Emergency Medicine: All Areas
Category: Abstract Submission
4: Emergency Medicine I
41 - National Trends in the Use of Psychotropic Medications in Pediatric Mental Health Emergency Department Visits Between 2006 and 2019
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 41
Publication Number: 41.103
Publication Number: 41.103
Katherine A. Nash, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Mark Olfson, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Craig Rothenberg, Yale School of Medicine, New Haven, CT, United States; Brett R. Anderson, Columbia University Medical Center, New York, NY, United States; Arjun Venkatesh, Yale School of Medicine, New Haven, CT, United States; Harold Pincus, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States

Katherine Nash, MD, MHS (she/her/hers)
Assistant Professor
Columbia University Vagelos College of Physicians and Surgeons
New York, New York, United States
Presenting Author(s)
Background: An increasing number of youths present to the emergency department (ED) for mental and behavioral health (MBH) care. Treatment of MBH crises often involves psychotropic medications, however, little is known about use during pediatric MBH ED visits.
Objective: Describe psychotropic medication use in a United States nationally representative sample of pediatric MBH ED visits over a 14-year period and examine associations between psychotropic medication use and sociodemographic characteristics.
Design/Methods: We analyzed pediatric (6-17 years) MBH ED visits, using the 2006-2019 National Hospital Ambulatory Medical Care Surveys. MBH visits were identified by ICD-9/10 codes. Medications used in the ED were characterized as psychotropic by Multum’s classification system and prior literature. We described psychotropic use over time, by medication type and sociodemographic characteristics (race and ethnicity, payer type, age, and sex). We used survey weighted logistic regression to examine relationships between psychotropic medication use and sociodemographic characteristics, adjusting for arrival time, geographic region, and disposition type.
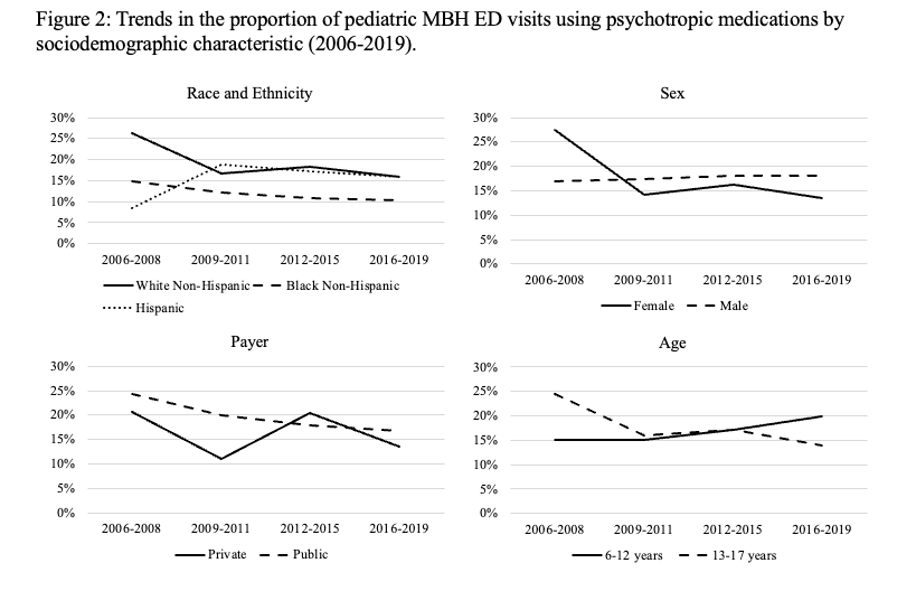
Results: Our sample represents 11,792,860 pediatric MBH ED visits, 2006-2019. Psychotropic medications were used in 17.2% of visits. Anxiolytics were most frequently used (10.6% of visits), followed by antipsychotics (4.7%), antihistamines (4.8%), and antidepressants (3.3%). The proportion of MBH ED visits using psychotropic medications decreased from 22.4% in 2006-2008 to 15.8% in 2009-2011, and then remained stable (15.6% in 2016-2019; Figure 1). Use of anxiolytics, antipsychotics, and antidepressants decreased over time, while use of antihistamines did not change (Figure 1). Psychotropic medication use decreased as a proportion of visits for most sociodemographic groups, however, increased for Hispanic patients (8.5% in 2006-2008 to 15.9% in 2016-2019) and younger patients (15.0% in 2006-2008 to 13.9% in 2016-2019) (Figure 2). In the most recent years, Black non-Hispanic patients had a 66% decreased odds of psychotropic medication use vs White non-Hispanic patients (aOr 0.44, 95% CI 0.19-0.99; Table 1). Conclusion(s): Psychotropic medication use in pediatric MBH ED visits decreased in the late 2000s but stabilized in the 2010s. Most recently 1 of 6 visits used a psychotropic medication. Given known adverse drug effects and observed differences in prescribing by sociodemographics, pharmacologic management of MBH crises warrants further surveillance for appropriateness, safety, efficacy, and equity of use.
