Environmental Health
Category: Abstract Submission
Environmental Health I
121 - Are Massachusetts Health Professionals Counseling Patients About Environmental Health Concerns?
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 121
Publication Number: 121.108
Publication Number: 121.108
Alan D. Woolf, Boston Children's Hospital, Boston, MA, United States; Marissa Hauptman, Boston Children's Hospital, Boston, MA, United States; Mary Susan L. Howlett, University of Massachusetts Boston, North Andover, MA, United States; Shalini H. Shah, Boston Children's Hospital, Boston, MA, United States; Mary Mortensen, Mortensen LLC, atlanta, GA, United States; Blair J. Wylie, Beth Israel Deaconess Medical Center, Brookline, MA, United States; Marc Nascarella, Massachusetts Department of Public Health, Boston, MA, United States

Alan D. Woolf, MD, MPH (he/him/his)
Associate Chief Medical Education Officer
Harvard Medical School
Boston, Massachusetts, United States
Presenting Author(s)
Background: Medical societies promote prevention counseling by health care professionals during routine care. Such counseling should include measures to ensure a safe, healthful physical environment. As an important part of their role as counselors, health care providers must feel confident in their own expertise regarding environmental health (EH) issues.
Objective: Assess educational interest and awareness of EH among actively practicing health care providers, and evaluate current preferences for consuming EH-related educational content.
Design/Methods: A 35-item instrument covering EH issues was created, pretested to ensure items were clearly articulated and response items were relevant, and modified. The finalized Internet-based survey was sent during January-April 2021 to a convenience sample of Massachusetts health care providers, of whom 362 returned completed surveys. Of these, 20% self-identified as pediatric or family practice care providers, respectively; 72% of respondents were nurses and/or nurse practitioners.
Results: Although clinicians recognized the importance of environmental exposures and their health impacts, 34% had not asked patients about such exposures in the previous year; only 7% endorsed receiving any previous training on how to counsel patients on environmental exposures. Health care professionals cited time pressure and limited knowledge as the top barriers to such discussions. While they felt knowledgeable when counseling on personal behavior exposures (e.g. smoking, vaping, or marijuana use), the safety of food and water from contamination by chemicals (e.g. perfluoroalkyl substances, metals) were among the least familiar and least discussed topics. (Figure 1) Other knowledge gaps included pesticides, indoor air pollutants, and hazards posed by household and personal care products. For those who sought out EH-related resources, 60% consulted government websites, 51% proprietary medical information websites, 49% professional literature, 46% professional society position statements, and 37% state/local health department resources. Clinicians preferred tip sheets, on-demand or pre-recorded materials, and online toolkits rather than live (in-person or virtual) trainings. Conclusion(s): These results can inform future plans for educational outreach to health care professionals regarding EH topics important to discuss during primary care.
