Adolescent Medicine: Disordered Eating
Category: Abstract Submission
Adolescent Medicine III
206 - The Effects of the COVID-19 Pandemic on Pediatric Hospitalizations for Eating Disorders
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 206
Publication Number: 206.400
Publication Number: 206.400
May Shum, Yale School of Medicine, New Haven, CT, United States; Rebecca C. Kamody, Yale School of Medicine, New Haven, CT, United States; Claudia Moreno, Yale Child Study Center/Yale New Haven Hospital, Woodbridge, CT, United States; Sarah McCollum, Yale University School of Medicine, Department of Pediatrics, New Haven, CT, United States; Veronika Shabanova, Yale School of Medicine, New Haven, CT, United States; Jaspreet Loyal, Yale School of Medicine, New Haven, CT, United States

May Shum, BA (she/her/hers)
Medical Student
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Eating disorders (EDs) are common among adolescents and often require hospital admission for nutritional restoration. Throughout the COVID-19 pandemic, there has been a notable increase in the volume of hospital admissions for adolescents with EDs, potentially due to interruptions in medical care and increased psychological distress. However, there is a paucity of information on how this increase has affected hospitalization courses and disposition planning following discharge. It is important to evaluate the evolving needs of ED patients during the pandemic to understand changing burdens on hospital resources.
Objective: Our aim was to quantitively describe the changes in hospitalizations for EDs at our institution prior to and during the COVID-19 pandemic.
Design/Methods: We reviewed the charts of patients with EDs admitted to our academic medical center in the Northeastern US for nutritional restoration from January 1, 2017, to June 30, 2021. We report differences in patient characteristics, hospital course, length of stay (LOS), and disposition pre-pandemic (2017-2019) and during the pandemic (2020-2021).
