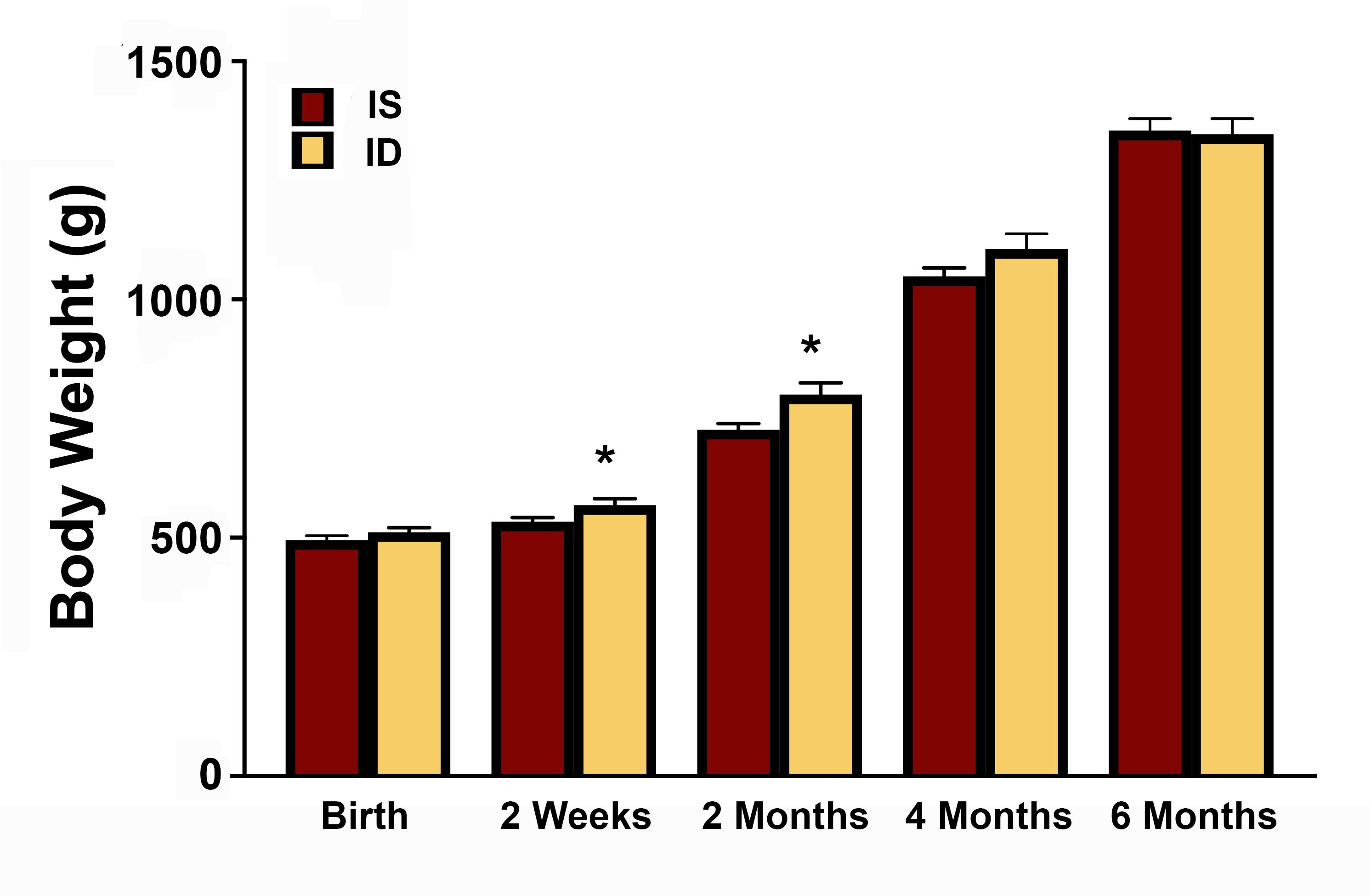
Fig 2. Relationship between Ret-He and transferrin saturation (TSAT) in the cohort (n=54)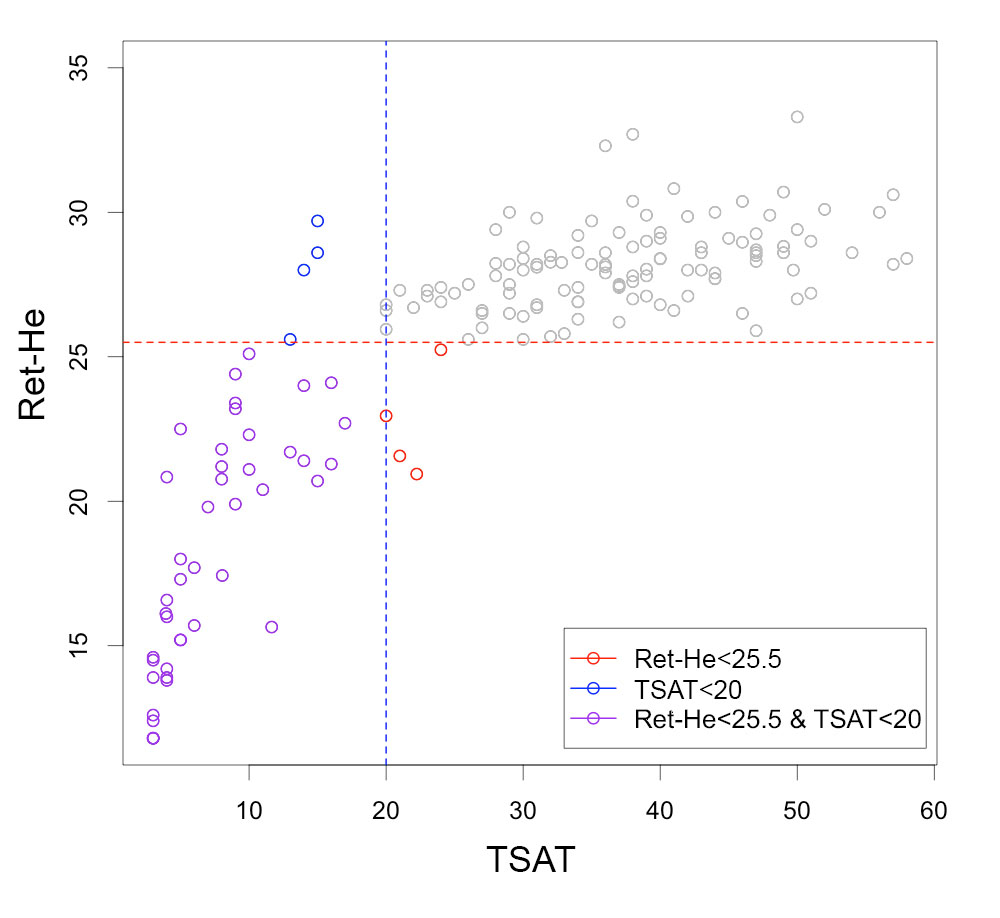
Objective: Determine whether Ret-He is a biomarker of impending anemia in a nonhuman primate model of human infantile ID.
Design/Methods: Iron indices (serum iron, transferrin saturation [TSAT], total and unsaturated iron-binding capacity), RBC indices (Hgb, Ret-He, mean corpuscular volume, mean corpuscular Hgb, mean corpuscular Hgb concentration and RBC distribution width) and growth parameters (weight, length, head circumference and rate of weight gain) were serially determined at 2 weeks, 2, 4, and 6 months in rhesus monkey infants and their mothers (n=54). The relationships between iron, RBC and growth parameters and risk of ID (TSAT < 20%) and anemia (Hgb < 10 g/dL) were determined.
Results: Thirty infants (56%) became ID and 16 infants (30%) developed anemia. ID and anemic infants gained weight faster than unaffected infants until 2 months of age (Fig. 1). Ret-He correlated with TSAT. A Ret-He < 25.5 correctly predicted impending anemia in 12/16 (75%) infants and falsely predicted anemia in 4/38 (10%) unaffected infants (Fig. 2). Ret-He and TSAT differed earlier than the other iron indices in infants developing anemia. Lower Ret-He was the only RBC index that predicted impending anemia (Fig. 3). There was no association between maternal and infant RBC and iron indices.Conclusion(s): In this naturalistic model of infantile ID, rapid postnatal weight gain predisposed to ID and anemia. Ret-He was a more sensitive early biomarker of anemia than other RBC indices and had a similar predictive specificity as TSAT. Ret-He is a component of the CBC panel in commonly used hematology analyzers and provides a hematology-based diagnostic approach that is cost effective and appealing to detect early ID.