Figure 1. Percentage of clinicians discussing versus unfamiliar with specific exposures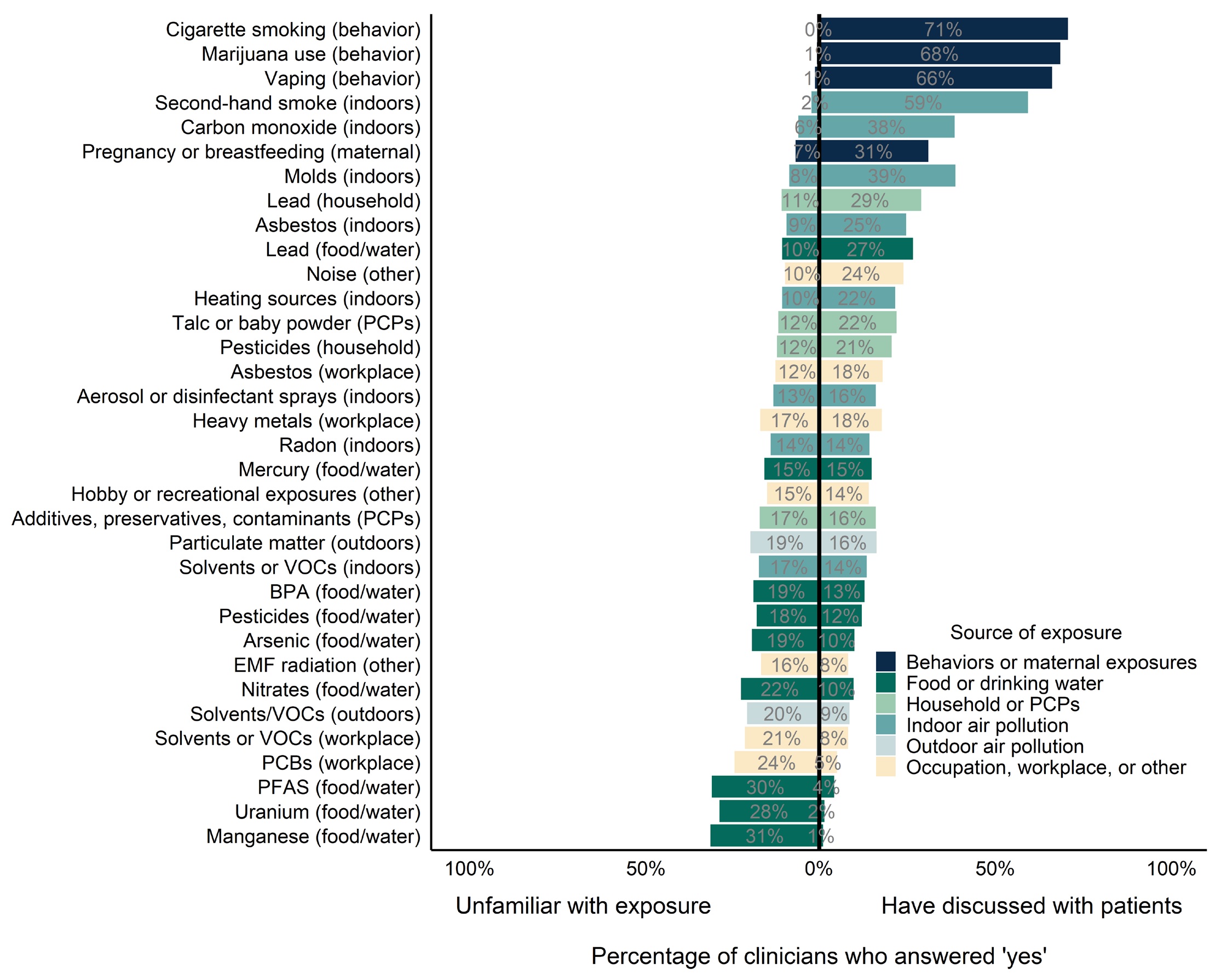 The exposures are ranked by the ratio of “have discussed” to “unfamiliar.” VOCs = volatile organic compounds; BPA = bisphenol A; EMF = electromagnetic fields; PCBs = polychlorinated biphenyls; PFAS = per- and polyfluorinated substances
The exposures are ranked by the ratio of “have discussed” to “unfamiliar.” VOCs = volatile organic compounds; BPA = bisphenol A; EMF = electromagnetic fields; PCBs = polychlorinated biphenyls; PFAS = per- and polyfluorinated substances
Objective: Assess educational interest and awareness of EH among actively practicing health care providers, and evaluate current preferences for consuming EH-related educational content.
Design/Methods: A 35-item instrument covering EH issues was created, pretested to ensure items were clearly articulated and response items were relevant, and modified. The finalized Internet-based survey was sent during January-April 2021 to a convenience sample of Massachusetts health care providers, of whom 362 returned completed surveys. Of these, 20% self-identified as pediatric or family practice care providers, respectively; 72% of respondents were nurses and/or nurse practitioners.
Results: Although clinicians recognized the importance of environmental exposures and their health impacts, 34% had not asked patients about such exposures in the previous year; only 7% endorsed receiving any previous training on how to counsel patients on environmental exposures. Health care professionals cited time pressure and limited knowledge as the top barriers to such discussions. While they felt knowledgeable when counseling on personal behavior exposures (e.g. smoking, vaping, or marijuana use), the safety of food and water from contamination by chemicals (e.g. perfluoroalkyl substances, metals) were among the least familiar and least discussed topics. (Figure 1) Other knowledge gaps included pesticides, indoor air pollutants, and hazards posed by household and personal care products. For those who sought out EH-related resources, 60% consulted government websites, 51% proprietary medical information websites, 49% professional literature, 46% professional society position statements, and 37% state/local health department resources. Clinicians preferred tip sheets, on-demand or pre-recorded materials, and online toolkits rather than live (in-person or virtual) trainings. Conclusion(s): These results can inform future plans for educational outreach to health care professionals regarding EH topics important to discuss during primary care.