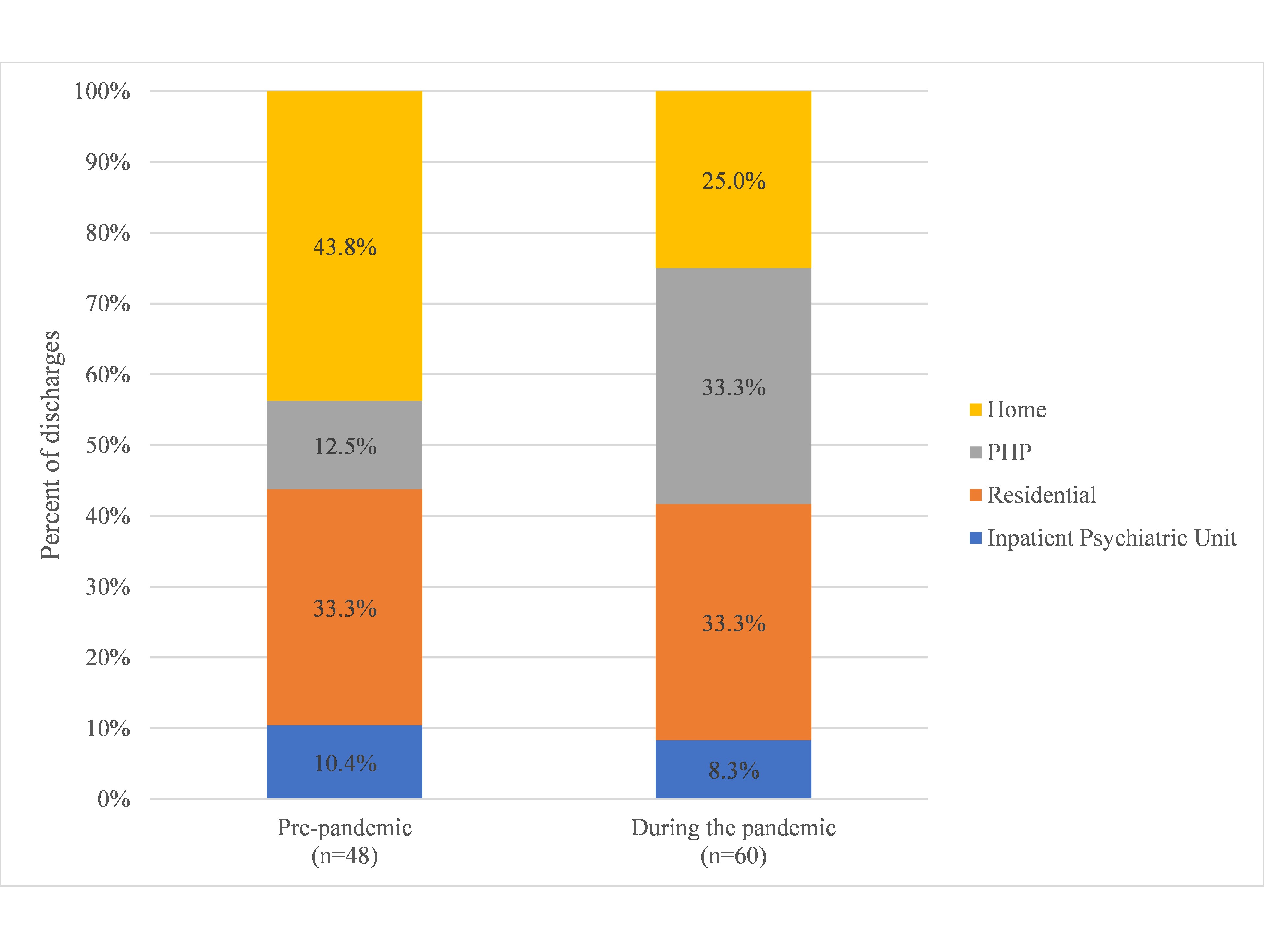
Results: We reviewed charts for 85 patients totaling 108 hospital admissions. The rate of monthly admissions for nutritional restoration prior to compared with during the pandemic increased from 1.3 to 3.3 admissions per month (p < 0.001). Most patients were female (90.6%), white (78.8%), had private insurance (80.0%) and had restrictive eating behaviors (97.2%). Significant differences when comparing pre- vs. during the pandemic included (1) an increase in the average LOS (12.8 days vs. 17.3 days, p=0.04) with younger age ( < 13 years of age) being associated with longer LOS (p < 0.001); (2) a greater proportion of patients for whom psychotropic medications were initiated or changed (12.5% vs. 28.3% p=0.04); and (3) a greater proportion of patients who were discharged to partial hospitalization, residential, or inpatient psychiatric treatment instead of home with outpatient therapy (56.2% vs.75.0%, p=0.04).Conclusion(s): In addition to an increase in the number of admissions for ED management during the pandemic, our study suggests an increase in severity of these admissions, as represented by longer admissions for younger children, increased need for psychotropic medication management, and higher levels of care after discharge. These increased demands have implications on allocations of hospital resources and represent areas where appropriate adaptations may improve the quality of care for ED patients.
APA Student Research Award CVSHUM_PAS CV 2021.pdf
Figure 2. Dispositions after discharge pre- and during the COVID-19 pandemic (2017-2019 vs 2020-2021, p=0.04).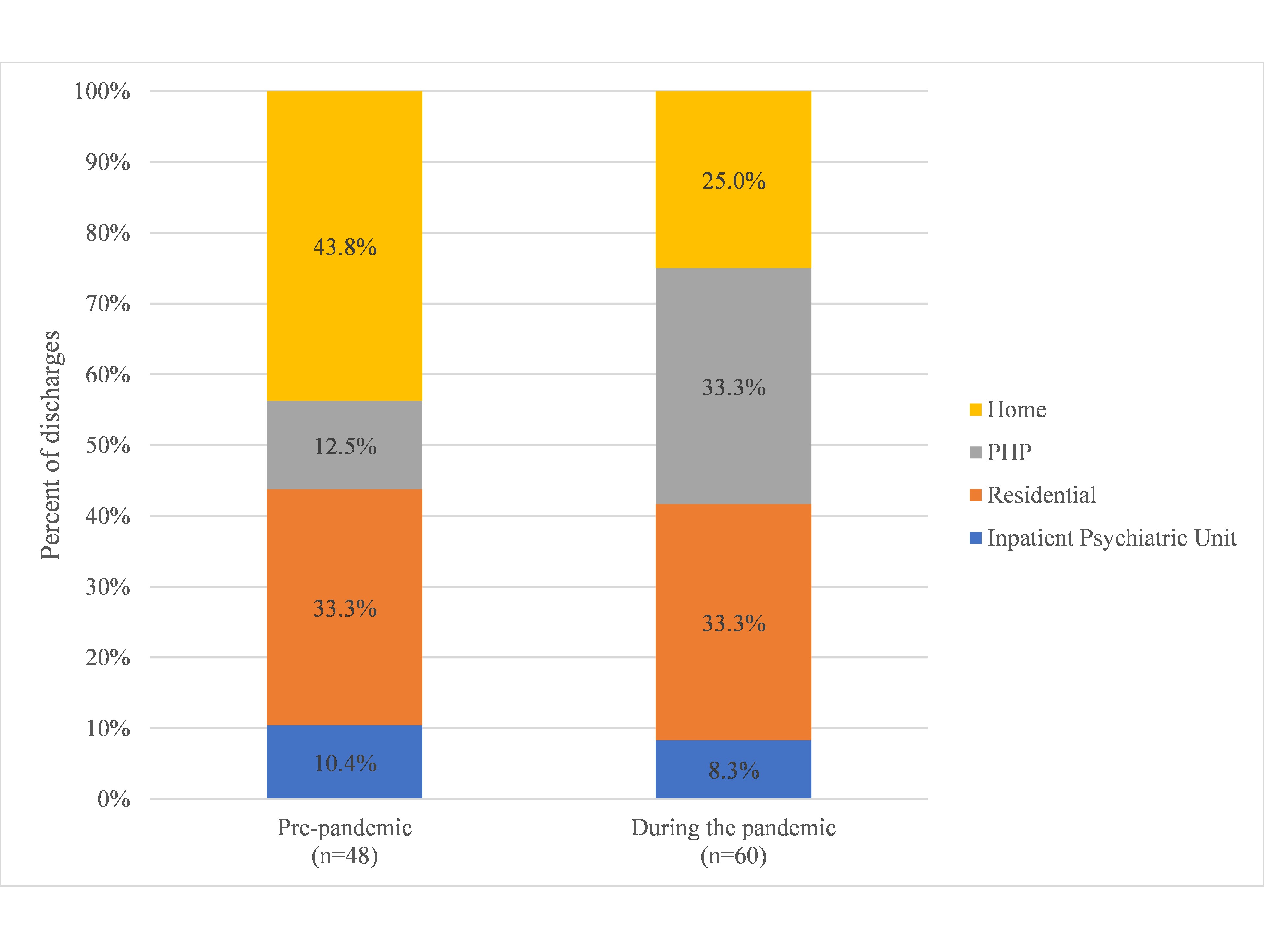
Objective: Our aim was to quantitively describe the changes in hospitalizations for EDs at our institution prior to and during the COVID-19 pandemic.