Fig 1. Body weight of infants developing iron deficiency anemia and those that remained unaffected. Values are mean +/- SEM (n=16 anemic and n=38 non-anemic); *p < 0.05 vs. age-matched IS.
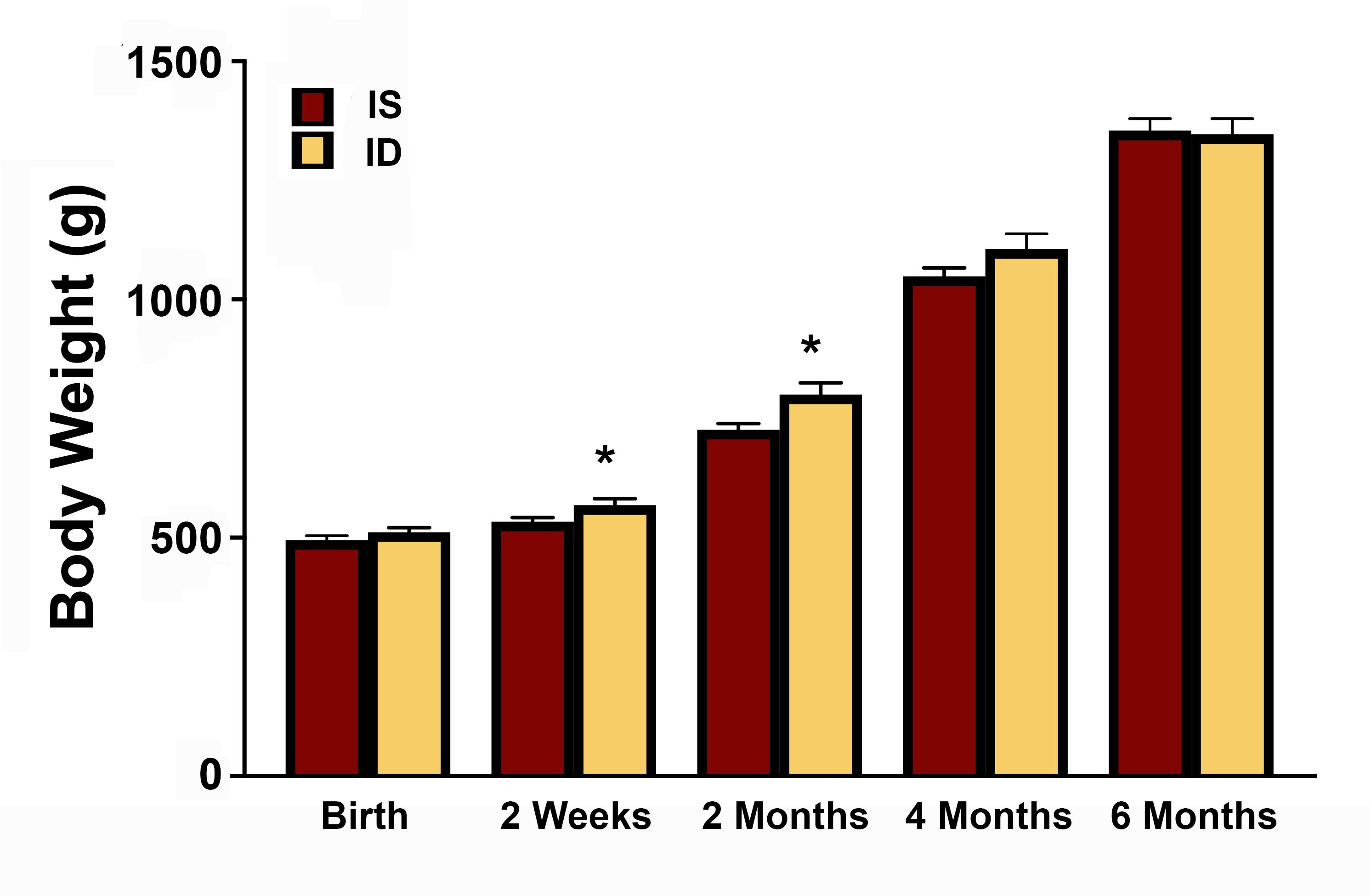
Fig 2. Relationship between Ret-He and transferrin saturation (TSAT) in the cohort (n=54)