Medical Education: Fellow
Category: Abstract Submission
Medical Education 3 - Medical Education: Fellow I
580 - Facilitators and barriers to using entrustable professional activities in pediatric fellowships
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 580
Publication Number: 580.117
Publication Number: 580.117
Angela S. Czaja, University of Colorado School of Medicine, Aurora, CO, United States; Richard Mink, The Lundquist Institute for Biomedical Innovation, Torrance, CA, United States; David A. Turner, American Board of Pediatrics, Chapel Hill, NC, United States; Megan L. Curran, University of Colorado School of Medicine, Aurora, CO, United States; Bruce E. Herman, University of Utah Department of Pediatrics, Salt Lake City, UT, United States; Angela L. Myers, Children's Mercy Kansas City, Kansas City, MO, United States; Diane E. Stafford, Stanford University/Lucile Packard Children's Hospital, Palo Alto, CA, United States; Pnina Weiss, Yale School of Medicine, New Haven, CT, United States; Melissa L. Langhan, Yale University School of Medicine, New Haven, CT, United States
Angela S. Czaja, MD PhD (she/her/hers)
Associate Professor
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Entrustable Professional Activities (EPAs) have been developed for pediatric subspecialties but are not uniformly used in pediatric fellowships. The American Board of Pediatrics intends to require EPA-based assessments in the near future as a part of initial certification. Understanding fellowship program directors’ (FPDs) perspectives will be essential for successful and meaningful implementation of assessment using EPAs.
Objective: To understand pediatric FPDs’ current use of EPAs and their perspectives on potential facilitators and barriers to EPA use.