Figure 1. Percentage of clinicians discussing versus unfamiliar with specific exposures
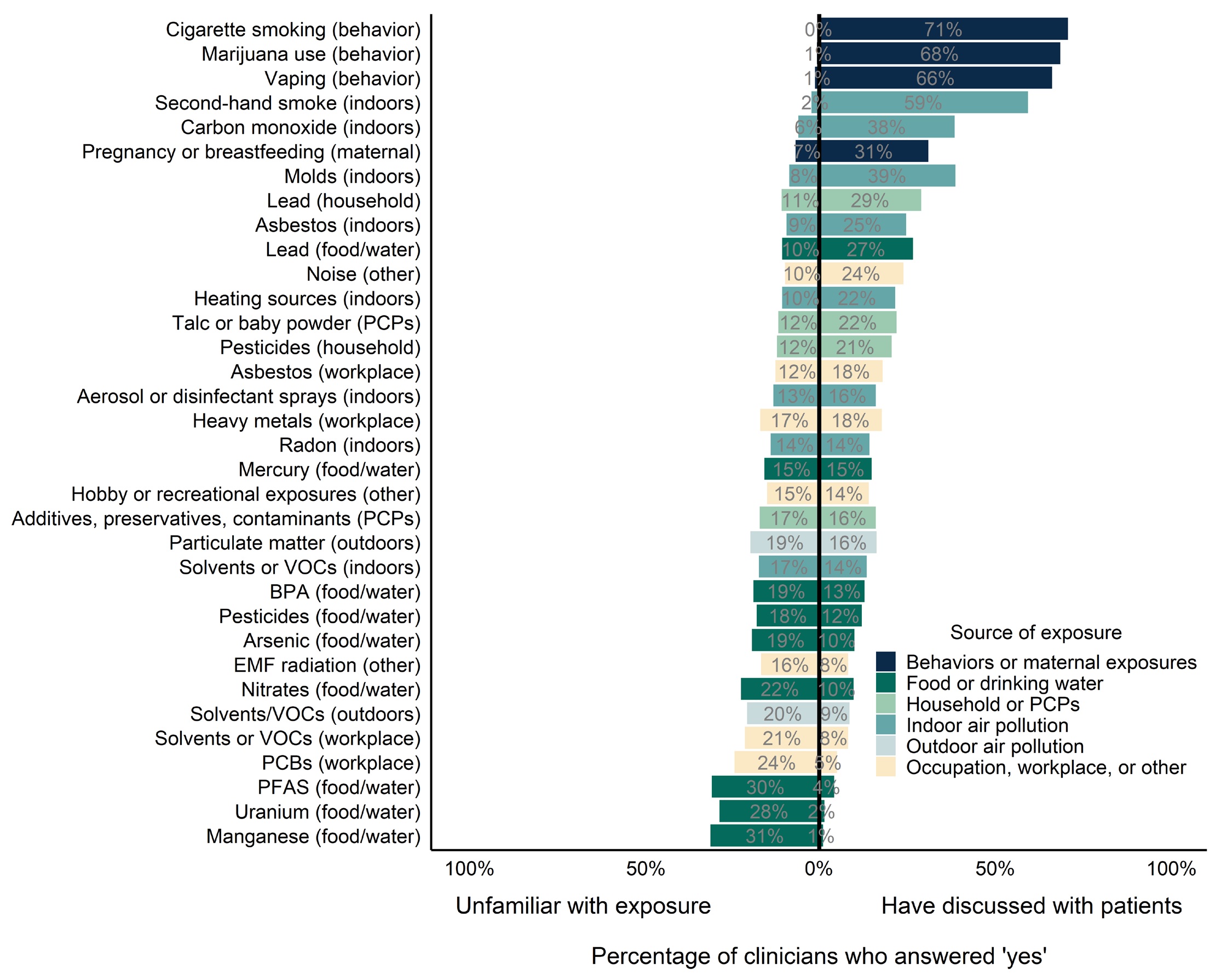 The exposures are ranked by the ratio of “have discussed” to “unfamiliar.” VOCs = volatile organic compounds; BPA = bisphenol A; EMF = electromagnetic fields; PCBs = polychlorinated biphenyls; PFAS = per- and polyfluorinated substances
The exposures are ranked by the ratio of “have discussed” to “unfamiliar.” VOCs = volatile organic compounds; BPA = bisphenol A; EMF = electromagnetic fields; PCBs = polychlorinated biphenyls; PFAS = per- and polyfluorinated substances