Infectious Diseases
Category: Abstract Submission
Infectious Diseases: Bacteria & Antimicrobials
295 - Clinical characteristics of pediatric patients with E.Coli O157:H7 or Shiga 1 or 2 toxin diarrhea with subsequent development of hemolytic uremic syndrome
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 295
Publication Number: 295.114
Publication Number: 295.114
Lydia Maleknia, Kaiser Permanente - Oakland Medical Center, Oakland, CA, United States; Zahra Samiezade-Yazd, Kaiser Permanente Division of Research, Oakland, CA, United States; Xing Wang, Kaiser Permanente - Oakland Medical Center, Berkeley, CA, United States; Miranda Ritterman Weintraub, Kaiser Permanente - Oakland Medical Center, Oakland, CA, United States; Tara Greenhow, Kaiser Permanente San Francisco, San Francisco, CA, United States

Lydia Maleknia, MD
Pediatric Hospitalist Fellow
Kaiser Permanente - Oakland Medical Center
Oakland, California, United States
Presenting Author(s)
Background: Hemolytic uremic syndrome (HUS) is a serious complication of Shiga toxin-producing Escherichia coli (STEC) diarrhea. Real-time polymerase chain reaction (RT-PCR) panels can detect the presence of serotype O157:H7, Shiga toxin (Stx) 1 and 2. Given the variability in HUS onset in patients with STEC, there is a gap in the literature on guidelines for clinical monitoring to detect HUS in a timely manner.
Objective: To assess clinical predictors, timing, and outcomes of children who test positive for STEC and develop HUS.
Design/Methods: This is a retrospective cohort study of children aged 0-17 years who were hospitalized with HUS between March 1, 2015 and February 28, 2020 within Kaiser Permanente Northern California. STEC RT-PCR results, HUS diagnoses, and other data were obtained from database extraction and chart review. We assessed STEC RT-PCR results, the number of clinical encounters prior to diagnosis, reason for hospital admission, and clinical outcomes.
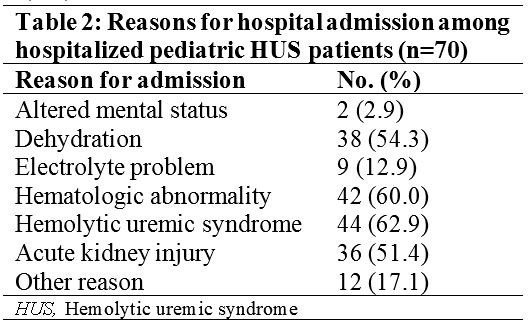
Results: There were 1,041 children with STEC infection and 70 (median age 3.9 years, 46% female) hospitalized with STEC-associated HUS. The most common STEC RT-PCR result was E.Coli O157:H7 with Stx2 (57%), and Stx2 was seen in 76% of all cases compared to 10% for Stx1 (Table 1). The median number of encounters prior to hospitalization was 2 (range: 0-9) and median time from symptom onset to hospitalization was 5 days (range: 0-10). STEC was detected up to 12 days prior to admission. Most children (63%) had definitive HUS at the time of admission. Other common indications for admission were hematologic abnormality, acute kidney injury, and dehydration (Table 2). Of the 70 hospitalized patients, 31 (44%) required intensive care, 20 (29%) required dialysis, 66 (94%) were discharged home and 2 (3%) died (Table 3). The median length of stay was 9 days (range: 6-16). The most common neurologic complication was altered mental status (13%), followed by seizure (7%), confusion (4%), stroke (3%) and delirium (1%).Conclusion(s): Most patients with STEC-associated HUS were E.Coli O157:H7 and Stx2 positive. Only two thirds of the patients met HUS criteria at the time of admission, demonstrating the need to stay vigilant for complications in patients with STEC diarrhea, especially if Stx2 is detected. Further analysis is needed to determine how Stx status may predict clinical trajectory or outcomes among those with STEC-induced HUS and the ideal timing of monitoring for patients with STEC diarrhea to detect HUS.
Lydia Maleknia Curriculum VitaeCV 2021.pdf
Table 2: Reasons for hospital admission among hospitalized pediatric HUS patients (n=70)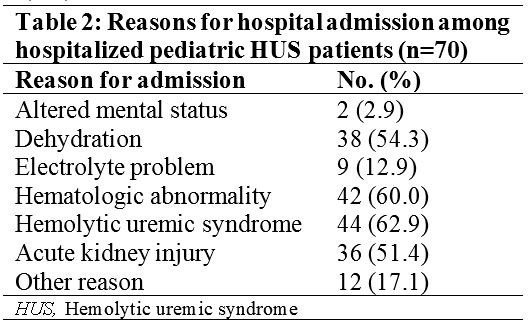
Objective: To assess clinical predictors, timing, and outcomes of children who test positive for STEC and develop HUS.
Design/Methods: This is a retrospective cohort study of children aged 0-17 years who were hospitalized with HUS between March 1, 2015 and February 28, 2020 within Kaiser Permanente Northern California. STEC RT-PCR results, HUS diagnoses, and other data were obtained from database extraction and chart review. We assessed STEC RT-PCR results, the number of clinical encounters prior to diagnosis, reason for hospital admission, and clinical outcomes.
Results: There were 1,041 children with STEC infection and 70 (median age 3.9 years, 46% female) hospitalized with STEC-associated HUS. The most common STEC RT-PCR result was E.Coli O157:H7 with Stx2 (57%), and Stx2 was seen in 76% of all cases compared to 10% for Stx1 (Table 1). The median number of encounters prior to hospitalization was 2 (range: 0-9) and median time from symptom onset to hospitalization was 5 days (range: 0-10). STEC was detected up to 12 days prior to admission. Most children (63%) had definitive HUS at the time of admission. Other common indications for admission were hematologic abnormality, acute kidney injury, and dehydration (Table 2). Of the 70 hospitalized patients, 31 (44%) required intensive care, 20 (29%) required dialysis, 66 (94%) were discharged home and 2 (3%) died (Table 3). The median length of stay was 9 days (range: 6-16). The most common neurologic complication was altered mental status (13%), followed by seizure (7%), confusion (4%), stroke (3%) and delirium (1%).Conclusion(s): Most patients with STEC-associated HUS were E.Coli O157:H7 and Stx2 positive. Only two thirds of the patients met HUS criteria at the time of admission, demonstrating the need to stay vigilant for complications in patients with STEC diarrhea, especially if Stx2 is detected. Further analysis is needed to determine how Stx status may predict clinical trajectory or outcomes among those with STEC-induced HUS and the ideal timing of monitoring for patients with STEC diarrhea to detect HUS.
Lydia Maleknia Curriculum VitaeCV 2021.pdf
Table 2: Reasons for hospital admission among hospitalized pediatric HUS patients (n=70)