Design/Methods: A qualitative study was performed from Nov 2019 to Sept 2020 using purposeful and snowball sampling of FPDs who self-identified as current EPA users or non-users. Semi-structured interviews were conducted using a guide with open-ended questions and prompts to explore current EPA use or non-use and the factors supporting or preventing their use. Interviews were audio-recorded and professionally transcribed. Educators from the research team independently coded the transcripts after inductive coding training. Group discussion and consensus informed code structure development and refinement. Iterative data collection and analysis continued until theoretical sufficiency was achieved.
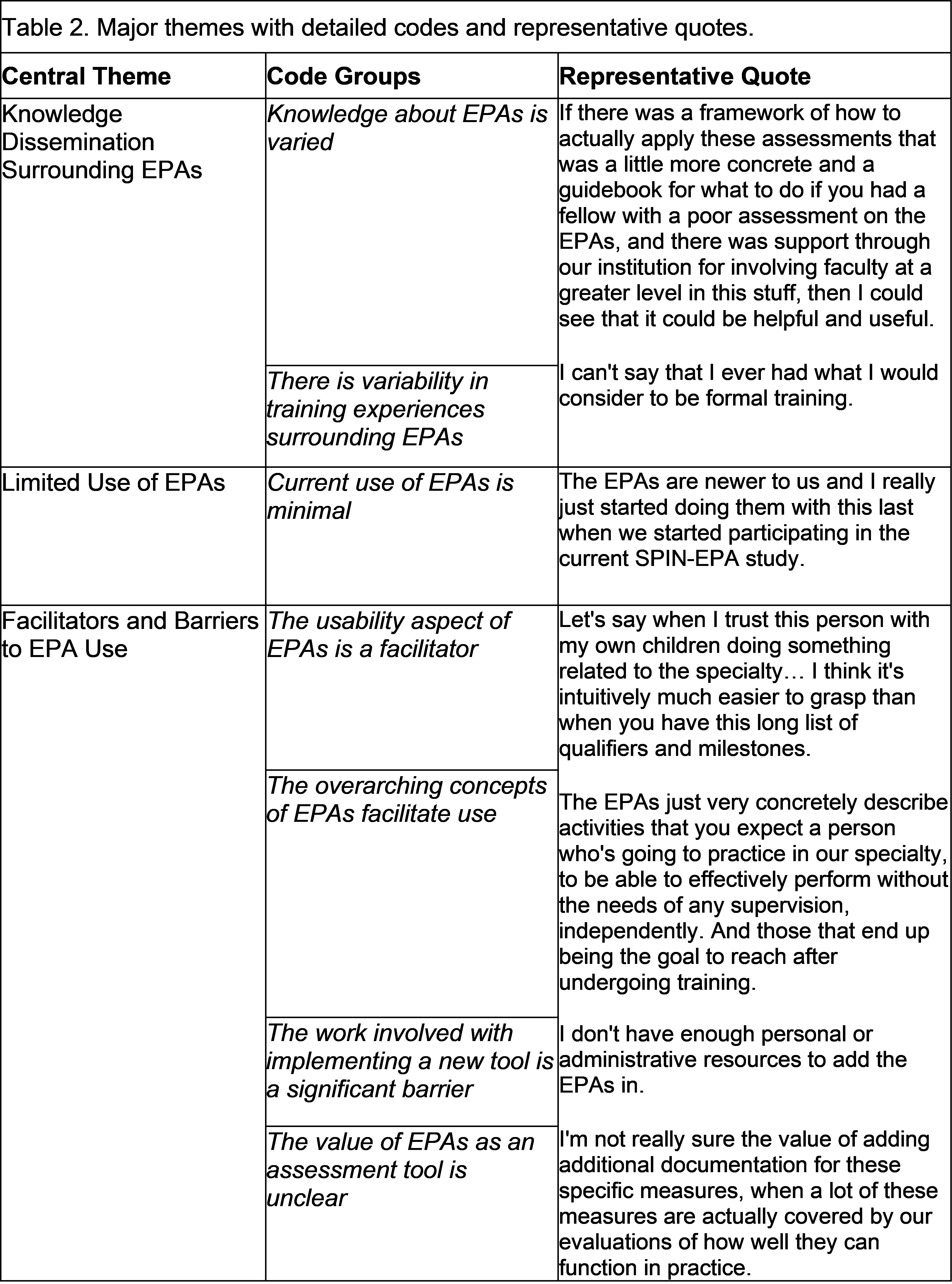
Results: 28 FPDs representing 11 pediatric subspecialties were interviewed, of whom 16 (57%) reported current EPA use. (Table 1) Four major themes emerged from the analysis (Table 2): (1) Variable knowledge and training surrounding EPAs, leading to differing levels of understanding; (2) limited current use of EPAs, even among self-reported users, some of whom only use EPAs as a part of research studies; (3) facilitators and barriers to use. Although FPDs recognize the intuitive nature and simple wording of EPAs, they also report workload burden and lack of a regulatory requirement as barriers to their use; and (4) complementary nature of EPAs and milestones. FPDs acknowledged the differing strengths each assessment tool provides but sought additional knowledge about the value added through EPAs, including impact on outcomes.Conclusion(s): The intuitive and straightforward nature of EPAs may facilitate their use in pediatric fellowship programs. However, effective implementation into the current assessment system requires a thoughtful approach to addressing barriers, such as additional workload and limited knowledge and understanding of EPAs and their perceived value. This will require significant engagement with, and education of, program directors.
