Hematology/Oncology
Category: Abstract Submission
Hematology/Oncology I
330 - Role of Steroids in Sickle Cell Patients with Acute Chest Syndrome
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 330
Publication Number: 330.113
Publication Number: 330.113
Kokila Jeyamurugan, Brookdale Hospital Medical Center, Brooklyn, NY, United States; Min-Kyung Jung, New York Institute of Technology College of Osteopathic Medicine, Oakland Gardens, NY, United States; Fernanda E. Kupferman, One Brookdale Health at Brookdale Hospital Medical Center, Brooklyn, NY, United States; Kusum Viswanathan, One Brooklyn Health, Brooklyn, NY, United States

Kokila Jeyamurugan, MD
Resident
Brookdale Hospital Medical Center
Brooklyn, New York, United States
Presenting Author(s)
Background: The role of corticosteroids to treat Acute Chest Syndrome (ACS) in patients with Sickle cell disease (SCD) has always been a matter of debate. In clinical practice, systemic steroids were given for ACS with more severe disease. With lack of standard treatment guidelines, their use to treat ACS is highly physician dependent and varies widely across different hospitals. The utility of corticosteroids in ACS still remains unclear.
Objective: To describe the differences between SCD patients treated with corticosteroids for ACS and those who were not and to evaluate the association between corticosteroid use, length of stay and readmission rates.
Design/Methods: This is a retrospective chart review of patients with SCD ≤ 18 years of age hospitalized for ACS between January 2016 and May 2021; Patients were organized into 2 groups based on corticosteroid use to treat ACS. Children with immunodeficiency, positive blood culture and on inhalational corticosteroids were excluded. Outcome variables included length of hospital stay (LOS), duration of oxygen requirement and iv pain medications, blood transfusions, ICU admission requiring respiratory support and readmission within 14 days of discharge for sickle crisis. To test the differences between patients treated with corticosteroids for ACS and those who were not, Mann-Whitney U test was used for continuous outcome variables and chi-square test for categorical outcome variables.
Results: We identified 43 patients with 60 episodes of ACS (mean age 11 years, 55% males). Corticosteroids were used in 32 episodes, while bronchodilators were used in 47. The median LOS was 6 days. Patients were readmitted within 14 days after 7 episodes (11.7%). Corticosteroid use was associated with a significant increase in length of stay (p = 0.07). The need for blood transfusions, ICU admission with respiratory support, and a chest x-ray finding with > 1 lobe involvement all point to moderate or severe ACS, which has been linked to steroid use. In patients