Design/Methods: We reviewed the charts of patients with EDs admitted to our academic medical center in the Northeastern US for nutritional restoration from January 1, 2017, to June 30, 2021. We report differences in patient characteristics, hospital course, length of stay (LOS), and disposition pre-pandemic (2017-2019) and during the pandemic (2020-2021).
Results: We reviewed charts for 85 patients totaling 108 hospital admissions. The rate of monthly admissions for nutritional restoration prior to compared with during the pandemic increased from 1.3 to 3.3 admissions per month (p < 0.001). Most patients were female (90.6%), white (78.8%), had private insurance (80.0%) and had restrictive eating behaviors (97.2%). Significant differences when comparing pre- vs. during the pandemic included (1) an increase in the average LOS (12.8 days vs. 17.3 days, p=0.04) with younger age ( < 13 years of age) being associated with longer LOS (p < 0.001); (2) a greater proportion of patients for whom psychotropic medications were initiated or changed (12.5% vs. 28.3% p=0.04); and (3) a greater proportion of patients who were discharged to partial hospitalization, residential, or inpatient psychiatric treatment instead of home with outpatient therapy (56.2% vs.75.0%, p=0.04).Conclusion(s): In addition to an increase in the number of admissions for ED management during the pandemic, our study suggests an increase in severity of these admissions, as represented by longer admissions for younger children, increased need for psychotropic medication management, and higher levels of care after discharge. These increased demands have implications on allocations of hospital resources and represent areas where appropriate adaptations may improve the quality of care for ED patients.
APA Student Research Award CVSHUM_PAS CV 2021.pdf
Figure 2. Dispositions after discharge pre- and during the COVID-19 pandemic (2017-2019 vs 2020-2021, p=0.04).