Table 1. Fellowship Program Director Participants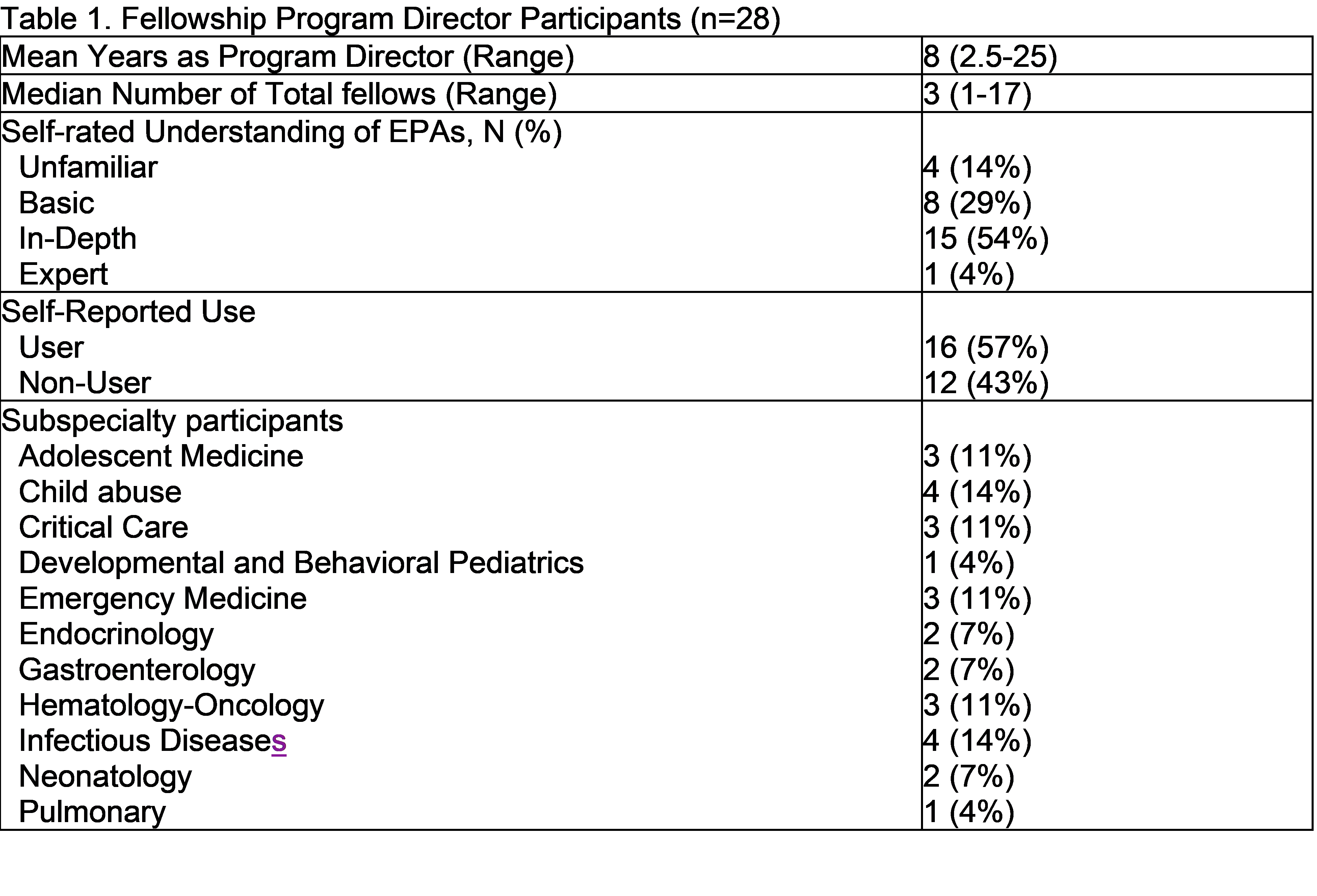
Table 2. Major themes with detailed codes and representative quotes.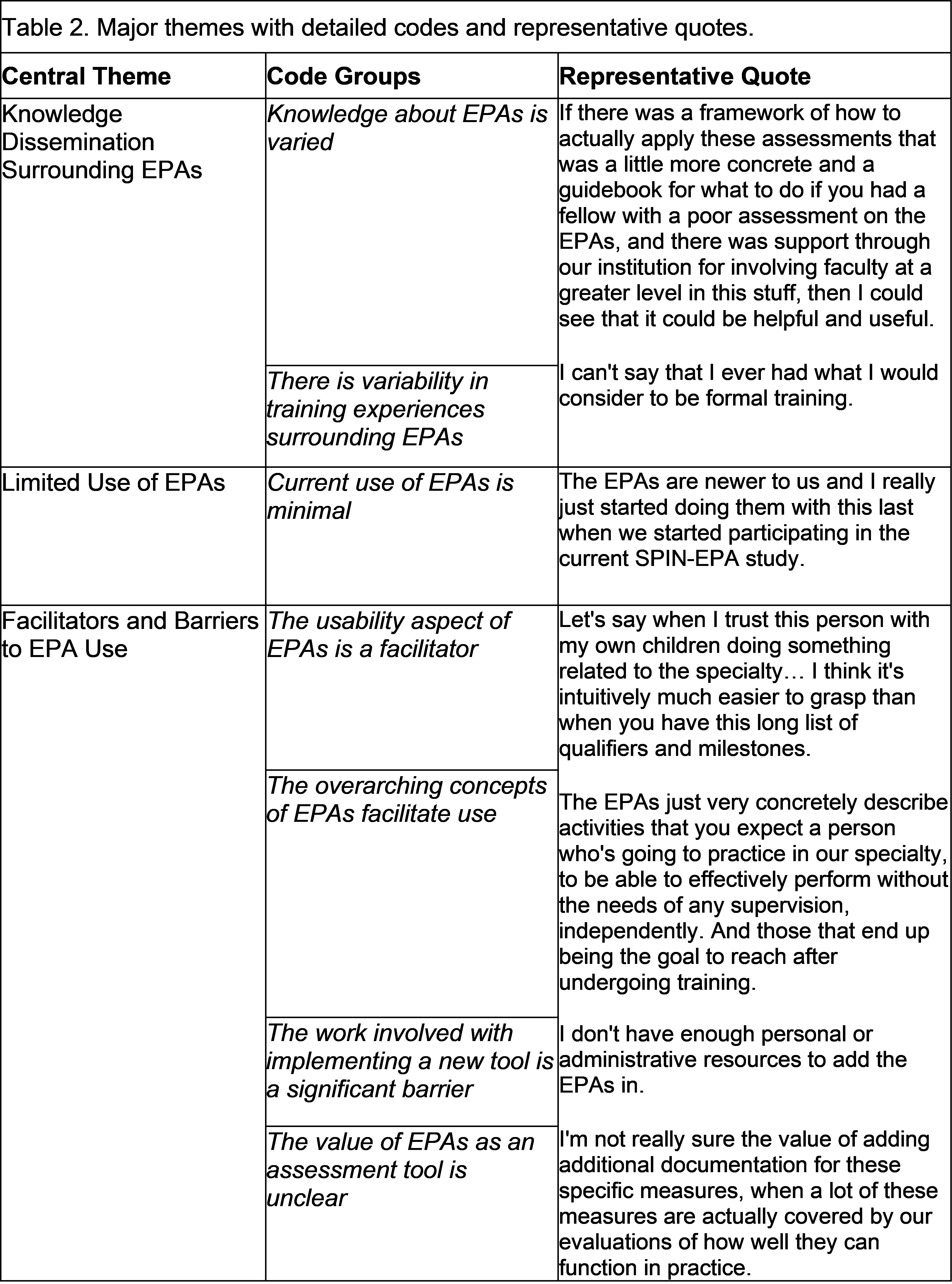
Objective: To understand pediatric FPDs’ current use of EPAs and their perspectives on potential facilitators and barriers to EPA use.
Design/Methods: A qualitative study was performed from Nov 2019 to Sept 2020 using purposeful and snowball sampling of FPDs who self-identified as current EPA users or non-users. Semi-structured interviews were conducted using a guide with open-ended questions and prompts to explore current EPA use or non-use and the factors supporting or preventing their use. Interviews were audio-recorded and professionally transcribed. Educators from the research team independently coded the transcripts after inductive coding training. Group discussion and consensus informed code structure development and refinement. Iterative data collection and analysis continued until theoretical sufficiency was achieved.
Results: 28 FPDs representing 11 pediatric subspecialties were interviewed, of whom 16 (57%) reported current EPA use. (Table 1) Four major themes emerged from the analysis (Table 2): (1) Variable knowledge and training surrounding EPAs, leading to differing levels of understanding; (2) limited current use of EPAs, even among self-reported users, some of whom only use EPAs as a part of research studies; (3) facilitators and barriers to use. Although FPDs recognize the intuitive nature and simple wording of EPAs, they also report workload burden and lack of a regulatory requirement as barriers to their use; and (4) complementary nature of EPAs and milestones. FPDs acknowledged the differing strengths each assessment tool provides but sought additional knowledge about the value added through EPAs, including impact on outcomes.Conclusion(s): The intuitive and straightforward nature of EPAs may facilitate their use in pediatric fellowship programs. However, effective implementation into the current assessment system requires a thoughtful approach to addressing barriers, such as additional workload and limited knowledge and understanding of EPAs and their perceived value. This will require significant engagement with, and education of, program directors.