Figure 1: Trends in the proportion of pediatric MBH ED visits using psychotropic medications overall, and by medication type (2006-2019).png)
Figure 2: Trends in the proportion of pediatric MBH ED visits using psychotropic medications by sociodemographic characteristic (2006-2019)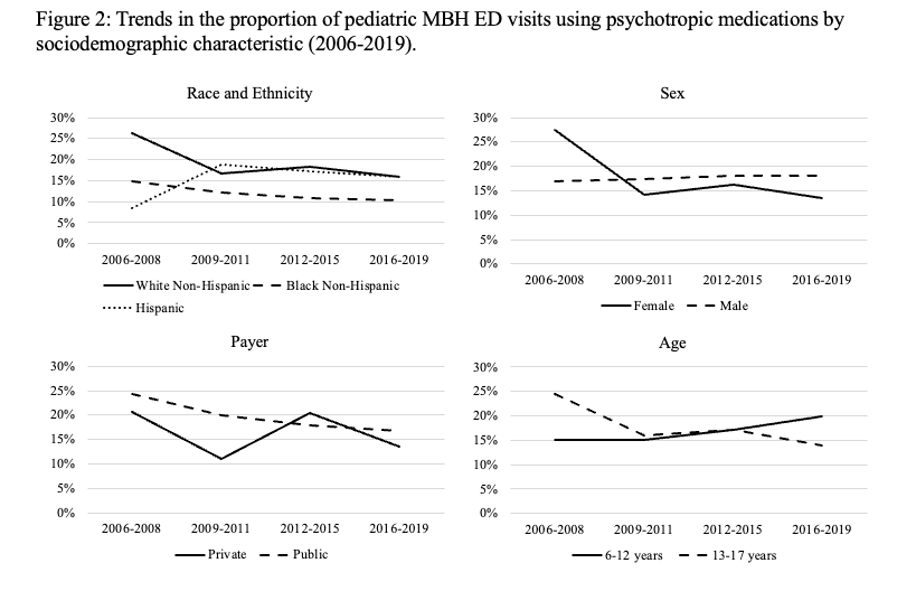
Objective: Describe psychotropic medication use in a United States nationally representative sample of pediatric MBH ED visits over a 14-year period and examine associations between psychotropic medication use and sociodemographic characteristics.
Design/Methods: We analyzed pediatric (6-17 years) MBH ED visits, using the 2006-2019 National Hospital Ambulatory Medical Care Surveys. MBH visits were identified by ICD-9/10 codes. Medications used in the ED were characterized as psychotropic by Multum’s classification system and prior literature. We described psychotropic use over time, by medication type and sociodemographic characteristics (race and ethnicity, payer type, age, and sex). We used survey weighted logistic regression to examine relationships between psychotropic medication use and sociodemographic characteristics, adjusting for arrival time, geographic region, and disposition type.
Results: Our sample represents 11,792,860 pediatric MBH ED visits, 2006-2019. Psychotropic medications were used in 17.2% of visits. Anxiolytics were most frequently used (10.6% of visits), followed by antipsychotics (4.7%), antihistamines (4.8%), and antidepressants (3.3%). The proportion of MBH ED visits using psychotropic medications decreased from 22.4% in 2006-2008 to 15.8% in 2009-2011, and then remained stable (15.6% in 2016-2019; Figure 1). Use of anxiolytics, antipsychotics, and antidepressants decreased over time, while use of antihistamines did not change (Figure 1). Psychotropic medication use decreased as a proportion of visits for most sociodemographic groups, however, increased for Hispanic patients (8.5% in 2006-2008 to 15.9% in 2016-2019) and younger patients (15.0% in 2006-2008 to 13.9% in 2016-2019) (Figure 2). In the most recent years, Black non-Hispanic patients had a 66% decreased odds of psychotropic medication use vs White non-Hispanic patients (aOr 0.44, 95% CI 0.19-0.99; Table 1). Conclusion(s): Psychotropic medication use in pediatric MBH ED visits decreased in the late 2000s but stabilized in the 2010s. Most recently 1 of 6 visits used a psychotropic medication. Given known adverse drug effects and observed differences in prescribing by sociodemographics, pharmacologic management of MBH crises warrants further surveillance for appropriateness, safety, efficacy, and equity of use.
Figure 1: Trends in the proportion of pediatric MBH ED visits using psychotropic medications overall, and by medication type (2006-2019)
.png)
Figure 2: Trends in the proportion of pediatric MBH ED visits using psychotropic medications by sociodemographic characteristic (2006-2019)