with asthma, the length of stay was not statistically significant between the groups (p = 0.44).Conclusion(s): Overall, our data show that treatment with systemic steroids for ACS is associated with more severe disease. The use of steroids remains associated with an increased length of stay among pediatric patients with ACS. Corticosteroids were not associated with a higher readmission rate in our study population; even in patients with ACS with comorbid asthma.
kj resume recent.pdf
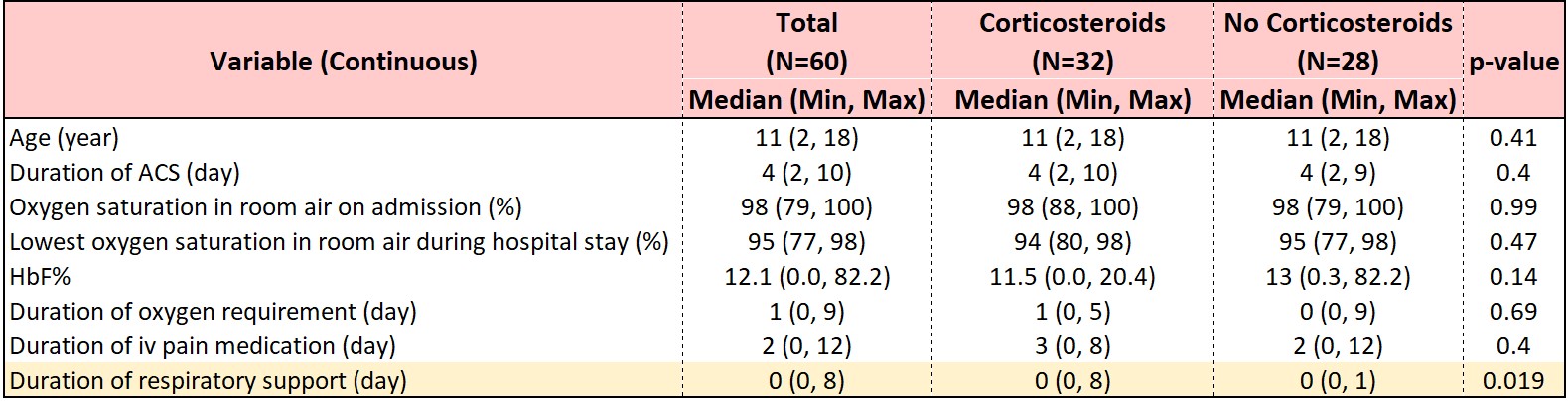
Descriptive Statistics of continuous variables by Corticosteroid treatment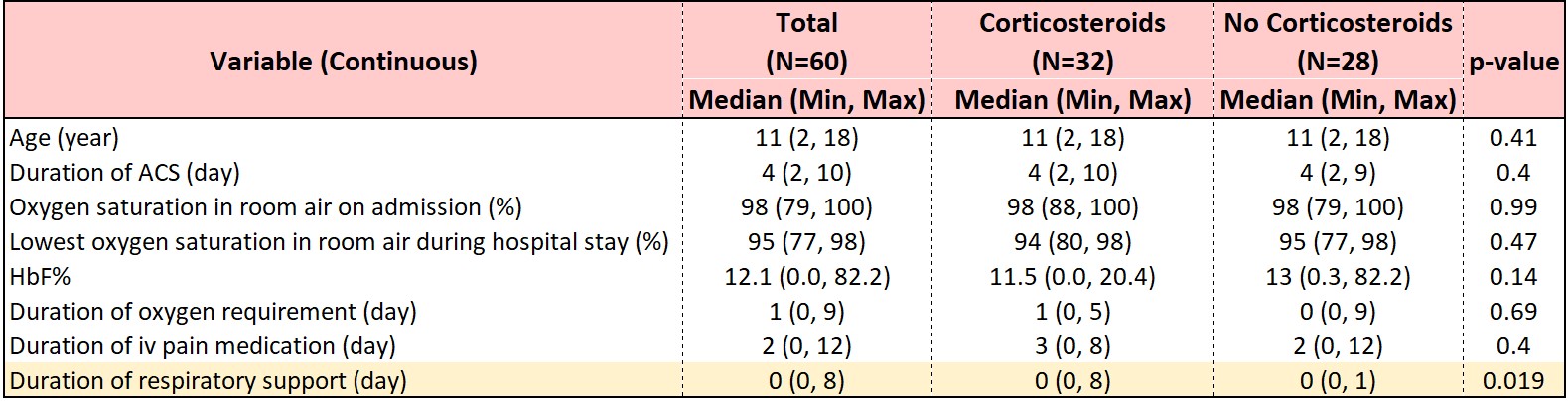
Objective: To describe the differences between SCD patients treated with corticosteroids for ACS and those who were not and to evaluate the association between corticosteroid use, length of stay and readmission rates.
Design/Methods: This is a retrospective chart review of patients with SCD ≤ 18 years of age hospitalized for ACS between January 2016 and May 2021; Patients were organized into 2 groups based on corticosteroid use to treat ACS. Children with immunodeficiency, positive blood culture and on inhalational corticosteroids were excluded. Outcome variables included length of hospital stay (LOS), duration of oxygen requirement and iv pain medications, blood transfusions, ICU admission requiring respiratory support and readmission within 14 days of discharge for sickle crisis. To test the differences between patients treated with corticosteroids for ACS and those who were not, Mann-Whitney U test was used for continuous outcome variables and chi-square test for categorical outcome variables.
Results: We identified 43 patients with 60 episodes of ACS (mean age 11 years, 55% males). Corticosteroids were used in 32 episodes, while bronchodilators were used in 47. The median LOS was 6 days. Patients were readmitted within 14 days after 7 episodes (11.7%). Corticosteroid use was associated with a significant increase in length of stay (p = 0.07). The need for blood transfusions, ICU admission with respiratory support, and a chest x-ray finding with > 1 lobe involvement all point to moderate or severe ACS, which has been linked to steroid use. In patients with asthma, the length of stay was not statistically significant between the groups (p = 0.44).Conclusion(s): Overall, our data show that treatment with systemic steroids for ACS is associated with more severe disease. The use of steroids remains associated with an increased length of stay among pediatric patients with ACS. Corticosteroids were not associated with a higher readmission rate in our study population; even in patients with ACS with comorbid asthma.
kj resume recent.pdf
Descriptive Statistics of continuous variables by Corticosteroid treatment