Table 1. Fellowship Program Director Participants
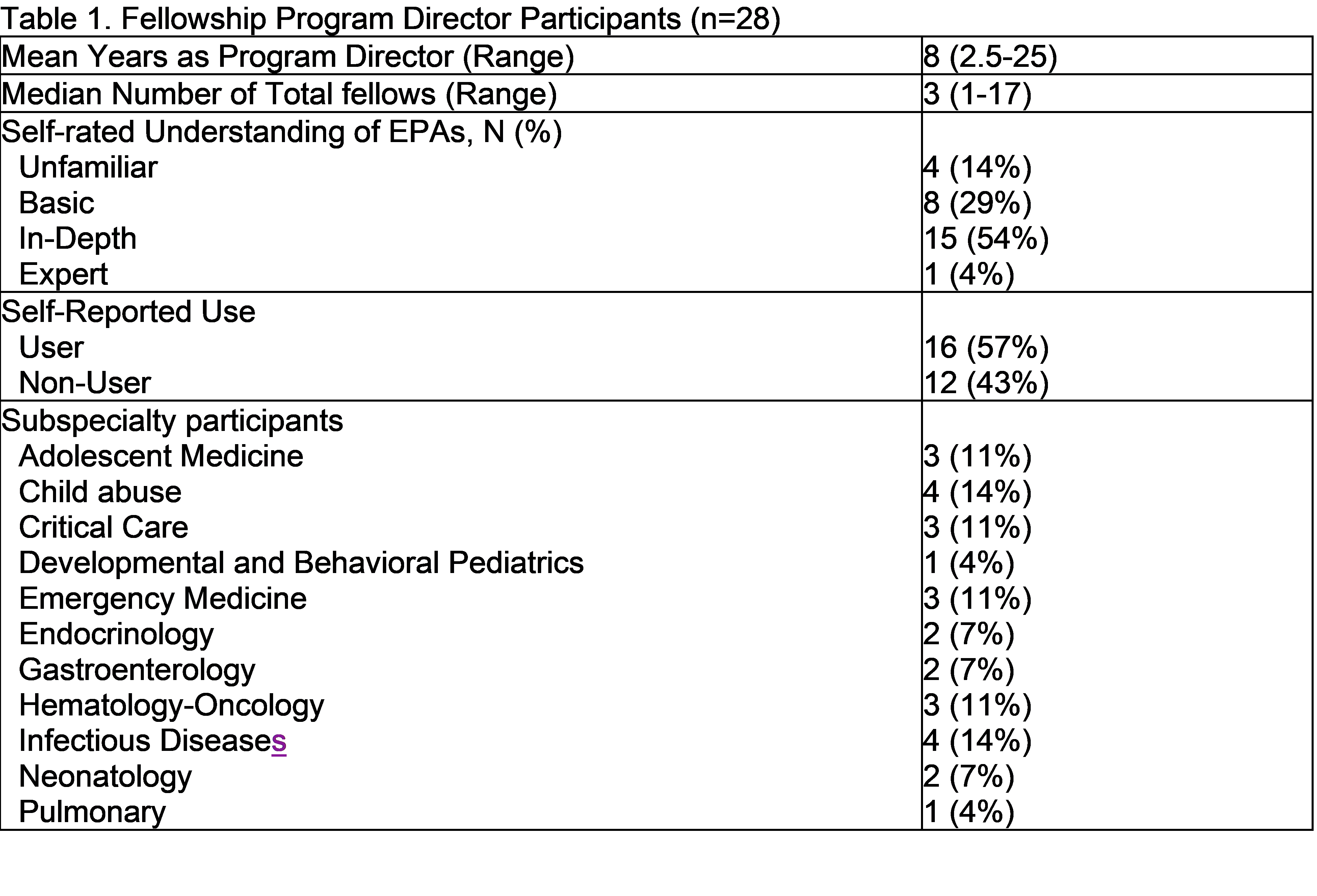
Table 2. Major themes with detailed codes and representative quotes.